Avascular Necrosis (AVN) of the knee, also known as osteonecrosis, is a condition where bone tissue dies due to a lack of blood supply. While AVN commonly affects the hip, it can also involve the knee joint. Left untreated, it can lead to joint collapse and severe pain, requiring surgical intervention, including knee replacement in advanced stages. Understanding the causes, symptoms, and management strategies of knee AVN is crucial for effective treatment.
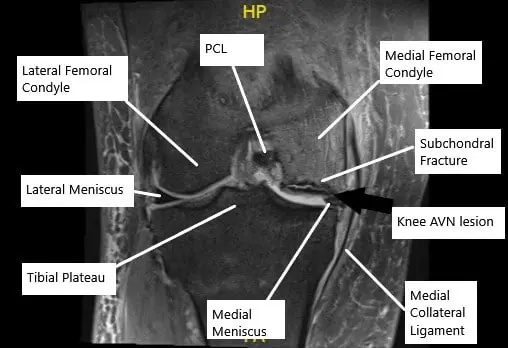
MRI of the knee in the coronal section showing AVN lesion along with subchondral fracture in the medial femoral condyle.
How Common It Is and Who Gets It? (Epidemiology)
AVN of the knee is relatively rare compared to hip AVN but can affect individuals across various age groups. It is more common in people who have a history of knee trauma, certain medical conditions like systemic lupus erythematosus, or those who have undergone long-term steroid treatment. Risk factors such as heavy alcohol consumption and diseases like Gaucher’s disease also increase the likelihood of developing knee AVN.
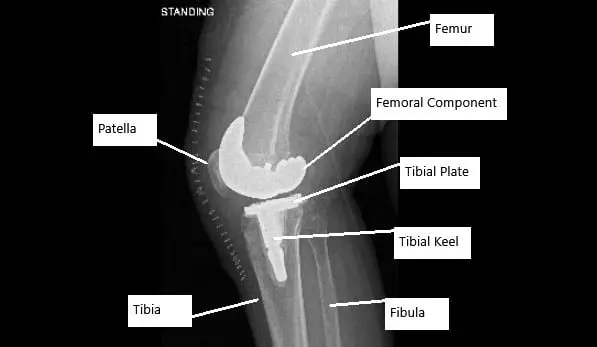
X-ray showing total knee replacement surgery in a patient with AVN knee.
Why It Happens – Causes (Etiology and Pathophysiology)
The primary cause of AVN is the disruption of blood supply to the bone, leading to bone death (infarction). In the knee, AVN often affects the medial femoral condyle, which is the inner part of the thigh bone. The lack of blood flow prevents the bone from receiving essential nutrients and oxygen, causing the bone tissue to die and potentially collapse. While many cases of knee AVN are idiopathic (no known cause), risk factors include:
- Alcohol abuse: Excessive alcohol consumption increases free fatty acids in the bloodstream, which can block blood vessels supplying the bone.
- Corticosteroid use: Long-term steroid use, often for conditions like rheumatoid arthritis or asthma, increases marrow pressure and may lead to AVN.
- Trauma or injury: Knee injuries from falls, accidents, or surgeries can disrupt blood flow, increasing the risk of AVN.
- Underlying diseases: Conditions such as thalassemia, Gaucher’s disease, and kidney transplant recipients are at higher risk.
How the Body Part Normally Works? (Relevant Anatomy)
The knee joint is the largest weight-bearing joint in the body, consisting of the femur (thigh bone), tibia (shin bone), and patella (kneecap). The ends of these bones are covered by articular cartilage, and just beneath it lies the subchondral bone. AVN affects this subchondral bone, often starting in the medial femoral condyle, and can lead to joint collapse if untreated.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of knee AVN can vary depending on the stage of the disease. Early on, symptoms may be mild or asymptomatic, but as the condition progresses, patients may experience:
- Pain: Pain is usually felt in the inner part of the knee and may start suddenly or gradually. It worsens with weight-bearing activities or during rest in advanced stages.
- Swelling: The knee may become swollen, especially after physical activity.
- Decreased Range of Motion: The knee may become stiff, making it difficult to fully extend or bend the joint.
- Instability: In severe cases, patients may feel as though their knee is unstable or “giving way.”
- Limping: Chronic pain and instability may cause individuals to walk with a limp.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a thorough physical examination, where the doctor checks for knee swelling, tenderness, and restricted movement. Early AVN may not show clear findings on plain X-rays, so further imaging tests are often required:
- MRI: MRI is the most sensitive tool for diagnosing AVN, revealing changes in bone structure, subchondral fractures, and early signs of bone death.
- X-ray: X-rays are used to monitor the progression of AVN and may show bone collapse and joint space narrowing in later stages.
- Bone Scan: This can be used to detect areas of abnormal bone activity, especially in the early stages.
Classification
AVN of the knee is classified into stages based on the progression of the disease:
- Stage 1: Early, asymptomatic stage. The bone appears normal on X-ray but may show subtle changes on MRI.
- Stage 2: The subchondral bone begins to collapse, and patients experience significant pain. MRI confirms bone damage.
- Stage 3: The joint surface collapses, and osteoarthritis begins to develop. X-rays show significant joint changes.
- Stage 4: Severe osteoarthritis with significant joint destruction. The knee’s range of motion is severely limited, and total knee replacement may be necessary.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions such as meniscal tears, osteoarthritis, and knee ligament injuries can cause symptoms similar to knee AVN, including pain, swelling, and decreased function. A thorough examination and imaging studies are necessary to differentiate between these conditions.
Treatment Options
Non-Surgical Care
- Stage 1: In the early stages, protected weight-bearing with crutches, a cane, or a knee brace is recommended. Medications such as NSAIDs and bisphosphonates may help manage pain and slow the disease’s progression.
- Stage 2: Core decompression, where small holes are drilled in the affected area to reduce marrow pressure and increase blood flow, can be effective. Bone and cartilage transplants or autologous chondrocyte implantation may be considered.
- Stage 3 & 4: In advanced stages, total knee replacement (TKR) surgery is the most effective treatment, providing relief from pain and restoring knee function.
Surgical Care
- Core Decompression: This procedure involves drilling small holes into the affected bone to relieve pressure and promote blood flow.
- Bone Grafting: Grafts may be used to repair the damaged area of the bone.
- Total Knee Replacement: In severe cases, when the joint is extensively damaged, knee replacement surgery may be required. This procedure involves removing the damaged bone and cartilage and replacing them with artificial components.
Recovery and What to Expect After Treatment
Rehabilitation plays a critical role in recovery, particularly after surgery. For conservative treatments, physical therapy focuses on improving range of motion and strengthening the muscles around the knee. After total knee replacement, patients will follow a rehabilitation plan to restore knee function, with most individuals regaining normal activity levels within 3 to 6 months.
Possible Risks or Side Effects (Complications)
- Infection: As with any surgery, infection is a potential risk.
- Blood Clots: Post-surgical patients may be at risk for deep vein thrombosis (DVT).
- Graft Failure: In some cases, grafts used in bone repair may fail to integrate or function as expected.
- Recurrent Pain: After total knee replacement, there may be some residual pain or discomfort as the body adjusts to the prosthetic joint.
Long-Term Outlook (Prognosis)
The prognosis for knee AVN depends on the stage at which it is diagnosed. Early intervention with non-surgical methods may prevent the progression to advanced stages. In severe cases, knee replacement can significantly improve quality of life, though long-term outcomes will depend on factors like the patient’s age, activity level, and the success of rehabilitation.
Out-of-Pocket Costs
Medicare
CPT Code 20902 – Bone Grafting (Harvest and Placement of Bone Graft): $63.66
CPT Code 27125 – Hip Replacement (Partial Hip Arthroplasty): $268.14
CPT Code 27130 – Hip Replacement (Total Hip Arthroplasty): $303.45
CPT Code 38220 – Bone Marrow Injection (Aspiration for Bone Marrow Concentrate Therapy): $36.05
Under Medicare, 80% of the approved amount for these procedures is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—usually cover this 20%, leaving most patients with little to no out-of-pocket expenses for Medicare-approved bone grafting, hip replacement, and bone marrow injection procedures. These supplemental plans coordinate directly with Medicare to provide full coverage for the procedures.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it functions as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or any uncovered charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on the specific policy and network status.
Workers’ Compensation
If your bone grafting, hip replacement, or bone marrow injection is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your injury requiring these procedures is the result of a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses, including bone grafting, hip replacement, and bone marrow injections. The only possible out-of-pocket cost may be a small deductible depending on your individual policy terms.
Example
David, a 60-year-old patient with severe hip arthritis, underwent total hip arthroplasty (CPT 27130) and also received bone marrow concentrate therapy (CPT 38220) for joint regeneration. His estimated Medicare out-of-pocket costs were $303.45 for the hip replacement and $36.05 for the bone marrow injection. Since David had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for the procedures.
Frequently Asked Questions (FAQ)
Q. What causes knee AVN?
A. Knee AVN is caused by a disruption in the blood supply to the bone, which can result from trauma, long-term steroid use, alcohol consumption, or underlying diseases.
Q. How is knee AVN diagnosed?
A. Knee AVN is diagnosed using a combination of physical examination, X-rays, MRI, and bone scans to assess the degree of bone damage.
Q. What are the treatment options for knee AVN?
A. Treatment options range from non-surgical methods, such as weight-bearing protection and medications, to surgical interventions, including core decompression and total knee replacement.
Q. Can knee AVN be prevented?
A. While not all cases of knee AVN can be prevented, reducing alcohol consumption, managing underlying health conditions, and preventing knee injuries can help lower the risk.
Summary and Takeaway
Avascular necrosis of the knee is a serious condition that can lead to joint collapse if left untreated. Early diagnosis and management are key to preventing the progression of the disease. Non-surgical treatments may help in the early stages, but surgery, including total knee replacement, may be necessary in advanced cases. By following a proper treatment plan and rehabilitation, individuals with knee AVN can regain function and improve their quality of life.
Clinical Insight & Recent Findings
Avascular necrosis (AVN) is a serious condition that affects the femoral head, leading to the potential need for total hip arthroplasty (THA). While THA is a common and effective treatment, it may not be ideal for younger, more active patients due to the risk of needing revision surgeries later in life.
A recent systematic review highlighted the role of orthobiologic therapies, such as bone marrow aspirate concentrate (BMAC), in delaying the need for hip replacement surgery. The study found that BMAC, in particular, significantly improved long-term survival without the need for THA, providing a promising alternative for managing AVN.
These findings suggest that early intervention with orthobiologics could help preserve the natural hip joint and delay more invasive procedures like THA. (“Study on orthobiologic therapies delaying hip replacement surgery in AVN – see PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons specializing in joint preservation, sports medicine, and knee surgery are typically involved in the diagnosis and treatment of knee AVN. Physical therapists play a crucial role in rehabilitation after treatment.
When to See a Specialist?
You should consult a specialist if you experience persistent knee pain, swelling, or limited movement, especially after an injury or long-term steroid use.
When to Go to the Emergency Room?
Seek emergency care if you experience sudden, severe knee pain, a noticeable shift in knee alignment, or signs of infection following surgery, such as increased redness or fever.
What Recovery Really Looks Like?
Recovery from knee AVN treatment, especially surgery, requires a structured rehabilitation program to regain strength and mobility. Full recovery, particularly after knee replacement, may take several months.
What Happens If You Ignore It?
Ignoring knee AVN can lead to severe joint damage, chronic pain, and loss of function. Timely treatment is essential to preserve knee health and prevent the need for extensive surgery.
How to Prevent It?
Prevention involves managing underlying health conditions, avoiding excessive alcohol consumption, and protecting the knees from injury through proper technique and protective gear.
Nutrition and Bone or Joint Health
Adequate nutrition, including calcium and vitamin D, is essential for bone health, especially for individuals at risk for AVN. Maintaining a healthy weight and staying active can also help reduce the risk of joint damage.
Activity and Lifestyle Modifications
Engaging in low-impact activities, such as swimming or cycling, can help maintain joint function without putting excessive strain on the knee.
Do you have more questions?
How common is Avascular Necrosis (AVN) of the knee?
AVN of the knee is relatively rare compared to other knee conditions, but its prevalence can vary depending on factors such as age, underlying medical conditions, and lifestyle factors.
Can AVN affect both knees simultaneously?
Yes, AVN can affect both knees simultaneously, although it is less common than unilateral (one-sided) involvement.
Is AVN of the knee more common in men or women?
AVN of the knee can affect both men and women, but certain underlying conditions or risk factors may predispose one gender more than the other.
How long does it take for AVN of the knee to progress?
The progression of AVN can vary from person to person and depends on factors such as the underlying cause, the stage of the condition, and how well it responds to treatment. In some cases, AVN may progress slowly over months or years, while in others, it may progress more rapidly.
Can AVN of the knee be cured completely?
Unfortunately, there is no cure for AVN of the knee. However, with proper treatment and management, symptoms can be alleviated, and the progression of the disease can be slowed down.
What are the long-term complications of untreated AVN of the knee?
Untreated AVN of the knee can lead to significant pain, joint deformity, and loss of function. In severe cases, it may result in the need for total knee replacement surgery.
Are there any alternative or complementary therapies that can help manage AVN of the knee?
Some people may explore alternative or complementary therapies such as acupuncture, herbal supplements, or chiropractic care to help manage symptoms of AVN. However, it’s essential to discuss these options with your healthcare provider to ensure they are safe and effective.
Can AVN of the knee recur after treatment?
While treatment for AVN can help alleviate symptoms and slow down the progression of the disease, there is a risk of recurrence, especially if the underlying cause is not addressed or if there is continued stress on the affected knee joint.
What lifestyle modifications can help manage AVN of the knee?
Lifestyle modifications such as maintaining a healthy weight, avoiding excessive alcohol consumption, quitting smoking, and engaging in low-impact exercise can help manage symptoms and improve overall knee health.
Are there any dietary changes that can help prevent or manage AVN of the knee?
While there is no specific diet that can prevent or cure AVN of the knee, maintaining a balanced diet rich in fruits, vegetables, lean proteins, and whole grains can support overall bone and joint health.
How does AVN of the knee affect daily activities and quality of life?
AVN of the knee can significantly impact daily activities and quality of life, leading to pain, stiffness, difficulty walking, and limitations in mobility. It’s essential to work closely with your healthcare team to develop strategies to manage these challenges effectively.
Can AVN of the knee lead to other complications or secondary conditions?
In some cases, AVN of the knee can lead to secondary complications such as osteoarthritis, joint instability, or bone fractures. These complications may require additional treatment and management.
What is the success rate of surgical treatment options for AVN of the knee?
The success rate of surgical treatment options for AVN of the knee can vary depending on factors such as the stage of the condition, the patient’s overall health, and the surgeon’s experience. However, many patients experience significant improvement in symptoms and function following surgery.
Are there any experimental treatments or clinical trials available for AVN of the knee?
Researchers are continually exploring new treatment options for AVN of the knee, including stem cell therapy, gene therapy, and biologic agents. Participation in clinical trials may be an option for some patients, but it’s essential to discuss these options with your healthcare provider.
How long does it take to recover from surgery for AVN of the knee?
The recovery time from surgery for AVN of the knee can vary depending on the type of procedure performed, the patient’s overall health, and other factors. In general, rehabilitation and recovery may take several months, with gradual improvement in symptoms and function over time.
Are there any support groups or resources available for people with AVN of the knee?
Yes, there are several online support groups, forums, and resources available for people with AVN of the knee. Connecting with others who are going through similar experiences can provide valuable support, information, and encouragement.
Can AVN of the knee be prevented in people at risk?
While it may not be possible to prevent AVN entirely, certain measures can help reduce the risk, such as avoiding excessive alcohol consumption, managing underlying medical conditions, and taking precautions to prevent knee injuries.
How often should follow-up appointments be scheduled after treatment for AVN of the knee?
Follow-up appointments after treatment for AVN of the knee may vary depending on factors such as the type of treatment received, the stage of the condition, and the patient’s overall health. Your healthcare provider will typically schedule follow-up appointments as needed to monitor your progress and adjust your treatment plan accordingly.
Can AVN of the knee affect children or adolescents?
Yes, AVN of the knee can affect individuals of any age, including children and adolescents. In younger patients, AVN may be related to factors such as trauma, infection, or certain medical conditions.
How does AVN of the knee differ from other knee conditions such as osteoarthritis or rheumatoid arthritis?
While AVN of the knee involves the death of bone tissue due to a lack of blood supply, osteoarthritis and rheumatoid arthritis are inflammatory conditions that affect the joints differently. Osteoarthritis is characterized by the breakdown of cartilage in the joints, while rheumatoid arthritis is an autoimmune disorder that causes inflammation and damage to the joints.
Are there any specific exercises or physical activities that should be avoided with AVN of the knee?
It’s essential to consult with your healthcare provider or physical therapist before starting any new exercise or physical activity regimen with AVN of the knee. In general, high-impact activities or exercises that put excessive stress on the knee joint should be avoided, while low-impact exercises that promote strength, flexibility, and range of motion may be beneficial.
What are the potential complications of surgery for AVN of the knee?
Like any surgical procedure, surgery for AVN of the knee carries risks, including infection, blood clots, damage to surrounding tissues, and complications related to anesthesia. Your surgeon will discuss these risks with you in detail before the procedure and take steps to minimize them during and after surgery.
Can AVN of the knee affect other joints in the body?
While AVN most commonly affects the knee joint, it can also occur in other joints such as the hip, shoulder, ankle, or wrist. The underlying causes and risk factors for AVN may vary depending on the affected joint.

