Medial patellofemoral ligament reconstruction is a surgical treatment used to correct kneecap instability. This procedure is offered when the ligament on the inner side of the knee is torn and no longer able to keep the kneecap centered. When this ligament is damaged, the kneecap may slide out of place, causing pain, swelling, and repeated dislocations. The goal of surgery is to restore stability so the knee can bend and straighten smoothly without the kneecap slipping.
How Common It Is and Who Gets It? (Epidemiology)
This surgery is most often recommended for people who suffer repeated kneecap dislocations. It is common in young, active individuals and athletes, though it can affect people of any age. It may also be needed in people with naturally loose joints or alignment issues that make the kneecap more likely to slip.
Why It Happens – Causes (Etiology and Pathophysiology)
The medial patellofemoral ligament helps guide the kneecap as the knee bends. A strong impact, fall, or sudden twisting motion can tear this ligament. Some people are more prone to this injury due to loose joints, unusual bone alignment, or tight tissues on the outer side of the knee. When the ligament heals in a stretched or loose way, the kneecap becomes unstable and may dislocate repeatedly.
Direct Trauma: A significant blow or impact to the knee, such as a fall or collision during sports activities, can result in MPFL injury. This trauma may cause stretching or tearing of the ligament.
Repetitive Stress: Activities that involve repetitive bending, twisting, or sudden changes in direction can put excessive stress on the MPFL, leading to gradual wear and tear over time. This is particularly common in athletes who participate in sports like basketball, soccer, or volleyball.
Genetic Factors: Some individuals may have an inherent predisposition to ligament laxity or abnormalities in the alignment of the patella and femur, increasing their risk of MPFL injury.
Muscular Imbalance: Weakness or imbalance in the muscles surrounding the knee, especially the quadriceps and hamstrings, can disrupt the normal function of the MPFL and contribute to its injury.
Besides traumatic injuries or athletic injuries, some patients may be prone to kneecap dislocation owing to the increased laxity in their joints and ligaments, or due to tight structures (patellar retinaculum) on the outer side of the knee joint.
The torn ligament may heal naturally but usually heals in a slack manner causing instability of the kneecap. This may result in recurrent instability further aggravating the condition. Further, over time, the cartilage forming the patellofemoral joint may wear out leading to arthritis and degenerative changes.
How the Body Part Normally Works? (Relevant Anatomy)
The kneecap sits in a small groove at the front of the thigh bone. As the knee bends, the kneecap moves up and down this groove. The medial patellofemoral ligament, located on the inner side of the knee, acts like a strap to prevent the kneecap from drifting outward. When this ligament is torn, the kneecap can shift out of place.
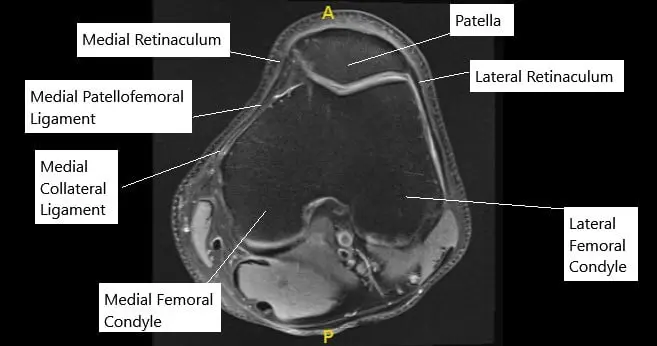
MRI of the knee in axial section showing normal MPFL.
What You Might Feel – Symptoms (Clinical Presentation)
Medial Patellofemoral Ligament (MPFL) injury typically presents with several distinctive symptoms that can vary in intensity depending on the severity of the injury. The MPFL is a crucial ligament that stabilizes the patella (kneecap) and prevents it from dislocating towards the outer side of the knee. When this ligament is injured, it can lead to significant discomfort and functional limitations. Here are the common symptoms associated with MPFL injury:
Pain: Pain is usually the first symptom experienced with an MPFL injury. It can be localized to the inner side of the knee or around the patella. The pain may range from mild to severe and can be aggravated by activities that involve bending or straightening the knee, such as walking, running, or climbing stairs.
Swelling: Swelling around the patella or throughout the knee joint is another typical symptom of MPFL injury. The swelling may develop rapidly after the injury or gradually over time and can contribute to stiffness and limited range of motion in the knee.
Instability or Feeling of Giving Way: Since the MPFL plays a crucial role in stabilizing the patella, its injury can lead to a sense of instability in the knee. Patients may describe a feeling of the knee “giving way” or feeling as though it might dislocate, especially during activities that require sudden changes in direction or weight-bearing.
Difficulty Straightening the Knee: In some cases, individuals with an MPFL injury may experience difficulty fully straightening the affected knee. This limitation in extension, also known as knee flexion contracture, can further contribute to functional impairment and discomfort.
Audible Popping or Clicking Sensation: Injuries to the MPFL can sometimes be accompanied by audible popping or clicking sensations within the knee joint, particularly during movement. These sounds may occur due to the patella shifting out of its normal alignment or rubbing against other structures within the knee.
Tenderness to Touch: The area around the inner side of the knee, where the MPFL attaches to the femur and patella, may become tender to the touch. Palpating this area can elicit pain and discomfort, especially if the injury is acute or if there is associated inflammation.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a review of how the injury occurred and any history of previous dislocations. A physical exam checks for looseness of the kneecap and signs of maltracking. X-rays help assess bone alignment. A computed tomography scan may be used to evaluate the shape of the knee. Magnetic resonance imaging shows the soft tissues clearly and can confirm a tear of the ligament.
Classification
Medial patellofemoral ligament injuries may be classified by the degree of tearing, the location of the tear, and the presence of repeated dislocations. Kneecap instability may also be graded by how often the kneecap slips and whether bone alignment contributes to the problem.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other causes of knee pain or instability include meniscus tears, ligament sprains, cartilage injuries, bursitis, tendon irritation, and generalized joint looseness. A careful exam and imaging studies help separate these conditions from kneecap instability.
Treatment Options
Non-Surgical Care
Initial care may include rest, bracing, physical therapy, and activity changes. These treatments strengthen the knee muscles and improve control of the kneecap. Some people recover without surgery after a single dislocation.
Surgical Care
Surgery is recommended after two or more dislocations or when the kneecap remains unstable. The procedure uses a small tendon graft, often taken from one of the hamstring muscles, to rebuild the torn ligament. The surgeon works through very small incisions using a camera and special instruments. The graft is attached to the inner side of the kneecap and the inner lower part of the thigh bone. Sometimes, if bone alignment contributes to the problem, the surgeon may reposition the bump of bone where the kneecap tendon attaches. After surgery, the knee is placed in a brace to protect the repair.
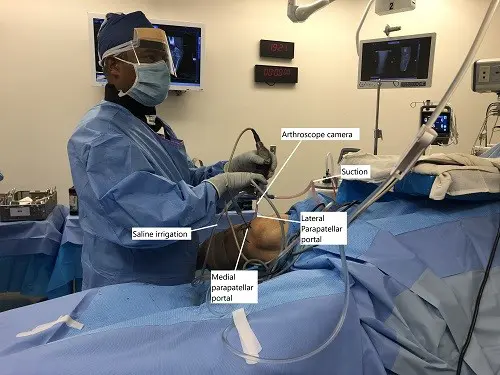
Intraoperative image showing arthroscopic repair of MPFL.
Recovery and What to Expect After Treatment
Recovery includes rest, ice, elevation, and pain-relief medicine. Physical therapy begins soon after surgery to restore motion and strength. A brace is worn to keep the knee straight during early healing. Most people return to daily activities within a few months, although full recovery varies.
Benefits of MPFL Reconstruction
MPFL Reconstruction offers several benefits for individuals experiencing knee instability:
Improved Stability: By repairing the MPFL, the surgery helps restore stability to the knee joint, reducing the risk of patellar dislocations.
Pain Relief: For many people, MPFL Reconstruction can alleviate pain and discomfort associated with knee instability.
Enhanced Function: With a stable knee joint, you’ll likely experience improved function and mobility, allowing you to participate in activities without fear of injury.
Possible Risks or Side Effects (Complications)
Risks include infection, stiffness, and soreness. There is also a chance the graft may not heal properly and may require further treatment. Temporary loss of motion is possible but usually improves with therapy.
Long-Term Outlook (Prognosis)
Most people who undergo this surgery regain stability and improved comfort. They are often able to return to normal activities without the fear of repeated kneecap dislocation. Long-term outlook is generally good when proper rehabilitation is followed.
Out-of-Pocket Costs
Medicare
CPT Code 27427 – MPFL Reconstruction: $168.63
CPT Code 20922 – Autograft tendon harvest (if performed): $145.72
CPT Code 20924 – Allograft (if used): $119.99
CPT Code 29873 – Arthroscopic lateral release (if performed): $128.93
Medicare usually pays most of the approved charges for these services, but a patient share remains. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield typically take care of the remaining twenty percent that Medicare does not cover. These plans are meant to fill that gap, so when the procedure is Medicare-approved, patients often do not owe anything further.
If you have secondary insurance through an employer plan, TRICARE, or the Veterans Health Administration, it acts as the next payer after Medicare. After any deductible is met, the secondary plan may cover the rest of the balance, including coinsurance. These plans may have their own deductible, which often ranges from $100 to $300 depending on the specific policy.
Workers’ Compensation
If your MPFL reconstruction is necessary because of a work-related injury, Workers’ Compensation covers the entire surgery and related care. There are no out-of-pocket expenses for you.
No-Fault Insurance
If your knee injury is caused by a motor vehicle accident, No-Fault Insurance covers the full cost of the procedure. The only possible charge would be a small deductible depending on your policy.
Example
A patient named Sarah required MPFL reconstruction due to repeated kneecap dislocations. Her estimated Medicare responsibility was $168.63 plus related add-on procedure amounts. Because she also carried secondary insurance, it covered the remaining share, leaving her with no out-of-pocket costs.
Frequently Asked Questions (FAQ)
Q. Will I be able to walk after surgery?
A. Yes, you will usually walk with a brace and support soon after the procedure.
Q. When can I return to sports?
A. Most people return to sports in a few months, but this depends on healing and therapy progress.
Q. Will the surgery stop the kneecap from dislocating again?
A. The goal is to greatly reduce or eliminate instability, but results vary depending on the individual.
Q. Does the surgery leave large scars?
A. No, the incisions are very small.
Q. Is the procedure painful?
A. Some pain and swelling are expected, but these improve with medication, ice, and therapy.
Summary and Takeaway
Medial patellofemoral ligament reconstruction is used to correct kneecap instability caused by a torn ligament. It improves stability, reduces pain, and helps prevent repeated dislocations. The procedure uses a small tendon graft to rebuild the damaged ligament, followed by structured therapy to restore strength and movement. With proper care and recovery, most people return to normal daily activities with a stable knee.
Clinical Insight & Recent Findings
A recent study reviewed outcomes of medial patellofemoral ligament reconstruction in skeletally immature patients and found that anatomic techniques—such as surface-based and transosseous fixation—had significantly lower redislocation rates and higher return-to-sport rates compared with nonanatomic methods, without evidence of growth-plate disturbance .
These findings support the surgical principles described above, where restoring stability to the kneecap with a precise, anatomically placed graft is essential for preventing recurrent dislocations and improving long-term knee function
The study’s results align with the goal of MPFL reconstruction as outlined in the clinical overview: to rebuild the ligament using a tendon graft, correct maltracking when necessary, and help patients return to normal activity with improved stability and reduced pain. (‘Study of MPFL reconstruction outcomes – see PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
This surgery is performed by orthopedic surgeons who specialize in knee injuries. Physician assistants, nurses, and physical therapists support the care before and after surgery.
When to See a Specialist?
You should see a specialist if your kneecap dislocates more than once, if the knee feels unstable, or if swelling and pain keep returning.
When to Go to the Emergency Room?
Go to the emergency room if the kneecap suddenly slips out of place and does not return on its own, if the knee becomes severely swollen, or if you are unable to move or straighten the leg.
What Recovery Really Looks Like?
Recovery involves controlled movement, gradual strengthening, and regular therapy. You may feel stiffness at first, but motion improves over time. Walking becomes easier as the ligament heals and the knee gains strength.
What Happens If You Ignore It?
If kneecap instability is ignored, repeated dislocations can lead to more pain, more damage to the cartilage, and the early development of arthritis.
How to Prevent It?
Strengthening the muscles around the knee, improving balance, and avoiding sudden twisting motions can help protect the kneecap. Proper rehabilitation after a first dislocation reduces future risk.
Nutrition and Bone or Joint Health
A balanced diet with protein, calcium, and vitamin D supports bone and tissue healing. Staying hydrated also helps joint function during recovery.
Activity and Lifestyle Modifications
After surgery, activities are reintroduced slowly. Low-impact exercises like cycling or swimming help rebuild strength without stressing the knee. High-impact sports should wait until full healing and clearance from your care team.
Do you have more questions?
How long does the surgery typically take?
The surgery usually takes about 1 to 2 hours to complete, depending on the complexity of the case.
Is MPFL Reconstruction performed under general anesthesia?
Yes, MPFL Reconstruction is typically performed under general anesthesia to ensure patient comfort throughout the procedure.
Will I need to stay in the hospital overnight after surgery?
In most cases, MPFL Reconstruction is performed as an outpatient procedure, meaning you can go home the same day. However, your surgeon will determine if overnight observation is necessary based on your individual circumstances.
How soon after surgery can I return to work or school?
The timing of your return to work or school will depend on the type of job or activities you engage in. In general, most patients can resume light activities within a few days to a week after surgery, but more strenuous activities may need to be avoided for several weeks.
What type of physical therapy will I need after MPFL Reconstruction?
Your physical therapy program will be tailored to your specific needs and goals, but it typically involves exercises to improve strength, flexibility, and range of motion in the knee. Your therapist will guide you through the process and monitor your progress closely.
How long will it take to fully recover from MPFL Reconstruction?
Recovery time can vary depending on factors such as the extent of the injury, the type of surgery performed, and individual healing rates. In general, most patients can expect to return to normal activities within 3 to 6 months after surgery.
Will I need to wear a brace after MPFL Reconstruction?
Your surgeon may recommend wearing a knee brace for a period of time after surgery to provide added support and stability to the knee joint during the initial stages of healing. However, this will depend on your specific situation and will be discussed with you before and after surgery.
What are the potential complications of MPFL Reconstruction?
Complications from MPFL Reconstruction are rare but can include infection, graft failure, stiffness, and nerve damage. Your surgeon will discuss these risks with you in detail before surgery and take steps to minimize them during the procedure.
How soon after surgery can I resume sports or physical activities?
You will need to wait until your surgeon and physical therapist determine that it is safe for you to return to sports or physical activities. This typically occurs around 4 to 6 months after surgery, although the timing may vary depending on your progress and the type of activities you wish to resume.
Will I be able to kneel after MPFL Reconstruction?
Most patients are able to kneel comfortably after MPFL Reconstruction once they have fully healed and completed their physical therapy program. Your surgeon will provide guidance on when it is safe to resume kneeling activities.
Can MPFL Reconstruction be performed using minimally invasive techniques?
Yes, MPFL Reconstruction can often be performed using minimally invasive techniques, which can result in smaller incisions, less pain, and faster recovery times compared to traditional open surgery.
How successful is MPFL Reconstruction in preventing future dislocations?
MPFL Reconstruction is generally highly successful in preventing future patellar dislocations, with success rates ranging from 85% to 95%. However, individual results may vary, and factors such as compliance with rehabilitation and activity modification can impact outcomes.
Will I need to avoid certain activities after MPFL Reconstruction?
Your surgeon may recommend avoiding high-impact activities or sports that involve repetitive twisting or pivoting movements to reduce the risk of reinjury to the knee. Your specific activity restrictions will be discussed with you during your postoperative appointments.
Can MPFL Reconstruction be performed as a standalone procedure, or is it typically done in conjunction with other knee surgeries?
MPFL Reconstruction can be performed as a standalone procedure or as part of a larger knee stabilization surgery, depending on the individual’s needs and the underlying cause of knee instability.
How soon after surgery will I be able to drive?
You should avoid driving until you are no longer taking prescription pain medication and can safely operate a vehicle. This typically occurs within a few days to a week after surgery, but you should check with your surgeon for specific guidance.
Will I need to undergo physical therapy before surgery?
Preoperative physical therapy may be recommended in some cases to help improve knee strength and range of motion prior to surgery. Your surgeon will advise you on whether prehabilitation is necessary based on your individual circumstances.
Are there any dietary restrictions I need to follow before or after surgery?
Your surgeon may recommend fasting for a certain period before surgery to reduce the risk of complications related to anesthesia. After surgery, it’s important to eat a healthy, balanced diet to support healing and recovery.
How long will I need to wear a knee brace after surgery?
The duration of knee brace use after surgery will vary depending on your surgeon’s recommendations and your individual progress. Some patients may only need to wear a brace for a few weeks, while others may require more extended use.
Will I need crutches after MPFL Reconstruction?
Crutches may be used immediately after surgery to help you move around safely while your knee heals. Your surgeon will advise you on how long you need to use crutches based on your specific situation.
Can MPFL Reconstruction be performed on both knees simultaneously?
While it is technically possible to perform MPFL Reconstruction on both knees at the same time, this approach is less common and may require a longer recovery period. Your surgeon will discuss the risks and benefits of bilateral surgery with you if it is deemed necessary.
How often will I need to follow up with my surgeon after MPFL Reconstruction?
You will typically have several follow-up appointments with your surgeon in the weeks and months following MPFL Reconstruction to monitor your progress, address any concerns, and adjust your treatment plan as needed.
Will I need to wear a brace during physical activity after I have fully recovered?
Your surgeon may recommend wearing a knee brace during high-risk activities or sports even after you have fully recovered from MPFL Reconstruction. This can provide added protection and reduce the risk of reinjury to the knee.
Can MPFL Reconstruction be performed on children or adolescents?
MPFL Reconstruction can be performed on children or adolescents who have persistent knee instability and recurrent patellar dislocations that have not responded to conservative treatment. However, the decision to proceed with surgery in this population should be carefully considered and discussed with a pediatric orthopedic specialist.

