Swelling is a common and expected response following total hip replacement (THR) surgery. It is a natural part of the healing process as the body works to repair the tissues and bone structures that were impacted during surgery. While some swelling is normal and typically subsides with time, excessive or persistent swelling could indicate complications such as infection or deep vein thrombosis (DVT), both of which require prompt attention and intervention. This guide explores the causes, symptoms, diagnosis, and management of swelling after hip replacement surgery, helping to differentiate normal post-operative healing from more serious issues.
Functional Anatomy
The hip joint is a ball-and-socket joint formed by the femoral head (the ball) and the acetabulum (the socket). During total hip replacement, the surgeon removes the damaged femoral head and the arthritic cartilage in the acetabulum and replaces them with metal and plastic prosthetics. The surgery involves cutting through various soft tissues around the hip joint, which leads to inflammation and swelling post-surgery. The lymphatic system and veins help clear the excess fluid, but gravity often causes fluid buildup in the lower leg, leading to visible swelling.
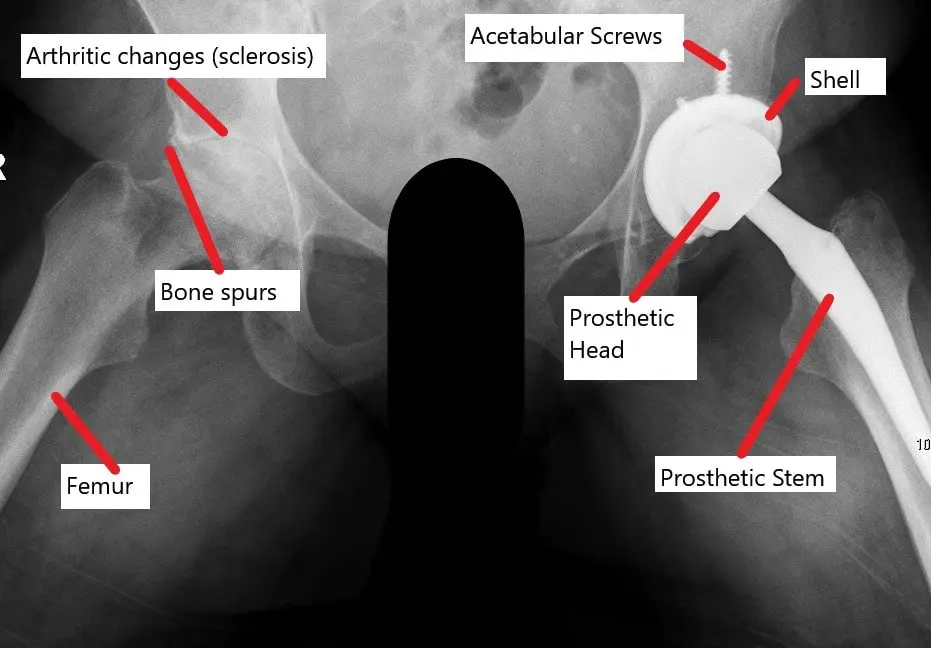
X-ray showing a total hip replacement with a contralateral arthritic joint.
Biomechanics or Physiology
Swelling after surgery is primarily caused by inflammation—a natural part of the body’s healing process. The body sends specialized cells called macrophages to the surgical site to aid in tissue healing. These cells trigger a release of fluid that builds up in the surrounding tissues, causing the swelling. During the healing process, blood vessels constrict to reduce the fluid accumulation, and the lymphatic system helps to clear excess fluid. Swelling is especially prominent in the leg due to gravity, which increases fluid retention, particularly in the lower extremities.
Common Variants and Anomalies
While swelling after hip replacement is usually expected, complications such as infection or deep vein thrombosis (DVT) may cause abnormal swelling. Additional issues such as heterotopic ossification (bone formation in soft tissue) or prosthetic-related complications can also contribute to post-operative swelling. Osteolysis, or bone resorption around the implant, may lead to abnormal fluid buildup and pain, requiring intervention.
Clinical Relevance
It is important to distinguish between normal post-surgical swelling and swelling due to serious complications. Infection and deep vein thrombosis can manifest with swelling, but these conditions are associated with other warning signs such as fever, redness, pain, and limited mobility. Differentiating between the two can help ensure timely treatment and prevent long-term complications. Vigilance is required in monitoring swelling, as early detection of complications can prevent the need for more invasive procedures, such as implant revision or surgical drainage.
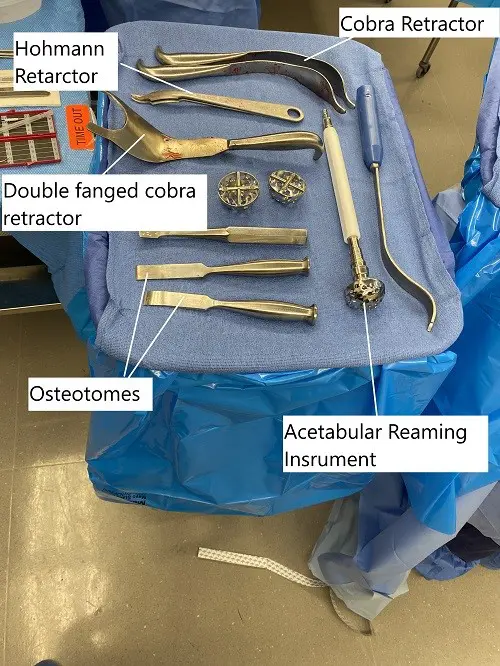
Instruments used in total hip replacement.
Imaging Overview
To evaluate the cause of persistent swelling, X-rays are used to check the alignment and integrity of the prosthetic components. If implant loosening or bone resorption is suspected, CT scans or MRI can provide more detailed images of the bones and soft tissues. Ultrasound is often used to diagnose deep vein thrombosis, as it can identify blood clots in the veins of the leg. In the case of infection, joint aspiration (removal of synovial fluid for culture) may be performed to detect bacteria.
Associated Conditions
Swelling following hip replacement may be associated with:
- Infection (prosthetic joint infection, PJI): Infection can lead to bone erosion, discharge, fever, and increasing pain.
- Deep vein thrombosis (DVT): Blood clot formation in the leg can cause swelling, pain, and potentially a pulmonary embolism if the clot dislodges.
- Heterotopic ossification: Abnormal bone formation in the surrounding soft tissues, leading to pain and restricted movement.
- Osteolysis: Bone loss around the implant may cause swelling and pain due to debris accumulation and inflammation.
Surgical or Diagnostic Applications
Diagnostic evaluation of swelling typically involves:
- Physical examination to assess for tenderness, warmth, or redness around the surgical site, as well as mobility and function of the hip.
- Blood tests to detect markers of infection (elevated ESR, CRP) or signs of clotting issues.
- Imaging (X-ray, CT, MRI, or ultrasound) to evaluate for joint alignment, fluid buildup, or complications such as DVT or infection.
- Joint aspiration for infection detection, particularly if there is suspicion of septic loosening or post-operative infection.
Prevention and Maintenance
While some degree of swelling is unavoidable, several strategies can help minimize swelling and speed up recovery:
- Elevation of the leg above the level of the heart to facilitate fluid drainage.
- Compression stockings to help with circulation and prevent fluid accumulation.
- Icing the hip and leg to reduce inflammation during the first few days post-surgery.
- Early mobilization and rehabilitation exercises, such as ankle pumps and gradual walking, to promote blood circulation and prevent clot formation.
- Anticoagulant medications (such as heparin or aspirin) may be prescribed to reduce the risk of deep vein thrombosis (DVT) and pulmonary embolism.
Research Spotlight
After undergoing a total hip replacement, some degree of leg swelling is expected as part of the body’s natural healing response. Swelling is generally managed with conservative measures like icing, leg elevation, and compression stockings.
A recent study has explored the role of an elastic compression dressing in reducing postoperative leg swelling.The study found a slight reduction in swelling in patients using the compression dressing, although the overall effect was modest and not enough to significantly improve clinical outcomes.
The study also showed no significant reduction in blood loss or transfusion rates, highlighting that while compression may help with swelling, its benefits are minimal in terms of other postoperative complications. (“Study on the effect of compression dressing on leg swelling after hip replacement – see PubMed.“)
Summary and Key Takeaways
- Swelling after hip replacement surgery is a normal part of the healing process, but excessive swelling may signal infection or deep vein thrombosis (DVT).
- Imaging and blood tests are essential tools for diagnosing the underlying cause of persistent swelling.
- Prevention strategies, such as elevation, compression, and early mobilization, can help reduce swelling and improve recovery.
- Anticoagulation therapy and rehabilitation exercises play an important role in preventing complications like DVT and ensuring a smooth recovery.
- Prompt intervention and close monitoring for signs of infection or DVT can prevent further complications and ensure long-term success after surgery.
Do you have more questions?
Is swelling after hip replacement surgery normal, or could it indicate a complication?
Swelling is a normal part of the healing process after hip replacement surgery. However, if swelling is excessive, accompanied by severe pain or other concerning symptoms, it could indicate a complication such as infection or deep vein thrombosis.
How can I differentiate between normal postoperative swelling and signs of infection or other complications?
Signs of infection or other complications include redness, warmth, increased pain, fever, and drainage from the incision site. If you experience these symptoms, it’s important to contact your surgeon promptly.
What can I do to reduce swelling after hip replacement surgery?
Elevating the leg, applying ice packs, wearing compression stockings, staying hydrated, and performing gentle exercises as recommended by your surgeon or physical therapist can help reduce swelling.
Can certain medications contribute to swelling after hip replacement surgery?
Yes, certain medications such as blood thinners or pain medications may contribute to swelling as a side effect. It’s important to discuss any concerns about medication side effects with your healthcare provider.
How does swelling affect the recovery process after hip replacement surgery?
Swelling can temporarily limit mobility and increase discomfort during the early stages of recovery. However, as swelling decreases, mobility and comfort typically improve.
: Are there specific factors that can increase the risk of swelling after hip replacement surgery?
Factors such as obesity, pre-existing circulation problems, prolonged surgery, and certain medical conditions may increase the risk of swelling after hip replacement surgery.
Can swelling after hip replacement surgery affect the success of the procedure or the longevity of the implant?
While swelling itself is unlikely to affect the success of the procedure or the longevity of the implant, persistent or excessive swelling may warrant further evaluation to rule out underlying issues that could impact outcomes.
How does swelling after hip replacement surgery impact the range of motion and function of the hip joint?
Initially, swelling may limit the range of motion and function of the hip joint. However, as swelling decreases and rehabilitation progresses, range of motion and function typically improve.
Is it normal for swelling to fluctuate or worsen at certain times during the recovery process?
Yes, swelling may fluctuate or worsen at times, particularly after periods of increased activity or when the leg is dependent for prolonged periods. This is normal and usually resolves with rest and elevation.
Can dietary factors influence swelling after hip replacement surgery?
Maintaining a balanced diet and staying hydrated can help reduce swelling after hip replacement surgery. Avoiding excessive salt intake may also help minimize fluid retention.
Are there any warning signs associated with swelling after hip replacement surgery that require immediate medical attention?
Warning signs that require immediate medical attention include sudden or severe swelling, increasing redness or warmth around the incision site, fever, and difficulty breathing.
How does swelling after hip replacement surgery impact the fit and comfort of clothing and footwear?
Swelling may temporarily affect the fit and comfort of clothing and footwear, particularly around the hip and thigh area. Wearing loose-fitting clothing and supportive footwear can help alleviate discomfort.
Can elevation of the leg help reduce swelling after hip replacement surgery, and if so, how often and for how long should it be done?
Yes, elevating the leg above heart level can help reduce swelling after hip replacement surgery. It’s generally recommended to elevate the leg for several times a day for about 20-30 minutes each session, as tolerated.
How does the presence of swelling impact the assessment of surgical incisions and monitoring for signs of infection?
Swelling can make it more challenging to assess surgical incisions and monitor for signs of infection, such as redness or drainage. However, careful inspection and regular wound care are still important.
Can swelling after hip replacement surgery affect sleep patterns or overall comfort during rest?
Yes, swelling may cause discomfort and difficulty finding a comfortable sleeping position, particularly in the early stages of recovery. Using pillows to elevate the leg and support the hip can help improve comfort.
Can the application of heat therapy help reduce swelling after hip replacement surgery, or is cold therapy preferred?
Cold therapy is typically preferred in the early stages after hip replacement surgery to reduce swelling and inflammation. Heat therapy may be used later in the recovery process to promote relaxation and muscle flexibility.
How does the use of compression garments or wraps affect swelling after hip replacement surgery?
Compression garments or wraps can help reduce swelling by providing gentle pressure to the affected area, promoting fluid drainage, and supporting the surrounding tissues. However, it’s important to ensure that compression is applied correctly to avoid restricting blood flow.
Can massage therapy or lymphatic drainage techniques help reduce swelling after hip replacement surgery?
Yes, gentle massage therapy or lymphatic drainage techniques performed by a trained professional may help reduce swelling and improve circulation in the affected area. However, it’s important to consult with your healthcare provider before starting any new therapies.
How does the timing and intensity of physical activity or rehabilitation exercises impact swelling after hip replacement surgery?
Gradually increasing the intensity and duration of physical activity and rehabilitation exercises as tolerated can help minimize swelling and promote healing after hip replacement surgery. However, overexertion or excessive activity may exacerbate swelling and delay recovery.

