Total hip replacement (THR) is one of the most reliable and successful orthopedic procedures, often restoring mobility and relieving chronic pain caused by arthritis or injury. Most hip implants last 20–25 years or longer, but over time, wear and tear of the prosthetic components may occur. This can lead to aseptic loosening, where the implant loses its attachment to the bone in the absence of infection. While gradual implant wear is expected over decades, certain factors—such as younger age, male gender, obesity, and high physical activity—can accelerate the process.
Functional Anatomy
A total hip replacement replicates the ball-and-socket structure of the natural hip joint. The femoral head (ball) is replaced with a metal or ceramic prosthetic head, which is attached to a metal stem inserted into the femoral canal. The acetabulum (socket) is fitted with a metal shell, which may be press-fit or secured with screws, and lined with a high-grade polyethylene (plastic) insert that allows smooth gliding of the prosthetic head. Over time, repetitive motion and load-bearing can produce microscopic wear particles, particularly at the interface between the metal head and polyethylene liner, leading to inflammation and bone loss.
Biomechanics or Physiology
The longevity of a hip replacement depends on the mechanical balance between the implant and bone. The implant must integrate properly with the bone through bone in-growth or cement fixation to provide long-term stability. Microscopic friction between the moving components (head and liner) generates wear particles that can trigger an inflammatory response. This inflammation stimulates osteoclasts, the bone-resorbing cells, leading to osteolysis (bone loss) and implant loosening. As the implant becomes unstable, patients experience pain, instability, and reduced function.
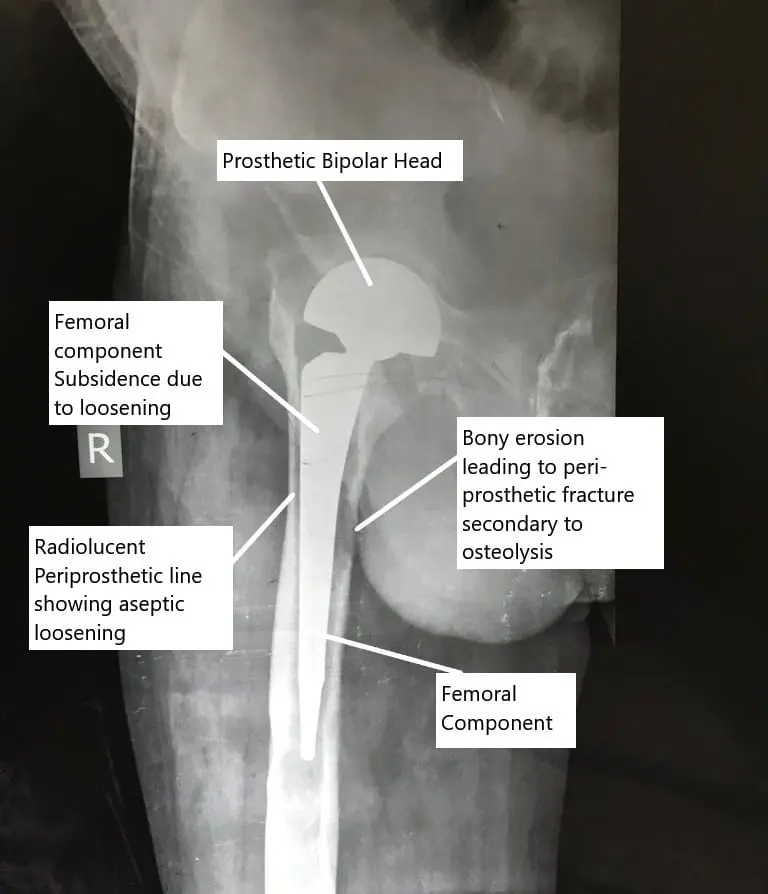
X-ray showing aseptic loosening of the hip replacement.
Common Variants and Anomalies
The rate and pattern of implant wear depend on factors such as:
- Implant material combination (e.g., metal-on-polyethylene, ceramic-on-ceramic, or metal-on-metal).
- Activity level and body weight (higher activity and obesity increase mechanical stress).
- Implant alignment and surgical technique (improper positioning accelerates wear).
- Bone quality (osteoporosis or metabolic disorders may affect implant fixation).
Among implant types, metal-on-polyethylene implants tend to produce more wear debris, while ceramic-on-ceramic implants generate less debris but may cause squeaking or fracture.
Clinical Relevance
Aseptic loosening is the most common long-term complication following total hip replacement and remains a leading cause for revision surgery. Patients typically develop pain after a painless interval following surgery, usually years later. The pain is often felt in the groin and worsens with weight-bearing or movement. Some patients may also report instability or the sensation of the hip “slipping.” Early identification of aseptic loosening through clinical evaluation and imaging is crucial to prevent extensive bone loss and ensure successful revision outcomes.
Imaging Overview
- X-rays are the first-line imaging study for evaluating implant stability. They may reveal radiolucent lines (clear spaces around the implant), bone thinning, or component migration.
- CT scans provide more detailed information on bone loss, component orientation, and surrounding bone integrity.
- MRI is useful for evaluating soft tissue inflammation, muscle status, or fluid collections.
- Nuclear bone scans can help distinguish between infection and aseptic loosening, with infection typically showing more diffuse uptake patterns.
Associated Conditions
Aseptic loosening may coexist with or be mimicked by other conditions such as:
- Periprosthetic joint infection (PJI) – infection-induced bone loss that must be ruled out before revision surgery.
- Osteolysis – bone loss due to chronic inflammation from debris particles without complete loosening.
- Periprosthetic fractures – fractures around the implant that may occur secondary to weakened bone.
- Stress shielding – bone loss due to the implant absorbing load instead of the surrounding bone.
Surgical or Diagnostic Applications
Diagnosis of aseptic loosening is made through a combination of clinical symptoms, physical examination, and radiological findings.
- Physical Examination: May reveal hip tenderness, instability, or abnormal movement (“clunking”).
- Diagnostic Tests: Blood tests (ESR, CRP) and joint aspiration are performed to rule out infection.
- Surgical Management: The definitive treatment is revision total hip replacement, which may involve replacing all or part of the implant. In some cases, only the loosened component (femoral stem or acetabular shell) is revised. Revision surgery is more complex than the primary procedure and should be performed by an experienced surgeon.
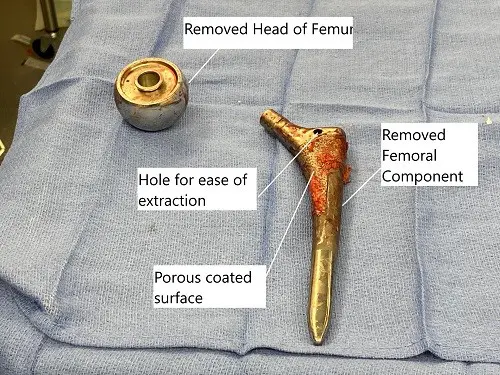
Extracted head of femur and the femoral component during revision surgery.
Prevention and Maintenance
To prolong the lifespan of a total hip replacement and reduce the risk of wear-related complications, patients should:
- Maintain a healthy body weight to reduce joint stress.
- Avoid high-impact activities (e.g., running or jumping).
- Undergo regular follow-up with imaging every few years to monitor for early signs of loosening.
- Ensure proper implant positioning during the initial surgery, performed by a skilled orthopedic surgeon.
- Maintain muscle strength and flexibility through prescribed physical therapy to reduce abnormal loading forces.
Summary and Key Takeaways
- Implant wear is an inevitable long-term consequence of total hip replacement but usually occurs gradually over decades.
- Aseptic loosening—loosening of components without infection—is the most common reason for revision surgery.
- Polyethylene debris triggers an inflammatory response that leads to bone loss and implant micromotion.
- X-rays and CT scans are essential for diagnosing implant loosening and bone loss.
- Revision surgery is the main treatment, with improved implant materials (e.g., highly cross-linked polyethylene) reducing wear rates.
- Preventive strategies include maintaining proper body weight, following activity restrictions, and undergoing regular orthopedic follow-up.
Do you have more questions?
Can wearing out of a total hip replacement cause pain or discomfort?
Yes, wearing out of a total hip replacement can lead to pain, discomfort, and decreased mobility as the implant components degrade over time.
How common is wearing out of a total hip replacement?
Wearing out of a total hip replacement is relatively common, especially in individuals who have had the implant for many years or are highly active.
Are there specific activities that increase the risk of wearing out a total hip replacement?
Activities that place repetitive stress on the hip joint, such as high-impact sports or heavy lifting, can increase the risk of wearing out a total hip replacement.
What are the symptoms of wearing out of a total hip replacement?
Symptoms may include increased hip pain, stiffness, decreased range of motion, swelling around the hip joint, and difficulty walking or bearing weight on the affected side.
How is wearing out of a total hip replacement diagnosed?
Diagnosis typically involves a combination of clinical evaluation, imaging studies such as X-rays or MRI scans, and assessment of symptoms and functional limitations.
Can wearing out of a total hip replacement be prevented?
While wearing out of a total hip replacement cannot always be prevented, certain measures such as maintaining a healthy weight, avoiding excessive stress on the hip joint, and following post-operative care guidelines can help prolong the lifespan of the implant.
What are the treatment options for wearing out of a total hip replacement?
Treatment options may include conservative measures such as pain management, physical therapy, and activity modification, as well as surgical interventions such as revision hip replacement to replace the worn-out components.
How long does recovery take after revision hip replacement surgery for wearing out of a total hip replacement?
Recovery time after revision hip replacement surgery varies depending on factors such as the extent of the procedure, individual patient factors, and adherence to post-operative rehabilitation protocols.
What are the risks associated with revision hip replacement surgery for wearing out of a total hip replacement?
Risks of revision hip replacement surgery include infection, bleeding, blood clots, implant loosening or failure, nerve or blood vessel injury, and complications related to anesthesia.
Are there any factors that increase the risk of wearing out of a total hip replacement, such as patient age or implant materials?
Factors that may increase the risk of wearing out of a total hip replacement include patient age, implant materials, activity level, implant positioning, and surgical technique.
Can wearing out of a total hip replacement affect other parts of the body, such as the spine or knees?
Yes, wearing out of a total hip replacement can alter gait mechanics and place increased stress on other joints such as the spine or knees, potentially leading to secondary complications over time.
How often should individuals with a total hip replacement undergo follow-up appointments to monitor for signs of wearing out?
Individuals with a total hip replacement should undergo regular follow-up appointments with their orthopedic surgeon to monitor for signs of wearing out and assess implant function and integrity.
Can wearing out of a total hip replacement lead to complications such as metallosis or adverse tissue reactions?
Yes, wearing out of a total hip replacement can lead to complications such as metallosis (metal poisoning) or adverse tissue reactions due to the release of metal ions from the implant components.
Are there any dietary or lifestyle modifications that can help slow down the wearing out of a total hip replacement?
While there are no specific dietary or lifestyle modifications proven to prevent wearing out of a total hip replacement, maintaining a healthy weight, staying physically active within recommended limits, and avoiding smoking may help optimize overall joint health.
Can individuals with a total hip replacement safely participate in physical activities such as sports or exercise classes?
In general, individuals with a total hip replacement can safely participate in low-impact activities such as swimming, cycling, or walking. However, high-impact sports or activities that place excessive stress on the hip joint should be avoided to minimize the risk of wearing out the implant.
How does the type of implant material used in a total hip replacement affect the risk of wearing out?
The type of implant material used in a total hip replacement, such as metal-on-metal, metal-on-polyethylene, ceramic-on-ceramic, or ceramic-on-polyethylene, can influence the risk of wearing out and the longevity of the implant.
Can individuals with a total hip replacement experience symptoms of wearing out even if the implant appears intact on imaging studies?
Yes, individuals with a total hip replacement can experience symptoms of wearing out even if the implant appears intact on imaging studies, as wear-related changes may not always be visible on imaging and can manifest clinically.
Are there any alternative treatments or therapies available for individuals experiencing symptoms of wearing out of a total hip replacement?
Alternative treatments or therapies for symptoms of wearing out of a total hip replacement may include non-invasive modalities such as acupuncture, chiropractic care, or physical therapy to manage pain and improve joint function.
Can wearing out of a total hip replacement affect the stability or alignment of the hip joint?
Yes, wearing out of a total hip replacement can lead to changes in implant position, joint stability, and alignment, which may contribute to symptoms such as pain, stiffness, and decreased mobility. Regular monitoring and timely intervention may be necessary to address these issues and prevent further complications.

