Knee replacement surgery is one of the most commonly performed procedures in orthopedics, often providing relief from chronic knee pain caused by conditions like arthritis. While this procedure is generally successful, swelling and discomfort in the knee area are common concerns for patients post-surgery. Understanding the causes of swelling, when to be concerned, and how to manage it is crucial for a smooth recovery.
How Common It Is and Who Gets It? (Epidemiology)
Knee replacement surgery is primarily performed on individuals suffering from osteoarthritis or other degenerative joint diseases. It is most common in older adults, typically those aged 60-80. However, younger patients with severe arthritis or knee damage from injury may also require this surgery. The prevalence of knee replacement is expected to rise as the population ages and more individuals seek relief from chronic knee pain.
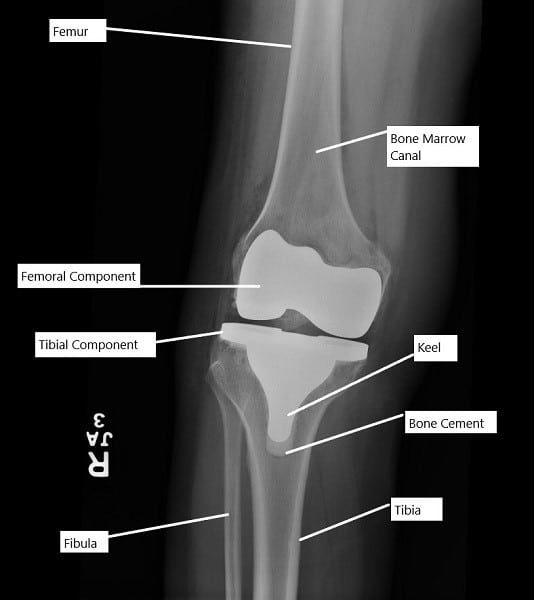
X-ray showing a total knee replacement.
Why It Happens – Causes (Etiology and Pathophysiology)
Swelling after knee replacement surgery is a natural part of the body’s healing process. The surgery involves cutting through tissues, including skin, muscles, and bone, which causes inflammation. The body responds by sending fluid to the affected area to aid in the healing process. Additionally, factors such as blood vessel changes, fluid accumulation, and the body’s inflammatory response contribute to the swelling. In some cases, swelling can indicate complications such as deep vein thrombosis or an infection of the prosthetic joint.
Surgical Impact: The physical manipulation of bone and tissue during surgery causes an inflammatory response.
Fluid Accumulation: The body’s response includes increasing fluid in the knee area to aid in healing, which contributes to swelling.
Blood Vessel Changes: Surgery can affect blood flow dynamics around the knee, further contributing to fluid buildup.
How the Body Part Normally Works? (Relevant Anatomy)
The knee joint is a hinge joint made up of the femur (thigh bone), tibia (shin bone), fibula (calf bone), and patella (kneecap). Ligaments, tendons, and cartilage help stabilize and allow movement in the knee. In total knee replacement surgery, the damaged portions of the femur and tibia are removed and replaced with metal and plastic components to restore the joint’s function.
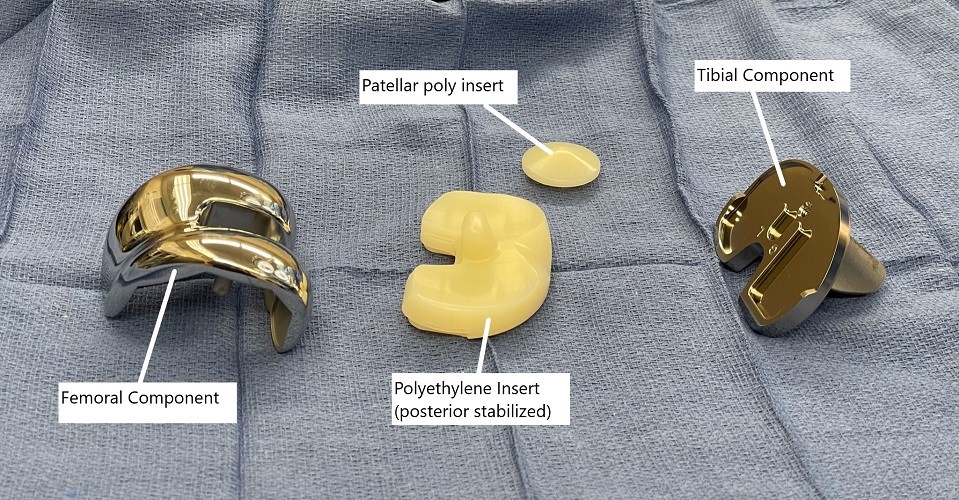
Intraoperative image showing knee replacement implants.
What You Might Feel – Symptoms (Clinical Presentation)
After knee replacement surgery, it is normal to experience some pain, swelling, and stiffness. Patients may also notice limited movement in the knee joint as it heals. The swelling may be more pronounced at the end of the day or after physical activity. If swelling is accompanied by redness, warmth, or fever, it could indicate infection or other complications and should be promptly addressed.
How Doctors Find the Problem? (Diagnosis and Imaging)
The diagnosis of swelling after knee replacement surgery is generally made based on clinical examination and patient history. Imaging studies, such as X-rays or ultrasounds, may be used to assess the placement of the prosthetic components and rule out complications such as infection or deep vein thrombosis.
Classification
Swelling after knee replacement can be classified as mild, moderate, or severe, depending on its extent and the presence of other symptoms. Mild swelling is expected and tends to resolve with time. Moderate to severe swelling that does not improve or is associated with other symptoms may require further investigation to rule out complications.
Other Problems That Can Feel Similar (Differential Diagnosis)
Swelling in the knee after surgery can sometimes be mistaken for other conditions. It is essential to distinguish between post-surgical swelling and issues such as infection, blood clots, or a failure of the prosthetic joint. Deep vein thrombosis (DVT) can cause swelling and should be ruled out. Infection of the knee joint can also present with swelling, redness, and pain, which requires immediate medical attention.
Treatment Options
Non-Surgical Care
Managing swelling post-surgery involves rest, elevation, and the application of ice. Over-the-counter anti-inflammatory medications may be used to control swelling and pain. Physical therapy is also crucial for improving movement and reducing swelling by promoting fluid drainage.
Surgical Care
In some cases, surgical intervention may be required if swelling is caused by complications such as infection or blood clots. Infected prosthetic joints may require revision surgery, and blood clots may require procedures to remove or dissolve the clot.
Recovery and What to Expect After Treatment
Swelling typically peaks in the first few days after surgery and gradually decreases as healing progresses. However, mild swelling may persist for several months. Adhering to post-operative care, including ice therapy, leg elevation, and movement exercises, can help manage swelling and accelerate recovery. Full recovery from knee replacement surgery can take up to 6 months.
Possible Risks or Side Effects (Complications)
While swelling is a common and generally benign complication, it may signal more serious issues such as infection, deep vein thrombosis, or joint instability. Symptoms of infection include redness, warmth, fever, and purulent discharge from the surgical site. Severe swelling combined with leg pain may indicate a blood clot, which can lead to a life-threatening pulmonary embolism if left untreated.
Long-Term Outlook (Prognosis)
For most patients, swelling will decrease over time as the body heals. While mild swelling can persist for several months, it typically resolves with continued physical therapy and proper self-care. However, if swelling is associated with complications like infection or blood clots, the prognosis depends on early intervention and appropriate treatment.
Out-of-Pocket Costs
Medicare
CPT Code 20610 – Joint Aspiration for Infection Evaluation: $15.12
CPT Code 27301 – Irrigation & Debridement of Infected Prosthetic Knee: $159.02
CPT Code 27486 – Irrigation & Debridement of Infected Prosthetic Knee (if Component Revision): $332.04
CPT Code 27487 – Revision Total Knee Replacement (Femoral + Tibial Components): $413.16
CPT Code 34201 – Blood Clot Removal (Thrombectomy, Lower Extremity): $237.43
CPT Code 34203 – Blood Clot Removal (Thrombectomy, Lower Extremity, if bilateral): $220.95
Under Medicare, 80% of the approved amount for these procedures is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved procedures. These supplemental plans work directly with Medicare to ensure full coverage for the procedures.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, ranging from $100 to $300, depending on the specific policy and network status.
Workers’ Compensation
If your knee infection, thrombosis, or surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your knee surgery or thrombectomy is the result of a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses. The only possible out-of-pocket cost may be a small deductible depending on your individual policy terms.
Example
Emily, a 63-year-old patient with a knee prosthesis infection, required irrigation and debridement of her infected knee (CPT 27301) and later underwent a total knee replacement revision (CPT 27487). Her estimated Medicare out-of-pocket costs were $159.02 for the debridement and $413.16 for the knee revision. Since Emily had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving her with no out-of-pocket expenses for the procedures.
Frequently Asked Questions (FAQ)
Q. How long will swelling last after knee replacement surgery?
A. Swelling is expected to last for a few weeks to months after surgery. It should gradually improve, but mild swelling may persist for up to six months.
Q. What can I do to reduce swelling after surgery?
A. Elevating your leg, applying ice, and using compression stockings can help reduce swelling. Physical therapy exercises and prescribed medications may also be beneficial.
Q. Is swelling a sign of infection after knee replacement surgery?
A. Swelling is common after knee replacement surgery and does not necessarily indicate infection. However, if swelling is accompanied by redness, fever, or discharge from the surgical site, it may suggest an infection and should be evaluated by a healthcare provider.
Summary and Takeaway
Swelling is a normal part of recovery after knee replacement surgery and typically resolves within a few months. However, patients should be vigilant for signs of complications, such as infection or deep vein thrombosis, which require immediate medical attention. Proper post-surgical care, including rest, elevation, ice, and physical therapy, can help reduce swelling and improve recovery.
Clinical Insight & Recent Findings
A recent study systematically reviewed the effects of manual therapy on pain management after total knee replacement (TKR) surgery. The findings indicated that manual therapy techniques, including osteopathic manipulative treatment (OMT), manual lymphatic drainage (MLD), and kinesio taping (KT), show promise in reducing pain and improving functional outcomes in the early postoperative period.
Specifically, MLD and KT were particularly effective in managing pain and swelling shortly after surgery, with improvements observed by day 4 post-surgery, although these benefits were generally short-lived.
Despite these encouraging results, the study highlighted the variability in outcomes across different interventions, underscoring the need for further research to refine protocols and better understand the long-term benefits of manual therapy in TKR rehabilitation. (“Study on manual therapy for postoperative knee rehabilitation – See PubMed“.)
Who Performs This Treatment? (Specialists and Team Involved)
Knee replacement surgery is typically performed by an orthopedic surgeon specializing in joint replacement. Post-operative care is managed by a team that may include physical therapists, nurses, and pain management specialists to optimize recovery and manage swelling.
When to See a Specialist?
If swelling is not improving or is accompanied by severe pain, redness, fever, or difficulty breathing, it is essential to seek immediate medical attention. A healthcare provider should be consulted if swelling persists beyond the expected time frame or worsens.
When to Go to the Emergency Room?
Seek emergency care if you experience sudden and severe pain, swelling that rapidly increases, chest pain, or shortness of breath. These symptoms could indicate serious complications like deep vein thrombosis or a pulmonary embolism.
What Recovery Really Looks Like?
Recovery from knee replacement surgery involves managing swelling, restoring movement, and regaining strength. While some patients can begin walking the day after surgery, full mobility is often achieved within a few months, with ongoing physical therapy.
What Happens If You Ignore It?
Ignoring excessive or worsening swelling can lead to complications such as infection or blood clots, which can significantly delay recovery and may require additional surgeries. Timely intervention is crucial to avoid long-term problems.
How to Prevent It?
To minimize swelling, patients should follow post-operative care instructions carefully, including regular exercise to promote circulation, elevation of the leg, and application of ice. Wearing compression stockings and using blood-thinning medications may also help reduce the risk of complications like blood clots.
Nutrition and Bone or Joint Health
A well-balanced diet rich in nutrients, including vitamins C and D, calcium, and protein, supports healing and overall joint health. Hydration is also crucial to help manage fluid retention and support the healing process after knee surgery.
Activity and Lifestyle Modifications
Patients should gradually increase activity levels post-surgery to avoid overexertion and worsening of swelling. Avoiding long periods of standing or sitting and performing gentle exercises, as recommended by a physical therapist, can help prevent complications and improve circulation.
Do you have more questions?
What exactly causes the body to react with swelling after knee replacement surgery?
Swelling is a natural part of the body’s inflammatory response to surgery, where increased fluid and white blood cells are sent to the knee to aid in healing and fight any potential infection.
Are there specific surgical techniques that reduce the risk of severe swelling?
Yes, minimally invasive surgical techniques and careful management of tissue handling can reduce the extent of trauma and, subsequently, swelling.
How long does swelling usually last after knee replacement?
Typically, swelling peaks within the first few days post-surgery and gradually decreases over the following weeks, but some mild swelling can persist for several months.
Can swelling affect the long-term outcome of my knee replacement?
Persistent or excessive swelling can potentially impact the healing process and knee function, but with proper management, long-term outcomes are generally very good.
What are the best ways to measure knee swelling at home?
Measuring the circumference of the knee with a tape measure at regular intervals can provide a quantitative way to track changes in swelling.
Is there a difference in swelling between robotic-assisted and traditional knee surgery?
Robotic-assisted surgery may result in less tissue damage and therefore potentially less swelling, although individual results can vary.
Does the type of knee implant affect swelling?
The type of implant itself typically does not directly affect swelling; however, the technique and accuracy of implant placement might.
What medications are best for controlling swelling after knee surgery?
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) are commonly used to reduce swelling and pain, but they should be taken under the guidance of a healthcare provider due to potential side effects.
How can I differentiate between normal swelling and an infection?
Normal swelling should gradually improve with time and respond to elevation and ice. If swelling is accompanied by increased pain, redness, or warmth, or if it worsens suddenly, it may indicate an infection.
Should I be concerned if one leg is more swollen than the other after bilateral knee replacements?
It’s not uncommon for one knee to swell more than the other, but significant differences should be evaluated by your surgeon.
Can diet affect swelling after knee replacement?
Yes, a diet high in sodium can exacerbate swelling, while foods rich in anti-inflammatory agents like omega-3 fatty acids can help reduce it.
How does physical therapy help manage swelling?
Physical therapy helps by promoting fluid drainage through movement and strengthening exercises, which also improve joint function and range of motion.
What role does compression therapy play in managing swelling?
Compression garments or bandages help reduce swelling by preventing fluid accumulation in the tissue around the knee.
When should I be able to stop using ice on my knee?
Ice can be used in the initial weeks post-surgery as needed to help control swelling and pain, typically decreasing in frequency as the swelling subsides.
Is elevation really effective for swelling?
Yes, elevating the leg above the level of the heart helps reduce the gravitational pull on fluids, decreasing swelling.
Can massage therapy reduce swelling after knee replacement?
Gentle massage may help by encouraging fluid movement away from the knee, but it should be performed by a professional familiar with post-operative care.
What are the signs that swelling is not resolving normally?
Persistent swelling, increased pain, decreased mobility, or signs of infection are indications that the swelling isn’t resolving as expected and should be checked by a healthcare provider.
Can I take diuretics to help with swelling?
Diuretics are not typically recommended for swelling due to knee surgery, as they can lead to other complications. It’s best to manage swelling through elevation, ice, and mobility.
What if the swelling suddenly increases a few weeks after surgery?
An increase in swelling after initial improvement could indicate activity-related inflammation or a complication such as an infection or blood clot, and should be evaluated urgently.
Are there any exercises I should avoid to prevent worsening the swelling?
High-impact activities like running or jumping should be avoided in the early post-operative period to prevent exacerbatingthe swelling. Gentle stretching and low-impact activities like walking and cycling are encouraged.
Can weather affect knee swelling after surgery?
Yes, changes in atmospheric pressure and humidity can affect joint swelling. Some patients report increased swelling in colder or damp weather.
Should I use heat or cold to treat the swelling?
In the initial post-operative phase, cold is generally recommended to reduce swelling and numb pain. Heat may be used later in the recovery to aid muscle relaxation and improve circulation once the acute swelling has subsided.
What are the consequences of not managing swelling effectively?
Poor management of swelling can lead to stiffness, reduced mobility, prolonged recovery, and in some cases, chronic swelling.
How soon after surgery can I expect my knee to look ‘normal’ again?
Most of the noticeable swelling subsides within the first few months, but complete recovery and the return to a ‘normal’ appearance can take up to a year, depending on various factors including the individual’s health and adherence to rehabilitation.
Is there a correlation between swelling and scar tissue formation?
Yes, excessive or prolonged swelling can lead to increased scar tissue formation, which might affect the knee’s function and range of motion. Proper management of swelling helps to minimize this risk.
