A dural tear is an opening or injury in the thin outer covering of the spinal cord and nerve roots, called the dura mater. This layer holds the cerebrospinal fluid (CSF), which cushions and nourishes the brain, spinal cord, and nerves. When the dura is torn, CSF can leak out, sometimes causing headaches, nausea, or other complications if not treated properly.
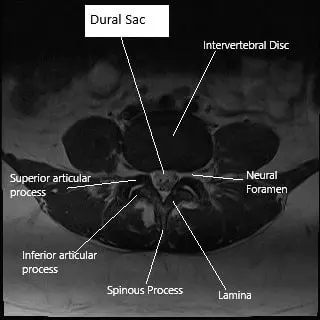
Axial section (MRI) of lumbar spine showing dural sac.
How Common It Is and Who Gets It? (Epidemiology)
Dural tears are among the most common complications of spine surgery, particularly in procedures on the lumbar spine. They may occur in 1% to 17% of surgeries, depending on the type and complexity of the operation. Although dural tears can happen in any patient, those who have had previous spine surgeries or scarring around the dura have a higher risk.
Why It Happens – Causes (Etiology and Pathophysiology)
Dural tears can occur in two main ways:
- Accidental (inadvertent) injury: Surgical instruments or bone spurs can puncture or nick the dura during spinal procedures.
- Intentional incision: The surgeon may open the dura deliberately to access or remove a lesion or tumor.
In rare cases, a dural tear may develop after surgery if the dura was weakened, if infection occurs, or if scar tissue pulls on the repair site.
How the Body Part Normally Works? (Relevant Anatomy)
The dura is the tough, protective outer membrane surrounding the brain and spinal cord. It contains cerebrospinal fluid, which serves as a cushion and delivers nutrients to nerve tissues. Underneath the dura are finer membranes (arachnoid and pia mater) that further protect the spinal cord. When the dura is torn, CSF leaks out, lowering pressure in the brain and spinal canal. This can lead to postural headaches (worse when standing), dizziness, and nausea.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of a dural tear depend on whether the leak occurs during or after surgery. Common signs include:
- Headache that worsens when sitting or standing
- Nausea, dizziness, or ringing in the ears
- Clear fluid drainage from the wound or nose (rare)
- Fatigue or neck stiffness
- Occasionally, pain or swelling near the incision site
In many cases, if the tear is recognized and repaired immediately, patients may not experience any symptoms at all.
How Doctors Find the Problem? (Diagnosis and Imaging)
Most dural tears are detected during surgery, when CSF leakage is seen directly. If not identified right away, doctors may suspect a tear if patients report persistent headaches or drainage after surgery.
Diagnostic tests may include:
- MRI: To look for fluid collections or pseudomeningoceles (small pockets of leaked fluid).
- CT myelogram: A specialized scan that uses dye to locate the site of the CSF leak.
Prompt diagnosis allows timely treatment and prevents complications such as infection or persistent leakage.
Classification
Dural tears can be classified by timing and size:
- Intraoperative tears: Found and repaired during surgery.
- Postoperative tears: Not noticed until after surgery, often presenting as CSF leakage.
- Small tears: May seal on their own with bed rest.
- Large tears: Require suturing or graft repair.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that can mimic dural tear symptoms include:
- Migraine or tension headaches
- Post-anesthesia headache
- Infection (meningitis or wound infection)
- Cerebrospinal fluid fistula from another source
Treatment Options
Non-Surgical Care
If a small dural tear is suspected but not severe, conservative treatment may be effective. This includes:
- Bed rest: Lying flat helps reduce fluid leakage and allows natural sealing.
- Hydration: Drinking fluids increases CSF production to restore balance.
- Pain relief medications: To ease headache and discomfort.
- Caffeine: Sometimes recommended to help alleviate spinal headaches.
Surgical Care
When leakage persists or the tear is large, surgical repair is required.
- Direct repair: The surgeon uses fine sutures to close the tear under magnification.
- Patch graft: A small piece of tissue or synthetic material is used to reinforce the repair.
- Sealants: Biological or synthetic glues may be applied for added watertight closure.
The repair is tested during surgery with a Valsalva maneuver, which gently increases pressure to ensure no fluid escapes.
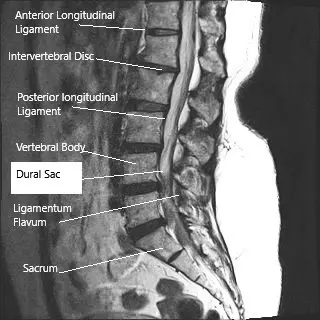
Sagittal section (MRI) of the lumbar spine showing dural sac.
Recovery and What to Expect After Treatment
After a dural tear repair, patients are typically advised to stay in bed for 24–48 hours to reduce CSF pressure on the repair site. Gradual sitting and walking follow, depending on symptom improvement. Most patients recover fully without long-term effects.
If symptoms such as headache or drainage recur, additional imaging or surgical revision may be necessary, but this is uncommon.
Possible Risks or Side Effects (Complications)
If a dural tear is not repaired or leaks persist, complications can include:
- Persistent spinal headache
- Fluid collection under the skin (pseudomeningocele)
- Infection such as meningitis
- Nerve irritation or pain
- Rarely, brainstem herniation due to loss of CSF pressure
Prompt identification and repair make these complications rare.
Long-Term Outlook (Prognosis)
The prognosis for patients with dural tears is excellent. Most recover without lasting problems, especially when the tear is recognized and repaired promptly. Long-term outcomes are similar to those of patients without a tear once healing is complete.
Out-of-Pocket Costs
Medicare
CPT Code 63710 – Dural Tear (Primary Repair): $265.18
CPT Code 63709 – Dural Repair with Graft: $274.27
CPT Code 63700 – Exploration of Spinal Cord or Canal: $331.47
Under Medicare, the program generally covers 80% of the approved costs for these spinal procedures once the deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield usually cover this coinsurance, effectively reducing or eliminating any out-of-pocket costs for Medicare-approved surgeries. These plans work directly alongside Medicare and are designed to close the financial gap for patients undergoing complex spine procedures such as dural repair.
If you have secondary insurance—such as Employer-Based Plans, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer after Medicare. Once your Medicare deductible is satisfied, secondary plans often pay the remaining balance, including co-insurance and minor uncovered costs. Most secondary plans have a small deductible, typically between $100 and $300, depending on your policy and whether your surgeon or facility is within the network.
Workers’ Compensation
If the dural tear occurred during or as a result of a work-related injury or surgery, Workers’ Compensation will fully cover all medical and surgical expenses, including dural repair, graft placement, or spinal canal exploration. Under this coverage, there are no out-of-pocket costs for the patient.
No-Fault Insurance
If the spinal injury or dural tear was sustained in a motor vehicle accident, No-Fault Insurance will cover all surgical and hospital-related expenses associated with the treatment. The only potential cost to you would be a small deductible based on your specific insurance policy terms.
Example
Maria, age 58, developed a dural tear during spinal decompression surgery that required primary repair (CPT 63710) and graft reinforcement (CPT 63709). Her estimated Medicare out-of-pocket costs were $265.18 and $274.27. Because Maria had supplemental insurance through Blue Cross Blue Shield, the remaining 20% not covered by Medicare was paid in full, leaving her with no out-of-pocket expense for her treatment.
Frequently Asked Questions (FAQ)
Q. Is a dural tear dangerous?
A. Most are not. When promptly repaired, patients recover completely without long-term issues.
Q. How long do I need to stay in bed after surgery?
A. Usually 1–2 days, depending on your surgeon’s protocol and symptom improvement.
Q. Can a dural tear heal on its own?
A. Small tears may seal naturally with rest and fluids, but larger ones need surgical repair.
Q. Will I have long-term headaches?
A. Persistent headaches are uncommon once the leak is closed and healing is complete.
Summary and Takeaway
A dural tear is a small hole in the protective covering of the spinal cord that can allow cerebrospinal fluid to leak. Although it can occur during spine surgery, it is typically repaired immediately and heals well. Most patients experience full recovery with proper rest and monitoring, and long-term complications are rare.
Clinical Insight & Recent Findings
A recent global survey of more than 900 spine surgeons evaluated how dural tears are managed during spinal surgery and the factors influencing complications. The study found that incidental dural tears occur in approximately 5–8% of spine surgeries, most commonly in lumbar procedures, with medium-sized tears (1–10 mm) being the most frequent.
Surgeons typically repaired these tears using Prolene sutures (77%) reinforced with fibrin glue or sealants (69%) and autologous grafts from fat or fascia (54%). Larger tears were often managed with 48 hours of bed rest, while smaller tears allowed for earlier ambulation. The most common complications were pseudomeningocele (60%) and cerebrospinal fluid (CSF) fistula (48%), though most surgeons reported them as rare or occasional.
Interestingly, surgeons with more than 16 years of experience had significantly fewer dural tears, while those working in public hospitals faced higher rates due to case complexity and limited resources. The authors concluded that although most dural tears can be effectively managed, standardized global protocols and randomized trials are needed to guide decisions regarding repair techniques and postoperative care. (Study of global practices in dural tear management – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Dural repair is performed by orthopedic spine surgeons or neurosurgeons experienced in microsurgical techniques, supported by anesthesiologists, nursing staff, and rehabilitation specialists.
When to See a Specialist?
You should consult a specialist if you have:
- Persistent headache after spine surgery
- Clear fluid drainage from a wound or nose
- Dizziness or nausea after spinal procedures
When to Go to the Emergency Room?
Seek emergency care if you experience:
- Severe, worsening headache when standing
- Fever, neck stiffness, or confusion (possible infection)
- New weakness, numbness, or loss of bladder control
What Recovery Really Looks Like?
Most patients rest for a few days and gradually return to normal activity within a week. Mild soreness or headache may persist briefly but resolves with healing.
What Happens If You Ignore It?
Untreated CSF leaks can lead to persistent headaches, infection, or neurological complications. Timely repair prevents these risks and ensures full recovery.
How to Prevent It?
While not all dural tears are preventable, careful surgical technique, magnification tools, and preoperative imaging reduce risk. Patients can support healing by following postoperative instructions closely.
Nutrition and Bone or Joint Health
Adequate hydration, balanced nutrition, and avoiding nicotine aid in tissue repair. Diets rich in protein, vitamin C, and zinc promote healing after surgery.
Activity and Lifestyle Modifications
After recovery, resume normal activities gradually. Avoid straining, heavy lifting, or sudden bending for several weeks. Proper posture and regular light exercise help maintain spinal health
Do you have more questions?
What is the function of the dura in the spine?
The dura mater is a protective membrane that surrounds the spinal cord and nerve roots, maintaining the cerebrospinal fluid (CSF) which cushions and nourishes these structures.
What are the common causes of dural tears during spine surgery?
Dural tears can be caused by inadvertent injury from surgical instruments, excessive retraction of tissues, or as a planned part of certain surgical procedures.
Why is cerebrospinal fluid (CSF) important?
CSF provides essential nutrients to the brain and spinal cord, acts as a cushion to protect against injury, and helps remove waste products from the central nervous system.
How are dural tears detected during surgery?
Dural tears can be detected by observing clear fluid leakage, using magnification tools, and performing tests like the Valsalva maneuver to identify any breaches.
What are the symptoms of a dural tear if it is not immediately detected during surgery?
Symptoms can include severe headaches, nausea, and sometimes clear fluid drainage from the surgical site, indicating a CSF leak.
How is a dural tear repaired during surgery?
Dural tears are repaired using very fine sutures and instruments under magnification to ensure a watertight seal. Synthetic grafts may be used if direct suturing is not feasible.
What materials are used if the dura cannot be directly sutured?
Synthetic grafts or local tissue grafts are used to reinforce or replace damaged dura, ensuring a watertight seal.
What is the Valsalva maneuver, and how is it used in dural repair?
The Valsalva maneuver involves the patient holding their breath and straining, which increases pressure in the thoracic and abdominal cavities, helping surgeons identify leaks in the dura.
What postoperative care is required for patients with dural tears?
Patients need to be on bed rest initially to monitor for CSF leaks. Gradual mobilization is attempted to ensure no recurrence of symptoms, with close follow-up care.
What are the long-term outcomes for patients who have had dural tears repaired?
Most patients recover well without significant long-term complications if the tear is promptly and properly repaired.
Can dural tears lead to serious complications if not managed properly?
Yes, if not managed properly, dural tears can lead to persistent CSF leaks, headaches, infections, and in severe cases, brain herniation.
Are there any preventive measures to avoid dural tears during spine surgery?
Surgeons can minimize the risk by using meticulous surgical techniques, employing advanced imaging, and ensuring proper instrument handling.
What role does magnification play in repairing dural tears?
Magnification, through microscopes or surgical loops, helps surgeons accurately suture the delicate dura and ensure a watertight repair.
How does a dural tear affect the recovery process compared to a surgery without complications?
Recovery may require additional bed rest and monitoring, but with proper management, long-term recovery is usually comparable to surgeries without complications.
What advancements in dural repair techniques are discussed in recent studies?
Recent advancements include the development of new suturing techniques, synthetic graft materials, and improved intraoperative monitoring methods.
Can dural tears recur after initial repair?
Recurrence is rare if the initial repair is successful, but ongoing symptoms or new CSF leaks should be promptly evaluated.
What are the signs of a successful dural repair?
Signs include the absence of CSF leaks, resolution of headaches, and normal neurological function without additional complications.
How is a CSF leak managed if it occurs after the patient has been discharged?
Management includes bed rest, hydration, and sometimes additional surgery to repair the leak if conservative measures fail.
How does bed rest help in the recovery of a dural tear?
Bed rest helps reduce pressure on the dura and allows time for the repair to heal, minimizing the risk of CSF leaks.
Are there specific risks associated with synthetic grafts in dural repair?
Risks include infection, rejection, and potential for the graft not integrating properly, although these are generally low with modern materials.
What follow-up care is necessary after a dural tear repair?
Follow-up care includes regular check-ups, monitoring for symptoms of CSF leaks, and ensuring the patient avoids activities that could stress the repair site.
What are the potential complications of a dural tear repair surgery?
Potential complications include infection, persistent CSF leaks, and neurological deficits, although these are uncommon with proper surgical technique.
Can dural tears be completely avoided during spine surgery?
While the risk can be minimized with careful surgical technique, dural tears cannot be completely avoided due to the complexity of spine surgeries.
How long does it typically take to recover from a dural tear repair?
Recovery time varies but generally spans a few weeks to a few months, depending on the severity of the tear and the patient’s overall health.

