Lumbar fusion surgery is a procedure designed to treat various lumbar spine conditions by fusing two or more vertebrae in the lower back. The goal of this surgery is to stabilize the affected segment, reduce pain, and prevent abnormal motion between the vertebrae, which could lead to further issues. The surgery is commonly used for treating conditions such as herniated discs, spinal deformities, and instability caused by degenerative disc disease or trauma. Various surgical techniques, including open and minimally invasive approaches, are employed to achieve spinal fusion.
How Common It Is and Who Gets It? (Epidemiology)
Low back pain (LBP) is one of the most common musculoskeletal disorders, affecting 70-85% of people at some point in their lives. Lumbar fusion surgery is particularly common among individuals with degenerative disc disease, spondylolisthesis, spinal stenosis, or other conditions that lead to spinal instability. The procedure is more frequent in older adults, especially those who have failed conservative treatments like physical therapy or medication.
Understanding Lumbar Fusion Surgery: A Comprehensive Guide
Lumbar fusion surgery is a procedure designed to address various spinal conditions by fusing two or more vertebrae in the lower back. This surgery aims to eliminate pain and instability by stopping motion between the affected vertebrae. Here, we will delve into the details of lumbar fusion, including its indications, techniques, and outcomes, using information from scientific studies and clinical experiences.
Why It Happens – Causes (Etiology and Pathophysiology)
Lumbar fusion is typically performed to treat conditions where the intervertebral discs between the vertebrae become damaged or degenerate. Causes of these issues include:
- Degenerative Disc Disease: The breakdown of intervertebral discs, often due to aging, results in decreased disc height and loss of cushioning.
- Herniated Discs: When the soft inner part of the disc bulges out and compresses surrounding nerves, causing pain, weakness, or numbness.
- Spinal Instability: Conditions such as spondylolisthesis, where one vertebra slips over another, causing instability and nerve compression.
- Spinal Stenosis: A narrowing of the spinal canal that puts pressure on the spinal cord and nerves.
How the Body Part Normally Works? (Relevant Anatomy)
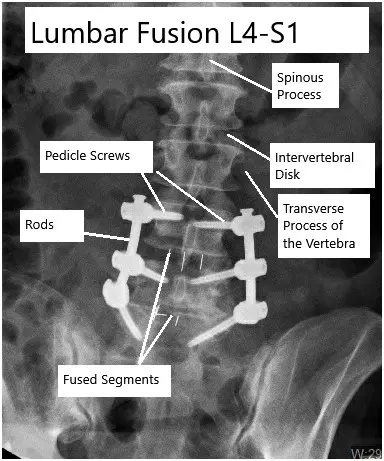
The lumbar spine consists of five vertebrae (L1-L5) that support the upper body and allow for movement and flexibility. Between these vertebrae are intervertebral discs, which act as shock absorbers and allow the spine to bend and move. The spine is also stabilized by muscles, ligaments, and other structures that provide support and maintain alignment. In lumbar fusion surgery, the discs between the vertebrae are often removed and replaced with a bone graft or artificial material to prevent movement between the affected vertebrae.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms that may indicate the need for lumbar fusion surgery include:
- Persistent Low Back Pain: Particularly in cases of degenerative disc disease or herniated discs.
- Radiating Pain: Pain that travels down the legs, often associated with sciatic nerve involvement.
- Weakness or Numbness: In the legs or feet, due to nerve compression.
- Difficulty Moving: Limited range of motion or difficulty standing, walking, or bending.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosing the need for lumbar fusion typically involves a thorough clinical examination, including physical tests to assess nerve function and mobility. Imaging studies such as X-rays, MRI, and CT scans are used to evaluate the condition of the discs, vertebrae, and spinal alignment. These images help determine the extent of degeneration, herniation, or instability in the spine.
Classification
Lumbar fusion procedures are typically classified based on the approach used:
- Anterior Lumbar Interbody Fusion (ALIF): Accessing the spine from the front.
- Posterior Lumbar Interbody Fusion (PLIF): Accessing the spine from the back.
- Transforaminal Lumbar Interbody Fusion (TLIF): A variant of PLIF that enters the spine at an angle.
- Lateral Lumbar Interbody Fusion (LLIF): Accessing the spine from the side.
Instrumentation and Stabilization
Instrumentation, such as screws and rods, is often used to stabilize the fusion site. Pedicle screws are a common choice, providing strong anchorage in the vertebrae. In minimally invasive techniques, these screws and rods can be inserted percutaneously, reducing tissue damage and promoting faster recovery.
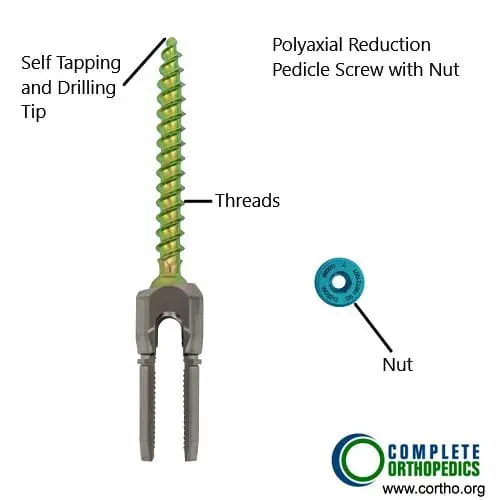
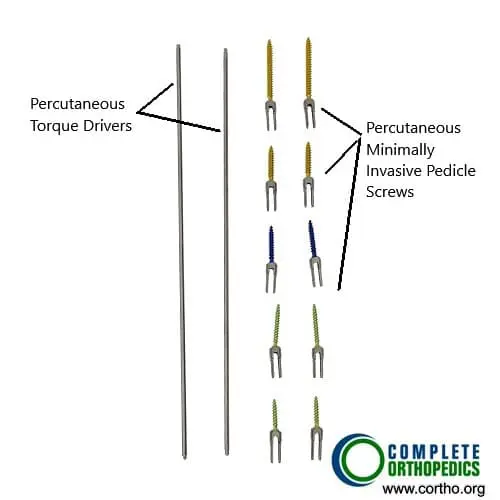
The images above show the pedicle screws used in minimally invasive lumbar fusion. The minimally invasive technique utilizes percutaneous insertion of pedicle screws and rods for fusion. The reduced cutting of the tissues results in earlier rehabilitation and reduced pain.
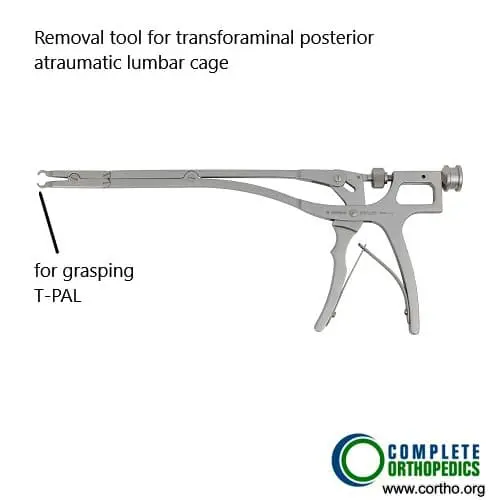
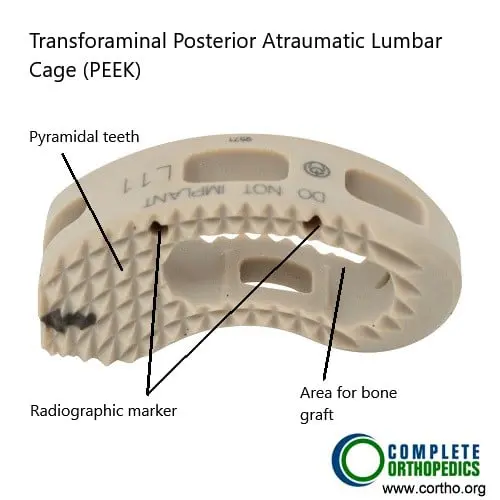
The T-PAL instrument and cage are used during performing traditional transforaminal lumbar interbody fusion. The transforaminal approach utilizes an incision at the side of the spinous process. The bone cage may be made of PEEK (poly-ether-ether-ketone) polymer with radiographical markers.
Combining Clinical and Scientific Knowledge
By integrating clinical knowledge with scientific insights, we can gain a comprehensive understanding of lumbar fusion surgery:
- Effectiveness: Lumbar fusion is highly effective in treating conditions like degenerative disk disease, spinal stenosis, and spondylolisthesis. Most patients experience significant pain relief and improved stability.
- Patient Selection: Careful patient selection is crucial. Not all patients with lower back pain are suitable candidates for lumbar fusion. Thorough evaluation and diagnostic imaging are essential to identify those who will benefit most.
- Surgical Precision: The success of lumbar fusion heavily relies on surgical precision. Proper placement of screws and rods, adequate preparation of the vertebral surfaces, and the use of appropriate graft materials are vital for successful fusion.
- Postoperative Care: Postoperative rehabilitation plays a significant role in recovery. Physical therapy and guided exercises help patients regain strength, flexibility, and function.
- Minimally Invasive Techniques: These techniques offer advantages such as reduced tissue damage, faster recovery, and lower complication rates. However, they require specialized training and expertise.
- Long-term Monitoring: Long-term follow-up is essential to monitor for potential complications like adjacent segment disease. Regular check-ups and imaging studies help detect and address issues early.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions that may mimic lumbar spine pain include:
- Piriformis Syndrome: Compression of the sciatic nerve by the piriformis muscle.
- Kidney Stones: Can cause lower back pain that may be mistaken for spinal issues.
- Muscle Strains: Common lower back injuries that can cause pain and stiffness.
- Osteoarthritis: Can lead to joint pain that radiates to the lower back.
Treatment Options
Non-Surgical Care
- Physical Therapy: To strengthen the back muscles and improve posture.
- Medications: Pain relievers like NSAIDs, corticosteroids, or muscle relaxants.
- Epidural Steroid Injections: To reduce inflammation and pain.
Surgical Care
- Lumbar Fusion Surgery: The primary surgical option when non-surgical treatments fail.
- Decompression Surgery: For conditions like spinal stenosis, to relieve pressure on the nerves.
Recovery and What to Expect After Treatment
After lumbar fusion surgery, patients typically begin walking within a day and may be discharged the same day or within a few days. Recovery focuses on:
- Physical Therapy: To regain strength, mobility, and function.
- Activity Restrictions: Avoiding heavy lifting or strenuous activities during recovery.
- Follow-up Care: To monitor fusion progress and detect any complications.
Possible Risks or Side Effects (Complications)
Possible complications include:
- Infections: At the surgical site or deeper within the spine.
- Blood Clots: Particularly in the legs (deep vein thrombosis).
- Implant Failure: In the case of hardware breakage or malfunction.
- Adjacent Segment Degeneration: Damage to neighboring vertebrae due to altered motion patterns.
- Failed Fusion (Nonunion): When the vertebrae do not properly fuse.
Long-Term Outlook (Prognosis)
The success rate of lumbar fusion is high, with most patients experiencing significant pain relief and improved mobility. However, some patients may continue to experience discomfort or develop adjacent segment degeneration over time. Regular follow-ups and imaging are essential to monitor long-term outcomes.
Out-of-Pocket Costs
Medicare
CPT Code 22558 – Anterior Lumbar Interbody Fusion (ALIF) / Lateral Lumbar Interbody Fusion (LLIF): $368.50
CPT Code 22630 – Posterior Lumbar Interbody Fusion (PLIF) / Transforaminal Lumbar Interbody Fusion (TLIF): $387.42
CPT Code 22612 – Posterior Lumbar Fusion (PLF): $382.85
Under Medicare, 80% of the approved cost for these procedures is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved lumbar fusion surgeries. These supplemental plans work directly with Medicare to ensure full coverage for ALIF, LLIF, PLIF, TLIF, and posterior lumbar fusion procedures.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it functions as a secondary payer once Medicare has processed the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, ranging from $100 to $300, depending on the specific policy and network status.
Workers’ Compensation
If your lumbar spine condition requiring fusion surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, instrumentation, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your lumbar spine injury resulting in fusion surgery is caused by a motor vehicle accident, No-Fault Insurance will pay for all medical and surgical expenses, including ALIF, LLIF, PLIF, TLIF, and posterior lumbar fusion. The only possible out-of-pocket cost may be a small deductible depending on your policy terms.
Example
Emily, a 64-year-old patient with lumbar instability, required anterior lumbar interbody fusion (ALIF, CPT 22558) and posterior lumbar interbody fusion (PLIF, CPT 22630) to relieve her pain and stabilize her spine. Her estimated Medicare out-of-pocket costs were $368.50 for the ALIF and $387.42 for the PLIF. Since Emily had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving her with no out-of-pocket expenses for her surgeries.
Frequently Asked Questions (FAQ)
Q. What is the recovery time for lumbar fusion surgery?
A. Recovery typically takes several months, with most patients returning to normal activities within 6-12 months.
Q. How long do the results of lumbar fusion last?
A. Most patients experience long-term pain relief, though adjacent segment degeneration can occur over time.
Q. Will I be able to walk after lumbar fusion surgery?
A. Yes, most patients begin walking soon after surgery and gradually increase activity as they recover.
Summary and Takeaway
Lumbar fusion surgery is a vital option for patients suffering from spinal conditions that lead to chronic pain or instability. By fusing vertebrae to stop motion and improve stability, the procedure offers significant pain relief and improves the patient’s quality of life. Advances in minimally invasive techniques have further enhanced recovery times and reduced risks.
Clinical Insight & Recent Findings
A recent study explored the factors contributing to short-term residual pain following posterior lumbar interbody fusion (PLIF) surgery, identifying key risk factors such as the condition of paraspinal muscles and psychological factors.
The study utilized machine learning models to predict postoperative pain, revealing that lower psoas muscle index (PMI), lower multifidus muscle index (MMI), and higher levels of anxiety were significant predictors of residual pain. Furthermore, the study found that patients with better muscle condition and psychological status, along with lower surgical segments, experienced less residual pain.
These findings highlight the importance of addressing muscle health and psychological well-being to optimize surgical outcomes and reduce postoperative pain. (“Study on predicting short-term pain after PLIF surgery – see PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Lumbar fusion surgery is performed by spine surgeons who specialize in spinal conditions and surgery. This team may include:
- Orthopedic Surgeons: Specializing in bones and joints.
- Neurosurgeons: Specializing in the nervous system and spine.
- Anesthesiologists: For managing anesthesia during the procedure.
- Physical Therapists: To assist in post-surgery rehabilitation.
When to See a Specialist?
If you experience chronic back pain, radiating leg pain, or weakness in the lower limbs, it is important to consult with a specialist to determine if lumbar fusion surgery is appropriate for your condition.
When to Go to the Emergency Room?
Seek immediate medical attention if you experience:
- Sudden loss of bladder or bowel control.
- Severe pain that does not respond to medication.
- Numbness or weakness that affects mobility.
What Recovery Really Looks Like?
Most patients experience significant pain relief and increased stability after lumbar fusion surgery. However, full recovery can take months, and physical therapy is crucial for regaining strength and flexibility.
What Happens If You Ignore It?
Ignoring symptoms of lumbar instability or herniated discs can lead to worsening pain, nerve damage, and permanent disability. Early intervention with surgery often leads to better outcomes.
How to Prevent It?
Maintaining a healthy weight, engaging in regular exercise to strengthen the back muscles, and avoiding heavy lifting or sudden movements can help prevent conditions that may lead to lumbar fusion surgery.
Nutrition and Bone or Joint Health
Eating a diet rich in calcium and vitamin D can support bone health and reduce the risk of degenerative spinal conditions. Proper hydration and nutrition also help in the recovery process after surgery.
Activity and Lifestyle Modifications
After surgery, patients are encouraged to engage in light physical activity, such as walking or swimming, to enhance recovery. Avoiding heavy lifting and high-impact activities is essential during the early stages of recovery.
Do you have more questions?
If I have Spondylolisthesis, will it be reduced?
Spondylolisthesis or slipping of one vertebra over the other are usually taken care by the surgery if it fails to give relief with conservative means. It is not necessary to get them 100% reduced, but the most important part is to relieve the neural elements of all the pressure, which is caused either by the bony vertebrate or the disc and prepare the vertebrae for fusion. In case of lumbar spine, spondylolisthesis need not to be reduced fully 100%, especially if the patient has a high grade listhesis, it is not desirable to reduce it completely. An important part of surgery is to clean the pressure of the spinal and nerve roots and prepare a healthy environment for bones to fuse.
How soon after the surgery can I start physical therapy?
Patients are not required to start their physical therapy till two weeks after the surgery. After two weeks of surgery, physician reexamination will help in deciding if the patient requires physical therapy or not. Many of the patients do not require physical therapy after the surgery.
Does smoking cause spine problems?
Smoking has proven to cause spine problems, including neck and lower back. At the same time, smoking is detrimental for patients who require spine surgery, especially fusion surgeries. It has been shown that smoking delays spine fusion, as well as lead to higher incidence of nonunion and possible need for revision surgeries.
Do I have to give up smoking?
For patients undergoing fusion surgery, it is highly desirable that they quit smoking. Smoking is detrimental for bone healing and hence the fusion. Smokers are at a higher risk of nonunion, that means non healing of the fusion mass, and these patients may need revision surgery. If the patient is not able to quit smoking, it is at least highly desirable for them to quit for three months. Use of the nicotine patch in place of smoking has the same detrimental effect as smoking itself.
What if, during my surgery, you encounter a different issue other than expected?
Usually, before the surgery, we discuss with the patient regarding all the possible spine issues that we may expect and how to manage them. If there is an unexpected issue, which has not been discussed earlier, we would go ahead and discuss it with the patient’s relative and treat it accordingly from there. If there is something which can wait, and is not detrimental to the patient, and relatives are not able to make decision on it, we may leave it for a later date to be discussed with the patient after the surgery.
How long is it possible to stay for back surgery?
Most of the patients with back surgery can be discharged within one to four days after the surgery depending on the type of surgery and the type of recovery that they have. Patients who undergo complex spine surgeries may need longer period of hospitalization and recovery.
Which pain medications will I be sent home with? What are the possible side-effects of these prescriptions?
Most of the patients with cervical spine surgery, will be sent with some narcotic pain medication to take care of their pain. These medications do have their multiple side-effects, which may be constipation, nausea, vomiting, impaired judgement, drowsiness, headache. Though patients who are treated with narcotic pain medication for acute pain, mostly do not lead to addiction, but these medications do have addiction potential.
Will you know before the surgery if I need a brace afterwards? If so, will I be fitted for one before the surgery?
Most of the patients with spine surgery do not need a brace. If we expect that the patient will need a brace, we will get the patient pre-fitted with a brace so that it is available immediately after the surgery. Occasionally the need for brace may be decided at the time of surgery. In such cases a brace is arranged in immediate post-operative period.
Will I need any other medical equipment like a walker when I go home? Should I get an adjusted bed or sleep downstairs?
Patient may need other medical equipment like walker or a stick. If that is required, patients are provided with such equipment in the hospital before their discharge and are trained how to use them by the physical therapist and occupational therapist. If the patient needs to use stairs, patients are trained by the physical therapist before they are let go home. If the patient needs an adjustable bed, they are informed about that. That can be done prior to the surgery. It is desirable for patients to stay downstairs for a few weeks if possible.
Who can I call if I have questions after the surgery?
In case patient has routine questions regarding after the surgery or regarding the surgery, they can call the physician’s office and talk to the nurse or secretary or the physician. If they’re not available on the phone, they can leave a voice mail and they will be answered later. In case the patient has a medical emergency, then they should not call the physician office but rather call 911 or get to the hospital ER as soon as possible.
How often will I see you after my surgery?
Patients are usually followed at two weeks, six weeks, three months, six months, and a year after surgery.
What symptoms would warrant a call to your office after the surgery?
If the patient develops problems like chest pain, breathing problems, sudden neurological deterioration, or any other emergency they should call 911, or go to the emergency room directly. Patients who develop worsening pain at the surgery site, discharge from the wound, fever; they should call in the office.
How long should I wait to bathe after the surgery?
Patients are usually asked to avoid bathing, until the incision heals, which may take two to three weeks. Patient can take shower after 72 hours of surgery with an impervious dressing in place. The dressing can be changes if the wound is visibly soaked. Patients are asked not to rub the area of surgery for about two to three weeks. They can gently dab it dry with a towel.
How long will I be out of work?
Patients with low demand work and desk job, can be back to work as soon as three to six weeks after the surgery depending on patient pain control as well as recovery. Patients who are in heavy lifting or control of heavy machinery or handyman job, may take three to four months, or even more to get back to work depending on their recovery from the surgery.
How soon after the surgery can I start physical therapy?
Patients after back surgery are usually started on physical therapy, if they need, depending on physician’s advice, at two to four weeks after the surgery. Many of the patients do not need physical therapy. A decision to go into physical therapy will depend on the surgery as well their recovery.
What if I get an infection?
If the patient has a superficial infection, few days of antibiotics will help heal these infections. Occasionally patient may develop deep infection. In these patients may need IV antibiotics for a longer period. If despite all efforts or in patients with rapid deterioration due to infection, surgery may be needed to help clean off the infection.
How common is surgery?
Most of the patients do not need surgery and can be treated with conservative means. When the patients do not respond to conservative measures, or if they have worsening neurological deficit, or worse pain, they may need surgery.
Will I have irreversible damage if I delay surgery?
Patients who develop neurological deficit in the form of weakness or involvement of bowel or bladder may have irreversible damage if the surgery is delayed enough.
When do I need fusion?
When patient has back pain or has a surgery in which enough bone is removed to destabilize the spine, in these cases patient may need a fusion surgery to stabilize the spine, as well as to alleviate the symptoms.
What are my risks of low back surgery?
General surgical risks of low back surgeries include bleeding, infection, persistence of pain, reversible/irreversible nerve damage leading to tingling, numbness, or weakness down the legs or involvement of bowel or bladder, failure of resolution of symptoms, failure of fusion, failure of implants. Most of the patients can undergo a safe surgery due to the development of vision magnification as well as refined surgical techniques. There are anesthesia risks also associated with this surgery.
When will I be back to my normal activities?
Though these things depend on the type of surgery patient has undergone, patient can usually be progressively back to their normal activities, starting from three to five days from surgery. Patients are encouraged to take care of their activities of daily living, as well as light household activities. Patients can get back to driving once they are free from pain medication and are able to sit for a duration of period for driving, which may take upto 2-3 weeks or more.
What type of surgery is recommended?
The type of surgery depends on the presenting complaint, examination findings, as well as imaging findings in the form of x-ray and MRI. Some patients may need to undergo just discectomy, or laminectomy, while others may need a fusion surgery on their back to relieve their symptoms. To know more about the type of surgery, the patient needs to discuss this with their spine surgeons.
How long will the surgery take?
Spine surgeries like discectomy and laminectomy usually last about one to one and a half hours. Spine fusion surgeries, may take longer periods, up to two and a half to four hours or more. It depends on type of surgery, and as well as the level of spine to be operated upon.
What is degenerative disc disease?
Degeneration means gradual damage of the tissue. Degenerative disc disease represents aging of the disc, either appropriate to the normal age of the patient, or maybe accelerated due to injury or chronic disease, or other factors like smoking, obesity.
What is Lumbar instability?
Lumbar instability means that the spine is not stable and there is excessive abnormal movement between two vertebrae. This is usually diagnosed by imaging in the form of X-rays, CT scan, or MRI of the patients. Instability may lead to compression of nerve roots causing radiculopathy with or without back pain.
What is Spinal Stenosis?
Spinal Stenosis means narrowing of the spinal canal. It is can be at the cervical or thoracic or lumbar level. Most common spinal stenosis is at lumbar level and it, when narrowed, can compress nerves, causing pain going down the legs, with or without tingling, numbness, weakness, or involvement of bowel or bladder.
What is Sciatica?
Sciatica is another name for lumbar radiculopathy, in which patient has pain going down their legs. The pattern of pain depends on the nerve root involved, but the most common is pain going down the outer side of the thigh and leg into the foot.
What is lumbar disc disease? How is this problem diagnosed?
The diagnosis of Lumbar disc disease is made by history and examination of the patient. The confirmation of diagnosis is done by imaging in the form of X-rays and MRI. Occasionally the patient is having contraindication to MRI, patient may need to undergo a CT scan. When a CT scan is done, occasionally the patient may need to get injected with a dye before the CT scan and this is called CT myelography. Occasionally patient may need a CT scan along with MRI also.
When should I consider surgery for the back pain?
Most of the patients get treated with conservative means. In case the patient is not getting relief despite continuous conservative measures, or if there is worsening of pain associated with or without weakness or involvement of bowel or bladder, the patient may need surgical intervention in the form of surgery.
Am I a candidate for minimal-invasive spine surgery?
Some patients are good candidates for minimally-invasive spine surgery and they can get better with that. History, physical examination, as well as special investigations like X-ray and MRI, are needed in order to discuss regarding options of minimal invasive spine surgery. Some patients are not good candidates for minimal invasive spine surgery and doing such a surgery in such patients may lead to non-resolved solution of the symptoms or worsening.
Are there any warning symptoms?
Warning symptoms of lumbar disc disease include worsening pain, tingling and numbness, development of weakness, or worsening of weakness, involvement of bowel or bladder in the form of incontinence of urine or stools, presence of fever, unintentional weight loss. In such conditions patients should immediately seek medical attention.
Do you need any tests?
General blood workup is needed in most patients before the surgery. This will include blood counts as well as metabolic profile. Special tests may be needed in some patients if the physician has suspicion of some other disease. Most of the patients will have to undergo X-ray and MRI, or a CT scan before the surgery to confirm their diagnosis.
What are the possible surgical complications from a low back surgery?
Common complications of a low back spine surgery are bleeding, infection, leak of cerebral spinal fluid temporary or permanent neurological deficits, blindness, worsening of pain, failure of fusion, failure of implants. There may be risks due to the anesthesia also.
What is spine stabilization?
Spine stabilization involves insertion of screws, rods, or plate to stabilize a spine. This surgery may be associated with fusion of the spine to be it a long-term solution to the instability of the spine. Call Us Now! (631) 981-2663 On your phone? Tap here to text us! Lumbar Spine Service Lumbar Spine Surgery Lumbar Fusion Surgery Lumbar Laminectomy Surgery Lumbar Disc Replacement Minimally Invasive Lumbar Fusion Anterior Lumbar Interbody Fusion Surgery Lumbar Hemilaminectomy Surgery Posterior Lumbar Interbody Fusion Surgery Prevention of Surgical Site Infections in Adult Spine Surgery Postoperative Management Protocol for Incidental Dural Tears During Degenerative Lumbar Spine Surgery Optimizing Spine Surgery Outcomes: Enhanced Recovery After Surgery (ERAS) IPD for Treatment of Degenerative Lumbar Spine Stenosis Computer-Based Techniques for Spine Analysis in MRI Development of Full-Endoscopic Lumbar Spine Surgery Recent Advances in Spine Surgery Non-fusion Surgeries of Lumbar Spine Laminectomy and Minimal Invasive Decompression Spondylolisthesis at L4-5 treated by XLIF Consecutive Multilevel Vertebral Paget’s Disease of the Lumbar Spine: Differential Diagnosis Bone Healing Strategies for Lumbar Interbody Fusion Advances in Surgical Techniques for Lumbar Interbody Fusion ALIF and OLIF: Spinal Fusion Transforaminal Lumbar Interbody Fusion (TLIF) COVID-19 and Spine Surgery Incorporating Posterior Interbody Fusion into Surgical Interventions for Degenerative Lumbar Spine Conditions Kyphoplasty versus Vertebroplasty in Osteoporotic Thoracolumbar Spine fractures Kyphoplasty and Vertebroplasty for Osteoporotic Thoracolumbar Spine Fractures Assessing Classification Systems for Thoracolumbar Spine Trauma Assessment of Thoracolumbar Spine Injuries using Medical Imaging Prolapsed Intervertebral Disk (PIVD) Osteoporotic Vertebral Compression Fractures

