Lumbar hemilaminectomy is a minimally invasive surgical procedure designed to relieve pressure on the spinal nerves caused by conditions like spinal stenosis or disc herniation. This surgery removes a small portion of the lamina (the roof of the spinal canal) to provide space and reduce nerve compression, offering relief from pain and other symptoms in the lumbar spine.
How Common It Is and Who Gets It? (Epidemiology)
Lumbar spine issues are prevalent, with back pain affecting a significant portion of the population, particularly in adults over 40 years of age. Conditions that lead to lumbar nerve compression, such as spinal stenosis and herniated discs, are common in older individuals, particularly those with age-related wear and tear or trauma to the spine.
Why It Happens – Causes (Etiology and Pathophysiology)
Several factors contribute to the need for lumbar hemilaminectomy surgery:
- Spinal Stenosis: Narrowing of the spinal canal, causing compression of the spinal cord or nerve roots.
- Herniated Discs: The intervertebral discs bulge or rupture, pressing on nerves in the lumbar spine.
- Bone Spurs: Overgrowth of bone due to age or injury, narrowing the space for nerves.
- Thickened Ligamentum Flavum: Thickening of the ligament can lead to compression of the spinal cord.
How the Body Part Normally Works? (Relevant Anatomy)
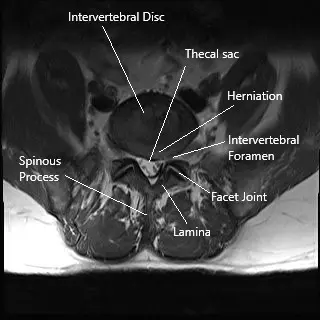
The lumbar spine consists of five vertebrae (L1 to L5) that support the lower back. The spinal cord passes through the spinal canal, and nerves branch out from the spinal cord, exiting through foramina to provide sensation and motor function to the lower extremities. The lamina forms part of the roof of the spinal canal, protecting the spinal cord and nerves.
What You Might Feel – Symptoms (Clinical Presentation)
Patients with conditions requiring lumbar hemilaminectomy surgery often experience:
- Back pain that may radiate into the buttocks or legs.
- Sciatica-like symptoms: Pain radiating down the thighs or legs.
- Numbness or tingling in the lower extremities.
- Weakness or difficulty walking, especially when bending backward or walking downhill.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis typically involves:
- Physical Examination: To assess pain and neurological function.
- MRI or CT Scan: To evaluate the spinal canal, identify herniated discs, bone spurs, or stenosis, and assess the extent of nerve compression.
- X-rays: To check for bone deformities or alignment issues.
- Electromyography (EMG): To test nerve function and identify damage.
Hemilaminectomy/Laminotomy: A Minimally Invasive Option
Hemilaminectomy/laminotomy is a surgical procedure used to relieve pressure on the spinal cord and nerves. Unlike a full laminectomy, which involves removing a larger portion of the lamina (the roof of the spinal canal), a hemilaminectomy removes only a small part, making it less invasive.
However, not all patients are candidates for hemilaminectomy. Patients with extensive involvement and compression may benefit from laminectomy surgery or lumbar fusion surgery.
Procedure Overview
Preparation: The surgery is performed under general anesthesia. The patient lies face down on the operating table.
Incision: A small incision is made in the back to access the affected area.
Muscle Retraction: The paraspinal muscles are gently moved aside to expose the spine.
Removal of Lamina: Using specialized instruments, the surgeon removes a portion of the lamina and may also remove parts of the thickened ligamentum flavum or herniated disc material.
Closure: The incision is closed in layers, and a sterile dressing is applied.
Classification
Lumbar hemilaminectomy can be classified as:
- Unilateral Hemilaminectomy: Removal of a portion of the lamina on one side of the spine.
- Bilateral Hemilaminectomy: Removal of a portion of the lamina on both sides of the spine (less common).
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that can mimic lumbar nerve compression include:
- Piriformis Syndrome: Compression of the sciatic nerve by the piriformis muscle.
- Hip Arthritis: Can cause referred pain to the lower back or buttocks.
- Muscle Strains: Often mistaken for spinal issues when the pain radiates down the legs.
- Kidney Stones: Can cause pain in the lower back that may be confused with spinal conditions.
Treatment Options
Non-Surgical Care
- Physical Therapy: Strengthening back muscles and improving flexibility.
- Pain Medications: Including NSAIDs, corticosteroids, and muscle relaxants.
- Epidural Injections: To reduce inflammation and alleviate pain.
- Nerve Blocks: To target specific pain areas and reduce symptoms.
Surgical Care
- Hemilaminectomy: A minimally invasive option for relieving pressure on spinal nerves.
- Laminectomy: A more extensive surgery where a larger portion of the lamina is removed.
- Lumbar Fusion: For cases with spinal instability or deformity requiring stabilization.
Recovery and What to Expect After Treatment
Post-operative care typically involves:
- Pain Management: Using medications to control discomfort.
- Physical Therapy: To restore strength, flexibility, and function.
- Activity Restrictions: Avoiding heavy lifting or high-impact activities for several weeks.
- Follow-up Visits: To monitor healing and assess for any complications.
Patients generally recover within a few weeks, with most resuming normal activities in 4-6 weeks.
Possible Risks or Side Effects (Complications)
Potential risks include:
- Incomplete Decompression: The surgery may not fully alleviate symptoms.
- Nerve Damage: There is a risk of damaging the nerves or spinal cord.
- Durotomy: Unintentional tearing of the dura mater (the outer membrane surrounding the spinal cord).
- Infection and Bleeding: Common risks associated with any surgery.
Long-Term Outlook (Prognosis)
The prognosis for most patients undergoing hemilaminectomy is positive, with significant pain relief and improved mobility. However, some patients may experience recurring symptoms or complications, especially if they have underlying spinal instability.
Out-of-Pocket Cost
Medicare
CPT Code 63047 – Lumbar Hemilaminectomy Surgery: $271.76
Under Medicare, 80% of the approved cost for this procedure is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—usually cover this 20%, leaving most patients with little to no out-of-pocket expenses for Medicare-approved spine surgeries like hemilaminectomy. These supplemental plans coordinate directly with Medicare to ensure full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare processes the claim. After your deductible is satisfied, the secondary plan may cover any remaining balance, including coinsurance or any uncovered charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on the specific policy and network status.
Workers’ Compensation
If your lumbar condition requiring hemilaminectomy surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including the surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your lumbar spine injury is the result of a motor vehicle accident, No-Fault Insurance will cover the full cost of the surgery. The only potential out-of-pocket cost would be a small deductible depending on your individual policy terms.
Example
James, a 60-year-old patient with lumbar stenosis, underwent lumbar hemilaminectomy (CPT 63047) to decompress the spinal cord and relieve his symptoms. His estimated Medicare out-of-pocket cost was $271.76. Since James had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. How long is the recovery after lumbar hemilaminectomy surgery?
A. Most patients recover within a few weeks, with physical therapy recommended for strengthening and flexibility.
Q. Can I go back to work after the surgery?
A. Most patients can return to work within 4-6 weeks, depending on the nature of their job and the extent of their recovery.
Q. Will my symptoms return after surgery?
A. While many patients experience long-term relief, some may have recurrence if there is ongoing spinal instability or degeneration in other segments.
Summary and Takeaway
Lumbar hemilaminectomy offers a minimally invasive solution for relieving pressure on spinal nerves caused by conditions like stenosis and disc herniation. The procedure has a high success rate, providing significant pain relief with a relatively quick recovery time. However, it may not be suitable for all patients, particularly those with extensive spinal issues, in which more invasive options may be required.
Clinical Insight & Recent Findings
A recent study analyzed the use of hemilaminectomy in treating intervertebral disc disease and diskospondylitis in an aardvark, demonstrating its potential in animal models. The procedure aimed to relieve spinal cord compression caused by disk herniation, though anatomical challenges in this species required significant adjustments in surgical technique.
The aardvark showed initial improvement post-surgery but experienced complications, including wound dehiscence and persistent infection. Despite intensive rehabilitation and antimicrobial treatment, the animal’s condition worsened due to progressive diskospondylitis, ultimately leading to euthanasia.
This case underscores the challenges of performing complex spinal surgeries in non-domestic animals, while contributing valuable insights for similar future treatments. (“Study of hemilaminectomy for diskospondylitis in an aardvark – see PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Hemilaminectomy surgery is typically performed by:
- Spine Surgeons: Orthopedic or neurosurgeons specializing in spinal conditions.
- Anesthesiologists: To manage anesthesia during the procedure.
- Physical Therapists: To assist in post-operative rehabilitation.
When to See a Specialist?
If you experience persistent back pain, radiating leg pain, numbness, or weakness in the lower extremities, it is essential to consult a spine specialist to determine if hemilaminectomy surgery is appropriate.
When to Go to the Emergency Room?
Seek emergency care if you experience:
- Sudden loss of bladder or bowel control.
- Severe pain that does not respond to medication.
- New or worsening neurological symptoms such as weakness or numbness in the legs.
What Recovery Really Looks Like?
Post-surgery, most patients experience relief from pain and can begin walking soon after. Rehabilitation typically lasts a few weeks, with gradual increases in activity levels.
What Happens If You Ignore It?
Ignoring symptoms can lead to worsening pain, potential nerve damage, and loss of function. Early intervention with surgery often leads to better outcomes and a faster recovery.
How to Prevent It?
Maintaining a healthy weight, engaging in regular back-strengthening exercises, and avoiding activities that put excessive strain on the lower back can help prevent conditions leading to lumbar hemilaminectomy.
Nutrition and Bone or Joint Health
A diet rich in calcium and vitamin D can support bone health and prevent spinal degeneration. Proper hydration and balanced nutrition are also essential for recovery.
Activity and Lifestyle Modifications
After surgery, patients should engage in light physical activities such as walking or swimming. Avoid heavy lifting and high-impact activities to allow for healing and prevent re-injury.
Do you have more questions?
How do I know if I’m a candidate for hemilaminectomy?
Candidates for hemilaminectomy typically have symptoms of nerve compression such as back pain, leg pain, numbness, and difficulty walking that haven’t improved with conservative treatments like physical therapy or medications.
What are the potential benefits of a hemilaminectomy over a full laminectomy?
Hemilaminectomy is less invasive, involves a smaller incision, and generally results in a quicker recovery time with less postoperative pain.
How long does the surgery usually take?
A hemilaminectomy typically takes about 1 to 2 hours, depending on the complexity of the case and the specific area being treated.
What kind of anesthesia is used during hemilaminectomy?
The surgery is performed under general anesthesia, meaning you will be asleep and pain-free during the procedure.
What is the recovery process like after hemilaminectomy?
Recovery includes an overnight hospital stay, pain management, wound care, and physical therapy. Most patients can return to normal activities within a few weeks.
Are there any dietary restrictions before or after the surgery?
Generally, you may be advised to avoid eating or drinking after midnight before the surgery. Postoperatively, a balanced diet helps in recovery, but specific restrictions are usually not necessary unless advised by your surgeon.
What are the risks of hemilaminectomy?
Risks include infection, bleeding, nerve damage, incomplete decompression, and dural tears. These complications are relatively rare but possible.
How soon can I return to work after hemilaminectomy?
This depends on your job and how quickly you recover. Patients with sedentary jobs may return in 2-4 weeks, while those with physically demanding jobs might need 6-8 weeks.
How effective is hemilaminectomy in relieving symptoms?
Hemilaminectomy is generally very effective in relieving symptoms of nerve compression, with most patients experiencing significant pain relief and improved function.
Can the symptoms return after surgery?
While hemilaminectomy provides long-term relief for many, there is a chance that symptoms can return if new areas of compression develop or if there is recurrent disc herniation.
What should I do if I experience new or worsening symptoms after surgery?
Contact your surgeon immediately if you experience new or worsening symptoms, as this could indicate a complication that needs prompt attention.
Is there anything I can do to prevent spinal problems in the future?
Maintaining a healthy weight, regular exercise, good posture, and avoiding activities that strain your back can help prevent future spinal issues.
Can I drive after the surgery?
You should avoid driving until you have stopped taking narcotic pain medications and feel comfortable sitting and turning your body, which is usually after a couple of weeks.
Will I have a scar after the surgery?
Yes, there will be a small scar where the incision was made, but it typically fades over time.
How soon can I start exercising after hemilaminectomy?
Light activities and walking can start soon after surgery, but strenuous exercises and heavy lifting should be avoided for at least 6-8 weeks. Follow your surgeon’s recommendations.
Will I need to wear a brace after the surgery?
This depends on the individual case. Some patients may be advised to wear a brace for additional support, but it is not always necessary.
What happens if I need another surgery in the future?
If further surgery is needed, your surgeon will discuss the best options based on your current condition and previous surgeries.
Can hemilaminectomy be performed on multiple levels of the spine?
Yes, hemilaminectomy can be performed on multiple levels if necessary, although the complexity and recovery time may increase.
How do bone spurs contribute to spinal stenosis?
Bone spurs, or osteophytes, can form due to arthritis and other degenerative changes. They can narrow the spinal canal and compress the nerves, contributing to spinal stenosis.
Is hemilaminectomy effective for treating herniated discs?
Yes, hemilaminectomy can be effective in relieving symptoms caused by herniated discs by removing the part of the disc that is compressing the nerve.
What is the role of the ligamentum flavum in spinal stenosis?
The ligamentum flavum can thicken and lose elasticity with age, which can narrow the spinal canal and contribute to nerve compression.
What are the signs of a successful hemilaminectomy?
A successful hemilaminectomy is indicated by significant pain relief, improved mobility, and the absence of neurological symptoms like numbness or weakness.
What follow-up care is necessary after a hemilaminectomy?
Follow-up care includes regular check-ups with your surgeon, adherence to physical therapy, and monitoring for any signs of complications. You will be given specific instructions tailored to your recovery needs.

