Cervical microdiscectomy is a minimally invasive surgical procedure used to treat cervical radiculopathy, a condition caused by compression of the cervical nerve roots, often due to a herniated intervertebral disc. The surgery aims to relieve nerve compression by removing the herniated disc material, helping to alleviate symptoms such as pain, numbness, and weakness in the upper extremities. This procedure is typically recommended when conservative treatments have failed.
How Common It Is and Who Gets It? (Epidemiology)
Cervical radiculopathy affects a significant number of people, particularly those between the ages of 30 and 50, with a higher incidence in individuals who engage in physical labor or repetitive motions. It is more common in individuals with age-related degenerative changes in the spine, but traumatic injuries such as falls or accidents can also lead to disc herniation and nerve compression. Approximately 10-20% of individuals with cervical disc herniation may require surgical intervention like microdiscectomy.
Why It Happens – Causes (Etiology and Pathophysiology)
Cervical radiculopathy occurs when a herniated disc or other spinal conditions compress the nerve roots exiting the cervical spine. Common causes include:
- Degenerative Disc Disease: The natural breakdown of discs with age, leading to a herniation of the disc’s inner nucleus.
- Traumatic Injury: Accidents or falls that cause a disc to herniate, putting pressure on the nerve roots.
- Bone Spurs: Overgrowth of bone around the discs, which can cause narrowing of the spaces where the nerves exit.
- Herniated Discs: The inner nucleus of a disc protrudes through the outer layer, pressing on the nerve root.
This pressure causes nerve irritation and inflammation, leading to the hallmark symptoms of radiculopathy: pain, numbness, tingling, and weakness in the arms, hands, and sometimes the neck.
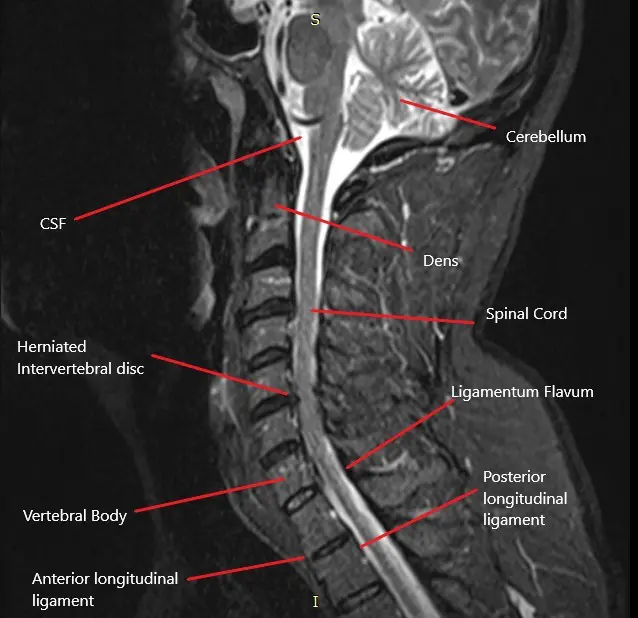
How the Body Part Normally Works? (Relevant Anatomy)
The cervical spine consists of seven vertebrae (C1-C7) in the neck region. Between each vertebra is an intervertebral disc that cushions and allows movement between the bones. The spinal cord passes through the central spinal canal, and nerves branch out from the spinal cord through the foramina (openings) in each vertebra. These nerves control sensation and movement in the shoulders, arms, hands, and other areas of the upper body. When a disc herniates, it can compress one or more of these nerves, leading to cervical radiculopathy.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of cervical radiculopathy often include:
- Neck Pain: Pain localized in the neck or radiating to the shoulders.
- Radiating Pain: Sharp or burning pain that travels from the neck down into the shoulder, arm, or hand.
- Numbness or Tingling: A sensation of “pins and needles” in the upper extremities.
- Weakness: Difficulty gripping objects, weakness in the arms, or clumsiness in the hands.
- Loss of Reflexes: Reduced reflexes in the affected arm.
How Doctors Find the Problem? (Diagnosis and Imaging)
The diagnosis of cervical radiculopathy involves:
- Physical Examination: A spine surgeon will assess the patient’s neck mobility, reflexes, and strength to identify nerve involvement.
- MRI: The gold standard imaging technique for identifying herniated discs, nerve compression, and other spinal abnormalities.
- CT Scan: To visualize the bone structure and help identify spinal issues.
- X-rays: To check for spinal alignment and rule out other potential causes of pain.
- Electromyography (EMG): To measure the electrical activity of muscles and help differentiate between nerve root compression and peripheral nerve issues.
Classification
Cervical microdiscectomy can be classified by the surgical approach:
- Anterior Cervical Discectomy (ACD): Performed from the front of the neck, usually through a small incision.
- Posterior Cervical Discectomy (PCD): Performed from the back of the neck, typically with an operating microscope for magnification.
- Endoscopic Discectomy: A minimally invasive technique using an endoscope and specialized instruments for a smaller incision and faster recovery.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions that may mimic cervical radiculopathy include:
- Thoracic Outlet Syndrome: Compression of nerves or blood vessels between the collarbone and the first rib, causing arm and hand pain.
- Rotator Cuff Injuries: Shoulder problems that can radiate pain down the arm, potentially mimicking cervical nerve compression.
- Carpal Tunnel Syndrome: Compression of the median nerve in the wrist causing similar symptoms in the hands.
- Peripheral Neuropathy: Nerve damage outside the spinal cord that may present with similar symptoms.
Treatment Options
Non-Surgical Care
- Physical Therapy: Exercises to strengthen the neck and upper back muscles, which can help alleviate pressure on the nerves.
- Medications: Pain relievers, muscle relaxants, and anti-inflammatory medications.
- Cervical Collar: Sometimes recommended to limit neck movement and reduce nerve compression.
- Epidural Steroid Injections: To reduce inflammation around the nerve roots.
- Nerve Blocks: To provide temporary relief from radicular pain.
Surgical Care
- Cervical Microdiscectomy: The removal of herniated disc material using an operating microscope to relieve pressure on the nerve root.
- Endoscopic Discectomy: A minimally invasive version of microdiscectomy using an endoscope.
- Anterior Cervical Discectomy and Fusion (ACDF): In cases where stabilization is needed, the disc is removed and the adjacent vertebrae are fused.
- Posterior Cervical Discectomy: Performed from the back of the neck, typically using an operating microscope for better visualization.
Recovery and What to Expect After Treatment
After cervical microdiscectomy, most patients:
- Pain Management: Initial pain is controlled with medications, and many patients report significant pain relief from nerve compression.
- Physical Therapy: Gentle exercises to improve mobility and strength.
- Hospital Stay: Most patients are discharged the same day or within 24 hours.
- Activity Restrictions: Avoid heavy lifting and strenuous activity during the initial recovery phase.
- Follow-up Care: Routine follow-up visits to monitor recovery and ensure the nerve root remains decompressed.
Possible Risks or Side Effects (Complications)
While cervical microdiscectomy is generally safe, complications may include:
- Injury to the Nerve Root: Rare, but possible during surgery.
- Dural Tear: Accidental puncture of the dura mater, requiring repair.
- Infection: At the surgical site.
- Recurrence of Disc Herniation: Some patients may experience a re-herniation of the disc at the same level.
- Cervical Instability: In some cases, instability may occur, requiring additional procedures like fusion.
Long-Term Outlook (Prognosis)
The prognosis for cervical microdiscectomy is generally excellent, with most patients experiencing significant pain relief and improvement in mobility. The minimally invasive nature of the surgery leads to faster recovery times and lower complication rates compared to traditional open discectomy. However, a small percentage of patients may experience recurrent symptoms or require additional surgeries in the future.
Out-of-Pocket Cost
Medicare
CPT Code 63020 – Cervical Microdiscectomy: $271.49
Under Medicare, 80% of the approved cost for this procedure is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved cervical microdiscectomy. These supplemental plans coordinate directly with Medicare to ensure full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it functions as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on the policy and network status.
Workers’ Compensation
If your cervical spine condition requiring microdiscectomy surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your cervical spine injury resulting in microdiscectomy surgery is caused by a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses, including the procedure. The only possible out-of-pocket cost may be a small deductible depending on your specific policy terms.
Example
Carlos, a 58-year-old patient with a herniated cervical disc, underwent cervical microdiscectomy (CPT 63020) to relieve nerve compression and alleviate pain. His estimated Medicare out-of-pocket cost was $271.49. Since Carlos had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. How long is the recovery after cervical microdiscectomy?
A. Most patients experience significant pain relief and can return to light activities within 1-2 weeks. Full recovery may take 4-6 weeks, depending on the individual.
Q. Will I need a fusion after cervical microdiscectomy?
A. Fusion is generally not necessary after microdiscectomy unless there is significant spinal instability or a multi-level disc herniation.
Q. Is there a risk of recurrence of the herniation?
A. While rare, disc herniation can recur after surgery, particularly if proper post-operative care is not followed.
Summary and Takeaway
Cervical microdiscectomy is a highly effective and minimally invasive procedure for relieving radicular pain caused by cervical disc herniation. The procedure offers quick recovery times and significant pain relief. While risks exist, such as nerve injury or recurrence of herniation, the success rates are high, and many patients return to normal activities soon after surgery.
Clinical Insight & Recent Findings
A recent study investigated the impact of rehabilitation on patients following anterior cervical discectomy and fusion (ACDF) surgery, focusing on pain management and recovery.
The study found that patients who underwent physical therapy and exercise after surgery (Group B) showed significant improvement in pain levels and disability index scores (VAS and ODI) six months postoperatively. In contrast, those who did not follow the rehabilitation program (Group A) experienced a slower recovery, with persistent pain.
However, no significant difference was observed in the cervical lordosis angle between the two groups, suggesting that while rehabilitation improved symptoms, it did not affect spinal alignment. The study supports the importance of early rehabilitation in enhancing post-surgical recovery and pain management. (“Study on rehabilitation after ACDF surgery – see PubMed“).
Who Performs This Treatment? (Specialists and Team Involved)
Cervical microdiscectomy is performed by:
- Spine Surgeons: Orthopedic or neurosurgeons specializing in spinal disorders.
- Anesthesiologists: For anesthesia management during surgery.
- Physical Therapists: To assist in rehabilitation after surgery.
When to See a Specialist?
If you experience persistent or worsening neck pain, arm pain, numbness, or weakness, and conservative treatments have failed, consult a spine specialist to discuss the possibility of surgery.
When to Go to the Emergency Room?
Seek emergency care if you experience:
- Sudden loss of bladder or bowel control.
- Severe, unmanageable pain.
- Sudden weakness or numbness in the arms or legs.
What Recovery Really Looks Like?
Recovery from cervical microdiscectomy is typically faster than traditional surgery, with many patients resuming light activities within a few weeks. Full recovery may take a few months, depending on the individual.
What Happens If You Ignore It?
Ignoring symptoms of cervical radiculopathy can lead to permanent nerve damage, muscle weakness, and loss of function. Early surgical intervention can prevent these outcomes and significantly improve quality of life.
How to Prevent It?
Maintaining good posture, strengthening neck and upper back muscles, and avoiding repetitive strain on the cervical spine can help prevent disc herniation and the need for surgery.
Nutrition and Bone or Joint Health
A diet rich in calcium and vitamin D can support bone health, and proper hydration is essential for maintaining the discs’ integrity in the spine.
Activity and Lifestyle Modifications
After surgery, patients should avoid heavy lifting and high-impact activities for several weeks. Low-impact exercises like walking or swimming can help maintain flexibility and strength during recovery.
Do you have more questions?
What is cervical microdiscectomy?
Cervical microdiscectomy is a surgical procedure to decompress spinal nerve roots in the neck by removing the herniated part of the intervertebral disc.
What is cervical radiculopathy?
Cervical radiculopathy is a condition caused by compression of cervical nerve roots, often due to a herniated disc, leading to pain, numbness, or weakness in the neck, shoulders, arms, and hands.
What is the role of MRI in diagnosing cervical radiculopathy?
MRI helps visualize the herniated cervical disc and assess the extent of nerve root compression.
What are the differences between anterior and posterior cervical discectomy?
Anterior cervical discectomy involves an incision in the front of the neck and allows for better visibility and access to the disc. Posterior cervical discectomy involves an incision in the back of the neck and provides access mainly to the side of the spinal cord.
What non-surgical treatments are available for cervical radiculopathy?
Non-surgical treatments include activity modification, pain medications, physical therapy, heat/cold therapy, epidural injections, and nerve root block injections.
What are the disadvantages of ACDF?
ACDF decreases neck motion and requires the placement of metallic hardware in the cervical spine.
What is the difference between anterior cervical discectomy with and without fusion?
Anterior cervical discectomy with fusion involves fusing the vertebrae after disc removal, while without fusion involves only removing the herniated disc and bone spurs without fusing the vertebrae.
What are the potential complications of cervical microdiscectomy?
Complications can include inadequate removal of herniation, excessive bleeding, nerve root damage, dural tear, CSF leakage, and injury to the esophagus, trachea, blood vessels, or nerves.
What imaging studies are used to diagnose cervical radiculopathy?
Imaging studies include X-rays, CT scans, and MRIs, with MRIs being the most detailed for visualizing soft tissues and nerve compression.
What is the role of electromyography (EMG) and nerve conduction tests in diagnosing cervical radiculopathy?
EMG and nerve conduction tests help differentiate cervical radiculopathy from peripheral neuropathy by assessing nerve function and muscle activity.
What is the role of the intervertebral disc in the cervical spine?
The intervertebral disc acts as a cushion between vertebrae, allowing for flexibility and absorbing shock during movement.
Can cervical microdiscectomy be performed using minimally invasive techniques?
Yes, cervical microdiscectomy can be performed using minimally invasive techniques with the help of an endoscope, resulting in smaller incisions and potentially quicker recovery.

