Neck pain is a common condition that can result from poor posture, muscle strain, degenerative changes, or injury. Most people experience neck discomfort at some point, often due to mechanical or postural causes. In most cases, it can be effectively managed with short-term rest, physical therapy, and simple home exercises.
However, if neck pain is accompanied by numbness, tingling, weakness, or radiating pain into the arms, it may indicate nerve compression or disc disease that requires medical attention.
How Common It Is and Who Gets It? (Epidemiology)
Neck pain affects nearly 20–30% of adults annually and is more common in women and older adults.
People who work long hours at desks or use computers frequently are especially at risk. Poor posture, stress, and repetitive movements can contribute significantly.
Most of these patients of disc disease are treated with medications and some rest. If there is no relief of symptoms with these conservative means, then they may need to undergo advance imaging to confirm the diagnosis and help in deciding further treatment.
Why It Happens – Causes (Etiology and Pathophysiology)
Neck pain can arise from several structures, including muscles, ligaments, joints, or intervertebral discs.
Common causes include:
- Muscle or ligament strain: Often due to poor posture, sudden movement, or overuse.
- Degenerative disc disease: Aging causes discs to lose flexibility, leading to stiffness or nerve irritation.
- Herniated cervical disc: The soft inner portion of the disc presses on nearby nerves, causing pain or numbness down the arm (cervical radiculopathy).
- Arthritis: Wear-and-tear arthritis (cervical spondylosis) can cause bone spurs that compress nerves.
- Whiplash injuries: Sudden acceleration or deceleration of the neck, as seen in car accidents, can strain muscles and ligaments.
- Postural imbalance: Extended use of smartphones or computers (“tech neck”) strains the cervical spine.
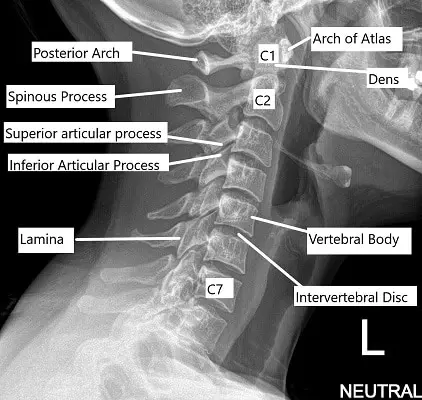
How the Body Part Normally Works? (Relevant Anatomy)
The cervical spine consists of seven vertebrae (C1–C7) supporting the head and allowing motion in all directions. These vertebrae are cushioned by intervertebral discs that act as shock absorbers. Muscles, tendons, and ligaments stabilize the spine and facilitate movement.
Pain occurs when these structures are strained, inflamed, or compressed.
What You Might Feel – Symptoms (Clinical Presentation)
Common symptoms of neck pain include:
- Aching or stiffness in the neck and shoulders.
- Reduced range of motion, making it difficult to turn or tilt the head.
- Pain radiating to the arms or hands (cervical radiculopathy).
- Numbness, tingling, or weakness in the upper extremities.
- Headaches, often originating from the neck (cervicogenic headaches).
- Muscle spasms or tightness in the neck and shoulders.
In most cases, pain improves with rest and physical therapy, but persistent symptoms may indicate a structural problem such as a herniated disc or arthritis.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis starts with a detailed medical history and physical examination. The physician will assess posture, muscle strength, reflexes, and nerve function.
Imaging tests may include:
- X-rays: Reveal bone alignment and degenerative changes.
- MRI: Provides detailed views of discs, nerves, and soft tissues.
- CT scans: Useful for bone or joint abnormalities.
- Nerve conduction studies (EMG/NCS): Evaluate nerve compression or damage.
Classification
Neck pain can be classified by duration and cause:
- Acute: Lasts less than 6 weeks, often due to muscle strain or poor posture.
- Subacute: Lasts 6–12 weeks.
- Chronic: Persists for more than 3 months, usually due to degenerative conditions or arthritis.
It can also be divided into mechanical neck pain (musculoskeletal) and neuropathic pain (nerve-related).
Other Problems That Can Feel Similar (Differential Diagnosis)
- Shoulder impingement or rotator cuff injuries
- Thoracic outlet syndrome
- Cervical spine fractures
- Myofascial pain syndrome
- Meningitis or other infections
- Rheumatoid arthritis or autoimmune disorders
Disclaimer – The above video content is external and shows the opinion of the involved vendor.
Rarely, the patient may need to undergo neck and spine surgery which can either be done from the front of the neck or the back depending on the condition as well as patient characteristics. Recovery from neck surgery is usually smooth and carries a good prognosis. Most patients can return to their normal daily activities within 2 to 3 months.
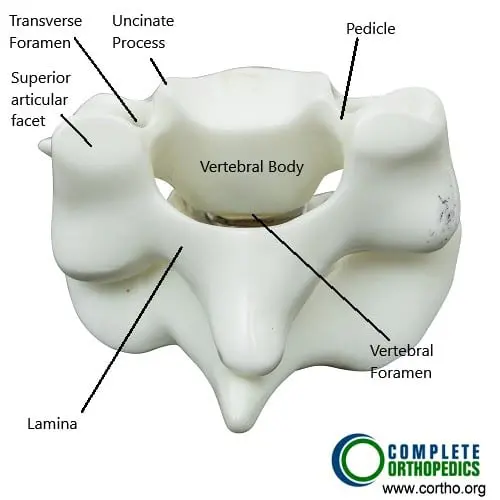
The image above shows the cervical spine vertebrae from the back. Spinal nerves or the spinal cord may be compressed due to the disease of various structures surrounding the spinal nerve or the spinal cord.
The patient should look for red flags and contact the physician if any of the red flags are present. The patients who are not relieved with conservative treatment may need to undergo advanced imaging to find out the cause of pain and plan treatment.
RED FLAGS
Neck pain can sometimes be a presentation of some grave underlying disorder. The patients who have back or neck pain with or without radiculopathy, (radiating pain, tingling, numbness) who have any of these following conditions should seek medical attention as soon as possible.
- Cancer, neoplasia or malignancy.
- Unexplained weight loss of more than 10 pounds in the last 6 months.
- Immunocompromised comorbidities like on chemo or radiotherapy or having disease like HIV or AIDs or being on prolonged corticosteroid therapy.
- IV drug users.
- Urinary tract infection.
- Fever of more than 100 degrees centigrade.
- Significant trauma from a fall or accident.
- Bowel or bladder involvement in the form of incontinence or retention.
- Weakness in the major joint of arm or leg.
Treatment Options
Non-Surgical Care
Most patients improve with conservative treatment.
- Medications:
- NSAIDs (ibuprofen, naproxen) for inflammation and pain relief.
- Muscle relaxants for spasm-related pain.
- Short-term corticosteroids for severe inflammation.
- Physical therapy:
- Stretching and strengthening exercises to restore mobility.
- Posture correction and ergonomic training.
- Heat and cold therapy: Helps relieve muscle stiffness and swelling.
- Lifestyle modification: Maintaining proper posture, avoiding heavy lifting, and regular exercise.
- Alternative treatments: Massage, acupuncture, and chiropractic care can help relieve muscle tension.
Surgical Care
Surgery is considered only when conservative treatment fails or there is nerve compression causing weakness or numbness.
Common surgical options include:
- Discectomy: Removal of a herniated disc pressing on a nerve.
- Laminectomy: Removal of part of the vertebra to relieve spinal cord compression.
- Cervical fusion or arthroplasty (disc replacement): Stabilizes the spine or replaces the damaged disc to restore function.
Recovery and What to Expect After Treatment
- Conservative recovery: Most patients recover within 4–6 weeks with exercise and posture correction.
- After surgery: Recovery typically takes 2–3 months, with gradual improvement in pain and mobility.
Physical therapy and strengthening exercises are essential for maintaining long-term results.
Possible Risks or Side Effects (Complications)
- Persistent or recurring pain
- Nerve irritation or numbness
- Stiffness or limited range of motion
- Infection (after surgery)
- Rarely, spinal cord injury in severe degenerative cases
Long-Term Outlook (Prognosis)
The prognosis for neck pain is excellent in most cases. Early diagnosis, physical therapy, and ergonomic modifications help prevent chronic pain. Only a small percentage of patients require surgery, and outcomes are generally very good.
Out-of-Pocket Costs
Medicare
CPT Code 63020 – Discectomy (Cervical/Thoracic): $271.49
CPT Code 63045 – Laminectomy (Posterior Decompression): $319.26
CPT Code 22551 – Anterior Cervical Discectomy and Fusion (ACDF): $417.50
CPT Code 22856 – Cervical Disc Replacement (Arthroplasty): $396.11
Under Medicare, 80% of the approved amount for these cervical spine procedures is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—usually pay this 20%, ensuring that most patients have little or no out-of-pocket costs for Medicare-approved surgeries. These supplemental policies are designed to coordinate with Medicare, covering complex cervical procedures such as discectomy, decompression, fusion, or disc replacement.
If you have secondary insurance—such as Employer-Based Plans, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer after Medicare. Once your deductible is satisfied, the secondary plan may cover remaining coinsurance or small residual charges. Most secondary policies carry a modest deductible, typically between $100 and $300, depending on your plan and provider network.
Workers’ Compensation
If your cervical spine condition or injury requiring discectomy, decompression, or fusion resulted from a work-related incident, Workers’ Compensation will pay all related medical and surgical costs, including hospitalization and rehabilitation. You will not have any out-of-pocket expenses under an approved Workers’ Compensation claim.
No-Fault Insurance
If your neck injury or cervical disc disease was caused or aggravated by a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses, including decompression, fusion, or disc replacement. The only possible out-of-pocket expense would be a small deductible depending on your policy’s terms.
Example
Jennifer, a 61-year-old patient with cervical disc degeneration and nerve compression, underwent anterior cervical discectomy and fusion (CPT 22551) with a disc replacement (CPT 22856). Her Medicare out-of-pocket costs were $417.50 and $396.11. Because she had supplemental insurance through AARP Medigap, the 20% not paid by Medicare was fully covered, leaving her with no out-of-pocket expense for her procedures.
Frequently Asked Questions (FAQ)
Q. What causes most cases of neck pain?
A. The majority of neck pain cases are caused by poor posture, muscle strain, or degenerative changes in the cervical spine.
Q. When should I see a doctor for neck pain?
A. If pain radiates to your arms, causes weakness or numbness, or persists for more than a few weeks, consult a spine specialist.
Q. Can neck pain be prevented?
A. Yes. Regular stretching, maintaining good posture, and using ergonomic work setups can help prevent most cases.
Q. Is surgery always required for neck pain?
A. No. Over 90% of cases improve with rest, medications, and physical therapy. Surgery is reserved for patients with nerve compression or severe spinal instability.
Summary and Takeaway
Neck pain is a common condition that usually improves with conservative treatment such as exercise, posture correction, and medication. Persistent pain with radiating symptoms may require imaging and, in rare cases, surgical intervention. Early treatment, regular exercise, and proper ergonomics are key to long-term recovery and prevention of recurrence.
Clinical Insight & Recent Findings
A recent case report described a 68-year-old woman presenting with chronic neck pain and swelling, later diagnosed as tuberculosis lymphadenitis (scrofula). She had immigrated from Haiti and reported two years of bilateral neck swelling with intermittent purulent drainage unresponsive to antibiotics, along with night sweats and weight loss.
Examination revealed nontender, hyperpigmented nodules with crusting along the cervical chain, while CT imaging showed a 3.4 cm necrotic lymph node with bilateral cervical, mediastinal, and axillary lymphadenopathy. A positive QuantiFERON-TB Gold test and lymph node biopsy confirmed the diagnosis. Treatment with rifampin, isoniazid, pyrazinamide, and ethambutol for two months, followed by rifampin and isoniazid for four months, led to full recovery.
The authors noted that paradoxical lymph node enlargement may occur during therapy in about 20% of cases but does not indicate treatment failure. This case highlights the need to consider extrapulmonary tuberculosis in patients with chronic cervical lymphadenopathy, especially those from endemic regions. (Study of tuberculosis lymphadenitis presenting as chronic neck pain – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Neck pain is managed by orthopedic spine surgeons, neurosurgeons, pain specialists, and physical therapists working as a coordinated team.
When to See a Specialist?
You should see a specialist if you experience:
- Persistent pain lasting more than 2–3 weeks.
- Radiating pain, numbness, or tingling in the arms.
- Weakness in the shoulders or hands.
- Difficulty moving the neck or turning your head.
When to Go to the Emergency Room?
Seek emergency care if you develop:
- Sudden loss of coordination or strength in arms or legs.
- Loss of bladder or bowel control.
- Fever, unexplained weight loss, or history of cancer with new neck pain.
- Severe trauma to the neck.
What Recovery Really Looks Like?
With conservative care, most patients see steady improvement within weeks. After surgery, full recovery may take 2–3 months, aided by physical therapy. Continued neck exercises and posture correction prevent recurrence.
What Happens If You Ignore It?
Untreated neck pain can progress to chronic stiffness, nerve compression, or permanent weakness. Early intervention helps maintain mobility and prevents complications.
How to Prevent It?
- Practice proper posture at all times.
- Adjust workstation ergonomics to keep screens at eye level.
- Take frequent breaks from desk or phone use.
- Maintain strong neck and shoulder muscles through exercise.
- Manage stress to avoid tension-related neck strain.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and omega-3 fatty acids supports bone and joint health. Hydration and proper nutrition promote spinal disc elasticity and muscle recovery.
Activity and Lifestyle Modifications
Incorporate low-impact exercises like swimming, yoga, or stretching into your routine. Avoid prolonged sitting or slouching. Use supportive pillows while sleeping and avoid cradling phones between the ear and shoulder.
Do you have more questions?
What is the most common cause of neck pain?
The most common cause of neck pain is nonspecific neck pain, which often arises from muscle strain or poor posture. It is typically not related to any specific injury or disease.
How can I tell if my neck pain is serious?
If your neck pain is accompanied by symptoms like numbness, tingling, weakness in the arms or hands, severe headaches, or if it follows a traumatic injury, it could indicate a more serious condition, and you should seek medical attention immediately.
When should I see a doctor for neck pain?
You should see a doctor if your neck pain persists for more than a few weeks, is severe, or if you have symptoms like arm or hand weakness, numbness, or if the pain follows an injury such as a fall or car accident.
Can poor posture really cause neck pain?
Yes, poor posture, particularly when sitting or working at a desk for long periods, is a major cause of neck pain. It puts additional strain on the neck muscles and cervical spine, leading to discomfort.
What are the risks of untreated neck pain?
Untreated neck pain can lead to chronic pain, reduced mobility, decreased quality of life, and in some cases, it can result in the development of other conditions like chronic headaches or shoulder problems.
Is surgery ever necessary for neck pain?
Surgery is typically considered only when there is a clear structural issue, such as a herniated disc causing significant nerve compression, and when conservative treatments have not provided relief.
Can neck pain cause headaches?
Yes, neck pain can cause cervicogenic headaches, which originate in the neck and radiate to the head. This is often due to tension in the neck muscles or issues with the cervical spine.
How can I prevent neck pain from recurring?
Preventing neck pain involves maintaining good posture, taking regular breaks from sitting, exercising to strengthen neck and back muscles, and managing stress effectively.
What is the role of physical therapy in treating neck pain?
Physical therapy plays a crucial role in treating neck pain by improving flexibility, strength, and posture. It also helps reduce pain and prevent recurrence through targeted exercises and manual therapy techniques.
Can neck pain be a sign of a more serious condition?
Yes, while most neck pain is not serious, it can be a sign of conditions like cervical radiculopathy, spinal stenosis, or even certain infections or cancers. It’s important to evaluate symptoms like severe pain, neurological deficits, or pain that doesn’t improve.
What lifestyle changes can help with neck pain?
Lifestyle changes that can help include improving posture, incorporating regular exercise, ensuring proper ergonomics at work, managing stress, and avoiding activities that strain the neck.
How does aging affect neck pain?
Aging can lead to degenerative changes in the cervical spine, such as disc degeneration and osteoarthritis, which can contribute to chronic neck pain. Regular exercise and maintaining a healthy lifestyle can help mitigate these effects.
What is the difference between neck pain and a pinched nerve?
Neck pain refers to general discomfort in the neck area, while a pinched nerve (cervical radiculopathy) involves nerve compression that can cause pain, numbness, or weakness radiating from the neck into the arms or hands.
Can ergonomic adjustments at work help with neck pain?
Yes, adjusting your workstation to ensure proper posture, such as having your monitor at eye level and using an ergonomic chair, can significantly reduce the risk of developing neck pain.
Are there any alternative therapies for neck pain?
Alternative therapies like acupuncture, chiropractic care, and massage can provide relief for some people. However, these should be used in conjunction with traditional treatments and under the guidance of a healthcare provider.

