Total hip replacement (THR) is one of the most successful procedures in orthopedic surgery, providing long-term pain relief and improved mobility for patients with hip arthritis or joint degeneration. However, some patients experience persistent or new hip pain after surgery. This discomfort can result from surgical factors such as implant loosening or soft tissue damage, or from unrelated conditions like nerve irritation or referred pain from the spine. Understanding the potential causes of post-operative hip pain is critical to ensure timely diagnosis and appropriate management.
Functional Anatomy
The hip is a ball-and-socket joint formed by the femoral head (ball) and the acetabulum (socket) of the pelvis. Both surfaces are covered by smooth cartilage, which allows pain-free motion. During total hip replacement, damaged cartilage and bone are replaced with prosthetic components: a metal or ceramic ball attached to a metal stem fitted into the femur, and a metal cup lined with plastic, ceramic, or metal in the acetabulum. These components restore joint function, reduce friction, and relieve arthritic pain.
Biomechanics or Physiology
A successful hip replacement replicates the natural biomechanics of the hip, allowing smooth movement, stability, and weight-bearing. The prosthesis must maintain proper alignment and fit securely within the bone to distribute forces evenly across the joint. Pain after hip replacement may arise when this mechanical balance is disrupted—by implant loosening, uneven loading, or impingement. Muscle and tendon injuries, nerve irritation, or changes in bone density around the implant can also contribute to discomfort.
Common Variants and Anomalies
Postoperative hip pain can be categorized into two main groups:
- Pain with abnormal imaging (e.g., implant loosening, bone loss, or infection).
- Pain with normal imaging (e.g., soft tissue irritation, nerve injury, or referred pain).
Specific variants include aseptic loosening, septic loosening, heterotopic ossification, stress shielding, and iliopsoas tendon impingement. Each condition presents differently, requiring careful evaluation to identify the cause.
Clinical Relevance
Pain after hip replacement is not always due to the prosthesis. It can be caused by issues ranging from infection, implant wear, and loosening to soft tissue injuries and spinal pathologies. Persistent hip pain may also indicate complications such as osteolysis (bone loss) or bursitis. Early recognition and management are essential to prevent progression and to maintain function. Most patients, however, experience lasting relief from hip arthritis, and only a small percentage develop chronic postoperative pain.
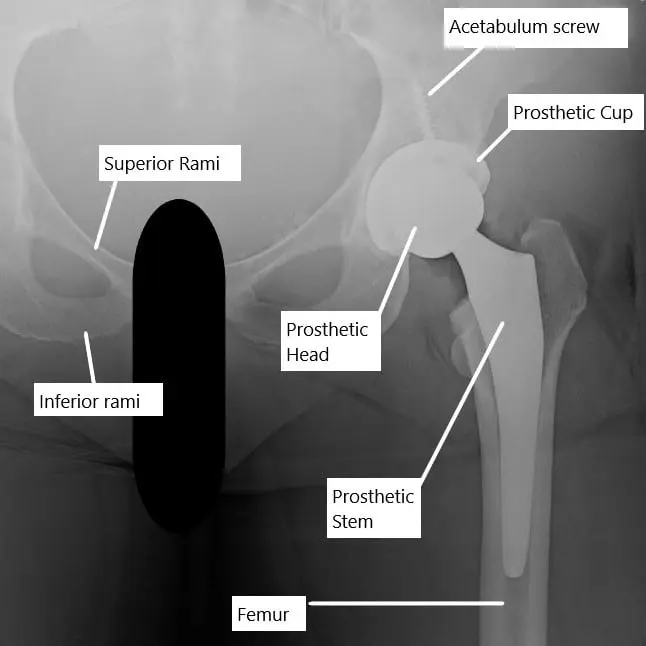
X-ray showing a total hip replacement.
Imaging Overview
Evaluation of hip pain after replacement begins with X-rays to assess implant position, loosening, or bone resorption. CT scans may be used to detect subtle bone loss or heterotopic ossification, while MRI can identify soft tissue injuries, bursitis, or tendon inflammation. Blood tests (e.g., ESR, CRP) and joint aspiration help rule out infection. Imaging findings guide treatment decisions, such as revision surgery for implant failure or conservative therapy for soft tissue inflammation.
Hip pain with abnormal X-ray studies
- Loosening of the implant without any sign of infection is known as aseptic loosening. The high grade polyethylene cup of the socket may release microscopic debris following motion. The micromotion of the implant also leads to debris accumulation.Special cells in the blood known as macrophages, try to clear the debris but in turn lead the body to attack the debris material with various enzymes and proteins.This in turn results in inflammation and loss of bone around the implant. The loss of bone surrounding the implant may lead to loosening of the implant.The loosening is visible on an X-Ray as a clear space around the implant. The implant may further sink in the femoral canal. Patients typically complain of pain after a relative painless period after the surgery.There are no signs of infection and the pain is worse on movement and weight bearing. At times, patients may complain of rest pain as well.
- Septic loosening is the loosening of the implant secondary to the infection. Infected hip replacement may lead to erosion of the bone around the implant.The erosion and loss of bone is due to various chemicals released by the infecting agent (usually a bacteria) and as a result of the body’s immune system trying to fight the infection. There may be formation of tracts which may open in the skin, leading to discharge of pus.Patients may have a rise of temperature, swelling and redness of the hip area. Some patients may have a low grade fever. The patient complains of pain which is characteristically worse at night or rest. The pain may occur immediately following the surgery or after weeks, months or years after the surgery.
- Abnormal formation of bone in the tissues surrounding the implant such as muscles is known as heterotrophic ossification. Heterotrophic ossification is visible as bone tissue in the muscles surrounding the hip joint. Patients complain of pain after a relative pain free period after the surgery. The pain is worse with activity and gets better with rest.
- Thigh pain may occur as a result of stress shielding of the femoral stem. The stiff femoral stem may impinge upon the weak bone especially further down the thigh bone.The stress of the femoral stem may lead to thickening of the bone down the thigh bone. Stress shielding occurs due to mismatch of the forces acting at the end of the femoral stem. Patients usually complain of thigh pain rather than hip or groin pain.
- Osteolysis is the loss of bone surrounding the implant but without any loosening. The loss of bone around the implant may lead to pain in the hip region.
- Wrong sized implant and improper positioning of the implant may lead to instability and reduced motion about the hip. The patients often complain of hip pain which may be present in the groin, buttocks or the side of the hip.

Intraoperative image of total hip replacement.
Hip pain with normal X-ray studies
- Iliopsoas tendinitis occurs due to the impingement of the iliopsoas tendon as it crosses the hip joint in the front. Patients complain of hip pain in the groin area and may walk with a limp secondary to pain.The pain characteristically appears after initiation of walking. The iliopsoas muscle helps in the bending of the hip. The pain therefore worsens on bending (flexion) of the hip.The impingement may occur as a result of malposition of the prosthetic acetabular cup (socket). The impingement may also occur as a result of retained cement particles during the surgery. A numbing injection in the tendon may be used for diagnosing iliopsoas tendinitis.
- Reactive synovitis may cause hip pain after hip replacement. Synovitis may occur as a result of osteolysis or may occur in the absence of osteolysis. The reactive synovitis may be diagnosed with the help of an MRI.
- Damage to the muscle groups during the surgery may lead to postoperative dysfunction and hip pain. The abductor muscles may be damaged during the surgery and may lead to limping and associated pain.
- Bursitis of the trochanteric bursae may lead to characteric pain over the side of the hip. The pain may be associated with pins and needles sensation. The bursae are small sacs containing fluid that help the smooth passing of the tendon and muscles over bony prominences.
- Improper position and uncovered prosthesis during the surgery may lead to impingement of the prosthetic implant. The pain is worse with activity and may get better with rest.
- Damage to the nerves surrounding the hip joint such as the sciatic nerve, superior gluteal nerve, femoral and obturator nerve may lead to pain following the surgery.The risk of damage to a particular nerve depends upon the approach used during the surgery and the technique of the surgery. The symptoms of nerve damage may not be immediate in patients in whom a blood collection in the area surrounding the nerve causes damage.
- Lumbar spine pathologies such as lumbar canal stenosis, prolapsed intervertebral disc and facet joint disease, etc may cause radiating pain to the hip region. Through evaluation and history may help to differentiate the radiating spine pain from hip pain.
- Rarely, pain may be referred to the hip region from a disease process in the abdomen or due to inguinal hernia.
Associated Conditions
Several conditions may lead to pain after total hip replacement:
- Aseptic Loosening – Gradual bone loss and implant micromotion causing pain during movement and weight-bearing.
- Septic Loosening – Infection around the implant resulting in bone erosion, pus formation, and night pain.
- Heterotopic Ossification – Abnormal bone growth in soft tissues around the hip, limiting motion and causing discomfort.
- Stress Shielding – Bone thickening and thigh pain due to mismatch between implant stiffness and bone flexibility.
- Osteolysis – Bone loss from inflammatory reactions to debris from the prosthetic material.
- Iliopsoas Tendinitis – Groin pain from tendon impingement on the implant or residual cement.
- Trochanteric Bursitis – Pain over the lateral hip due to inflammation of the trochanteric bursa.
- Nerve Injury – Damage to nerves such as the sciatic or femoral nerve causing radiating or burning pain.
- Referred Pain – Pain from the lumbar spine, hernia, or abdomen perceived in the hip region.
Surgical or Diagnostic Applications
Diagnostic evaluation includes:
- Clinical examination for tenderness, swelling, and range of motion.
- X-rays to assess loosening, subsidence, or implant malposition.
- CT or MRI for detecting bone or soft tissue changes.
- Joint aspiration and cultures for infection confirmation.
Treatment depends on the diagnosis: - Non-surgical management includes anti-inflammatory medications, physiotherapy, or injections for bursitis and tendinitis.
- Surgical management may involve revision surgery for implant loosening, irrigation and debridement for infection, or tendon release for impingement.
Prevention and Maintenance
Preventing postoperative pain and complications requires:
- Careful implant selection and positioning during surgery.
- Adherence to postoperative rehabilitation to maintain muscle strength and joint mobility.
- Infection prevention protocols, including sterile technique and antibiotic prophylaxis.
- Weight management and activity modification, avoiding high-impact sports that can accelerate implant wear.
- Routine follow-up imaging to detect early signs of loosening or bone loss.
Research Spotlight
Following a total hip replacement, patients may experience pain or discomfort despite the procedure’s general success. The causes of this discomfort can range from issues directly related to the surgery, such as implant loosening or muscle damage, to factors unrelated to the surgery itself.
Understanding the relationship between tendon degeneration and muscle strength, particularly in key areas such as the gluteus medius, is critical for rehabilitation planning. A recent study found a moderate correlation between degeneration in the gluteus medius tendon and muscle strength both before and after surgery.
This research suggests that rehabilitation should focus on strengthening key muscles, including the gluteus medius, hamstrings, and quadriceps, to minimize discomfort and improve functional recovery post-surgery. (“Study on gluteus medius tendon degeneration and its impact on hip replacement recovery – see PubMed.“)
Summary and Key Takeaways
- Pain after hip replacement can arise from surgical, mechanical, infectious, or unrelated causes.
- Aseptic loosening, infection, and tendon irritation are common causes of postoperative discomfort.
- Imaging and laboratory studies are essential for accurate diagnosis and management.
- Conservative treatments (physical therapy, anti-inflammatory medications) are effective for mild cases, while revision surgery may be needed for implant-related complications.
- Strengthening key muscles and maintaining proper rehabilitation routines are vital for long-term pain relief and functional success.
References / Citations (Optional)
American Academy of Orthopaedic Surgeons. “Total Hip Replacement.”
Study on gluteus medius tendon degeneration and its impact on hip replacement recovery – see PubMed.
¿Tienes más preguntas?
Are there specific exercises or rehabilitation techniques that can target and alleviate pain after hip replacement surgery?
Yes, physical therapists can prescribe a variety of exercises and rehabilitation techniques tailored to each patient’s needs and goals. These may include gentle stretching, strengthening exercises, balance training, gait training, and functional activities to help reduce pain and improve hip function.
Can certain lifestyle modifications help in managing pain after hip replacement surgery?
Yes, adopting certain lifestyle modifications such as maintaining a healthy weight, avoiding activities that put excessive stress on the hip joint, using assistive devices as needed, practicing good posture, and following proper body mechanics can help in managing pain and promoting long-term joint health after hip replacement surgery.
How important is it to adhere to post-operative instructions and precautions to minimize pain and complications?
Adhering to post-operative instructions and precautions provided by the surgeon and healthcare team is crucial for minimizing pain, preventing complications, and promoting successful outcomes after hip replacement surgery. These instructions often include activity restrictions, medication management, wound care, and follow-up appointments.
Is it normal to experience psychological distress or emotional reactions such as anxiety or depression due to pain after hip replacement surgery?
Yes, it is not uncommon for patients to experience psychological distress or emotional reactions such as anxiety, depression, frustration, or fear due to pain or challenges during the recovery process after hip replacement surgery. Seeking support from healthcare professionals, family members, or mental health professionals can be helpful in addressing these concerns.
How can I effectively communicate my pain levels and concerns to my healthcare provider after hip replacement surgery?
Effective communication with your healthcare provider is essential for addressing pain and concerns after hip replacement surgery. Keep a pain diary, be specific about your symptoms, ask questions, express your preferences and goals for pain management, and actively participate in shared decision-making regarding treatment options.
Are there any alternative or complementary therapies that may help in managing pain after hip replacement surgery?
Yes, alternative or complementary therapies such as acupuncture, massage therapy, heat or cold therapy, relaxation techniques, guided imagery, or dietary supplements may provide additional relief from pain and support overall well-being after hip replacement surgery. However, it’s essential to discuss these options with your healthcare provider before trying them.
What are the potential long-term effects or complications of persistent pain after hip replacement surgery?
Persistent pain after hip replacement surgery may impact a patient’s quality of life, mobility, independence, and ability to perform daily activities. It may also increase the risk of developing chronic pain, functional limitations, joint stiffness, muscle weakness, or psychological issues over time. Early recognition and management of pain are crucial for minimizing long-term effects and complications.
How does the type of hip replacement surgery (e.g., anterior vs. posterior approach) impact post-operative pain and recovery?
The type of hip replacement surgery, such as anterior vs. posterior approach, can affect post-operative pain, recovery time, and outcomes. The anterior approach may result in less muscle damage and faster recovery, potentially leading to reduced post-operative pain compared to the posterior approach. However, individual factors and surgical techniques also play significant roles in determining pain levels and recovery outcomes.
How soon after hip replacement surgery can I start physical therapy to address pain and regain mobility?
Physical therapy typically begins soon after hip replacement surgery, often within the first few days or weeks, depending on the individual’s overall health status and the surgeon’s recommendations.
What role does physical therapy play in managing pain after hip replacement surgery?
Physical therapy is an essential component of rehabilitation after hip replacement surgery, helping to improve strength, flexibility, and mobility while reducing pain and promoting optimal recovery.
Are there any specific warning signs or symptoms that I should watch out for regarding pain after hip replacement surgery?
Yes, warning signs or symptoms to watch out for regarding pain after hip replacement surgery include sudden onset or worsening of pain, pain that does not improve with rest or medication, swelling, warmth, redness, or drainage from the surgical site, fever, chills, or difficulty moving the hip joint.
How can I differentiate between normal post-operative pain and pain that may signal a complication?
Normal post-operative pain typically improves gradually over time and is manageable with pain medications and other conservative measures. However, pain that is severe, worsening, or accompanied by other concerning symptoms such as fever, redness, swelling, or difficulty bearing weight may indicate a complication and requires medical attention.
Should I be concerned if I experience persistent or severe pain after hip replacement surgery?
Persistent or severe pain after hip replacement surgery may indicate underlying issues such as infection, implant loosening, dislocation, nerve damage, or other complications, and should be promptly evaluated by a healthcare provider.
How effective are non-drug therapies such as physical therapy or acupuncture in alleviating post-operative pain?
Non-drug therapies such as physical therapy, acupuncture, or transcutaneous electrical nerve stimulation (TENS) can be effective complementary approaches to pain management after hip replacement surgery, helping to improve mobility, reduce inflammation, and alleviate discomfort.
What medications are commonly prescribed to manage pain after hip replacement surgery?
Pain management medications may include nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, opioids, muscle relaxants, or nerve pain medications, depending on the individual’s needs and tolerance.
Are there specific activities or movements that may exacerbate pain after hip replacement surgery?
Yes, certain activities such as high-impact exercises, heavy lifting, or prolonged periods of standing or walking may exacerbate pain during the recovery period after hip replacement surgery.
How long does it typically take for the pain to subside after hip replacement surgery?
The duration of pain after hip replacement surgery varies among individuals, but it often improves gradually over several weeks to months as the surgical site heals and the body adjusts to the new hip joint.
What are the most common causes of pain after hip replacement surgery?
Pain after hip replacement surgery can result from various factors such as inflammation, nerve irritation, muscle strain, implant-related issues, infection, or complications related to the surgical procedure.

