If cervical spine pain intensifies, interferes with everyday activities, or is accompanied by swelling or redness, it is crucial to consult a healthcare provider. At Complete Orthopedics, our expert team focuses on effectively managing posterior cruciate ligament injury with customized approaches and surgical options. We are committed to understanding your symptoms, identifying the underlying problems, and recommending suitable treatments or surgical procedures.
Our facilities span across New York City and Long Island, with connections to six prominent hospitals, ensuring access to top-tier care for cervical spine issues. Schedule an appointment with one of our orthopedic surgeons either online or over the phone. Learn about the causes and treatments for cervical spine pain, and recognize when surgery is the best course of action.
Overview
Anterior cervical discectomy and fusion (ACDF) is one of the most commonly performed neck surgeries. The ACDF surgery is done to relieve symptoms associated with compression of the spinal cord or the spinal nerves in the cervical region. The recovery after ACDF surgery may vary from patient to patient due to different baseline health and the type of ACDF surgery performed,
The ACDF helps to relieve symptoms such as neck pain, numbness and tingling in the arms, shoulders, or hand, shooting pain in the arms, weakness of hands, or lower extremities. During the surgery, the spine surgeon accesses the cervical vertebrae from the front of the neck.
The surgeon removes the diseased intervertebral disc and any tissues that compress the neural structures. A bone graft is usually placed along with a prosthetic bone cage to maintain the disc space and help in the union.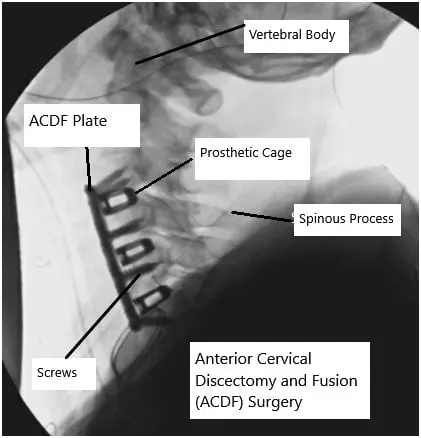
X-ray showing ACDF surgery.
Immediately after the surgery, the patient is usually managed in the recovery area and post-operative pain is managed with medication. The patient may be able to go home the same day after the surgery or the next day depending upon the extent of the surgery and patient risk. The patients are motivated to sit and walk after the surgery.
At home, the patients are usually advised to wear a neck collar to prevent sudden turning or bending movement. The neck collar may be taken off while eating or taking a shower. The post-operative pain is usually managed with opioid analgesics and the patient is slowed weaned off the analgesics in two weeks.
The patients are advised to stay active in the form of walking and moving but with precautions to not lift objects more than 5 pounds, bending, or turn quickly. The patients are also advised to report any warning signs during the initial post-op period.
Common Symptoms and Their Management
Pain: Some discomfort is normal after surgery. Pain typically improves over time and can be managed with prescribed medications.
Swelling and Soreness: Mild swelling and soreness in the neck are common and usually subside within a few weeks.
Difficulty Swallowing: This can happen due to the swelling of the throat area but generally resolves on its own.
The warning signs may be increasing numbness, tingling or weakness of the upper or lower extremities, swelling of the arms/feet, loss of bowel bladder control, pain, swelling, redness, or discharge from the incision site.
Some common symptoms patients may experience after the ACDF surgery include sore throat, hoarseness, pain, difficulty speaking and difficulty swallowing. The symptoms usually get better in the first month.
The hoarseness and difficulty speaking are attributed to the retraction of the recurrent laryngeal nerve that supplies the voice box situated on top of the windpipe. Similarly, retraction of the food pipe and the muscles around the food pipe may cause symptoms of difficulty swallowing and sore throat after ACDF.
Constipation is a common symptom immediately following ACDF surgery. Constipation may also result from the use of opioid analgesics for pain. The patients are advised to enrich their diet with fibers and increase their dietary intake of water.
The patients are advised a liquid diet during the initial recovery period to help with the symptoms of difficulty swallowing. The patients are also advised to keep phonation at a minimum and speak softly to help with difficulty speaking and hoarseness. The difficulty swallowing and speaking may require late in patients with multi-level fusion who generally have a prolonged surgery time.
First Few Weeks Post-Surgery
- Activity Level: Limited activity is crucial during the first few weeks. Patients should avoid heavy lifting, strenuous activities, and any movements that strain the neck.
- Physical Therapy: Starting physical therapy early can help in regaining strength and mobility in the neck. A tailored exercise program helps in a smoother recovery.
- Follow-Up Visits: Regular follow-up visits with the surgeon are essential to monitor the healing process.
At 4 weeks post-op, the fusion of the adjoining vertebrae has significantly progressed with a solid construct only at 3 months post-op. The fusion continues to progress into a stronger construct 1-year post-op. The patient at 4 weeks post-op are allowed more activities and after an assessment, the surgeon may recommend physical therapy.
Physical therapy is aimed at strengthening the muscles around the neck and also increasing the flexibility of the neck. Physical therapy also allows workplace assessment and the suitability of the patient to return to work. Physical therapy also helps to train patients to maintain a correct posture and balance and avoid certain motions/activities.
The patients may be allowed to participate in low-impact activities such as golf and tennis but impact sports may still be prohibited. The majority of the patients return to work at 4 weeks but some patients may return earlier depending upon the type of work and the extent of the ACDF surgery.
Along with posture precautions, smoking cessation forms an important part of the recovery. Continued smoking delays the healing of the fusion construct and may even lead to nonunion of the fusion. Smoking is also associated with increased post-op complications and continued neck pain.
The majority of the patients are quickly able to get back to the activities they enjoy following the rehabilitation after ACDF surgeries. Some patients may require special rehabilitation protocols depending upon the disease status prior to the surgery and the extent of the surgery.
Long-Term Recovery and Expectations
Gradual Return to Normal Activities
- Resuming Work: Most patients can return to light work within two to four weeks, depending on the nature of their job. Those with physically demanding jobs may need a longer recovery period.
- Physical Activity: Light exercises and walking are encouraged as they promote healing. Gradual increase in activity levels is advised.
- Driving: Patients can resume driving once they are off pain medications and can comfortably turn their head without pain.
Potential Complications
- Infection: As with any surgery, there is a risk of infection. Keeping the incision area clean and following the surgeon’s instructions can help prevent this.
- Non-Union: In some cases, the bones may not fuse as expected, a condition known as non-union. This may require additional treatment.
- Nerve Damage: Although rare, there is a risk of nerve damage, which can cause persistent pain or weakness.
Success Rates and Outcomes
High Success Rates
- According to studies, 98.2% of ACDF patients experience significant pain relief and improvement in function post-surgery. This high success rate makes ACDF a preferred option for treating cervical disc problems.
Patient Satisfaction
- Most patients report high satisfaction with the outcomes of ACDF. The procedure not only alleviates pain but also helps in improving the overall quality of life.
Long-Term Benefits
- ACDF offers long-term benefits by providing spinal stability, reducing pain, and improving neck function. With proper care and rehabilitation, patients can return to a normal, active lifestyle.
Tips for a Smooth Recovery
Follow Medical Advice: Adhering to the surgeon’s post-operative care instructions is crucial for a successful recovery.
Stay Active: Engage in light physical activities and exercises as recommended by the physical therapist.
Healthy Diet: A balanced diet rich in vitamins and minerals aids in the healing process.
Avoid Smoking: Smoking can hinder the healing process and should be avoided.
Conclusion
Recovery from ACDF surgery is a gradual process that requires patience and adherence to medical advice. With a high success rate and the potential for significant pain relief, ACDF can greatly improve the quality of life for individuals suffering from cervical spine issues. Proper post-operative care, physical therapy, and a healthy lifestyle are key to ensuring a smooth and successful recovery.
¿Tienes más preguntas?
What are the signs that my ACDF surgery is healing properly?
Signs of proper healing include a decrease in pain, reduced swelling, improved mobility, and the absence of signs of infection such as redness, warmth, or discharge at the incision site. Regular follow-ups with your surgeon will also help monitor the healing process through physical exams and possibly imaging studies.
How long will I need to wear a neck brace after ACDF surgery?
The duration for wearing a neck brace varies based on the individual case and the surgeon’s protocol. Typically, patients may need to wear it for 1-6 weeks to ensure proper spine stabilization during the initial healing phase.
When can I start physical therapy after ACDF surgery?
Physical therapy usually starts within a few weeks after surgery. Your surgeon will provide specific timing based on your recovery progress. Initial exercises will focus on gentle movements to restore neck mobility and strength.
Are there any specific exercises I should avoid during my recovery?
Yes, you should avoid high-impact activities, heavy lifting, strenuous exercises, and any movements that cause neck strain. Stick to the exercise plan provided by your physical therapist and surgeon.
Can ACDF surgery affect my ability to swallow permanently?
Difficulty swallowing is usually temporary and resolves as swelling decreases. Permanent swallowing issues are rare. If you experience persistent difficulty, contact your surgeon for an evaluation.
How should I sleep after ACDF surgery?
Sleep on your back or side with a pillow that supports the natural curve of your neck. Avoid stomach sleeping as it can strain your neck. Using a neck brace while sleeping, if recommended by your surgeon, can also provide additional support.
What should I do if I experience severe pain after surgery?
Severe pain after surgery is not typical and should be promptly reported to your surgeon. It could indicate a complication such as infection, nerve damage, or issues with the fusion.
How will I know if the bones are fusing properly?
Your surgeon will monitor the fusion process through follow-up visits and imaging tests such as X-rays or CT scans to ensure the bones are fusing properly.
Is it normal to feel numbness or tingling after ACDF surgery?
Some numbness or tingling can be normal as the nerves heal. However, if these sensations are severe or worsen, you should inform your surgeon as it could indicate nerve irritation or damage.
Can I shower or bathe after surgery?
You can typically shower a few days after surgery, but you should avoid soaking the incision in a bath until it is fully healed. Follow your surgeon’s instructions regarding wound care and hygiene.
Will I need any additional surgeries after ACDF?
Most patients do not require additional surgeries if the initial ACDF is successful. However, in cases of non-union or adjacent segment disease, further surgery might be necessary.
What are the chances of developing adjacent segment disease after ACDF?
Adjacent segment disease, where nearby spinal segments degenerate faster due to the altered mechanics, can occur in a small percentage of patients. Regular monitoring and maintaining a healthy lifestyle can help mitigate this risk.
Can I return to sports or high-intensity activities after ACDF?
You can usually return to sports or high-intensity activities several months after surgery, depending on your recovery progress and surgeon’s approval. Gradual reintroduction with proper technique and precautions is essential.
How can I prevent future cervical spine issues?
Maintaining good posture, engaging in regular exercise, avoiding smoking, and using proper body mechanics during activities can help prevent future cervical spine issues.
What dietary changes should I make to aid recovery?
A diet rich in protein, vitamins (especially vitamin D and C), calcium, and minerals supports bone healing and overall recovery. Staying hydrated and avoiding excessive caffeine and alcohol is also beneficial.
Can I drive myself to follow-up appointments?
You can drive once you are off narcotic pain medications and can move your neck comfortably. Ensure you can perform all necessary driving maneuvers without pain or restriction.
Are there any long-term limitations after ACDF surgery?
Most patients can return to normal activities without significant long-term limitations. However, it’s advisable to avoid activities that place excessive stress on the neck.
How do I manage scar care after ACDF surgery?
Keep the incision clean and dry, and follow your surgeon’s instructions on wound care. Once healed, using scar creams or silicone sheets can help minimize scarring.
Will I have a noticeable scar after ACDF surgery?
The scar is usually small and located in a natural skin crease, making it less noticeable. Over time, it will fade and become less prominent
What is the typical timeline for full recovery after ACDF?
Full recovery can take several months. Most patients feel significant improvement in symptoms within 6-8 weeks, with ongoing healing and strengthening over the next few months.
How do I know if I need to return to the surgeon before my scheduled follow-up?
If you experience severe pain, signs of infection (fever, increased redness, swelling), new or worsening neurological symptoms, or any other concerning symptoms, contact your surgeon immediately.
Can ACDF surgery fail, and what are the signs?
ACDF surgery can fail in rare cases. Signs of failure include persistent or worsening pain, instability, and lack of bone fusion. Regular follow-ups and imaging tests help detect and address any issues early.
What should I avoid doing in the initial weeks post-surgery?
Avoid heavy lifting, strenuous activities, twisting or bending your neck excessively, and any actions that cause pain or discomfort.
What are the benefits of having ACDF surgery over other types of cervical spine surgeries?
ACDF has a high success rate for relieving symptoms, provides spinal stability, and has a relatively quick recovery period compared to other more invasive spinal surgeries. It is particularly effective for addressing disc-related issues in the cervical spine.

