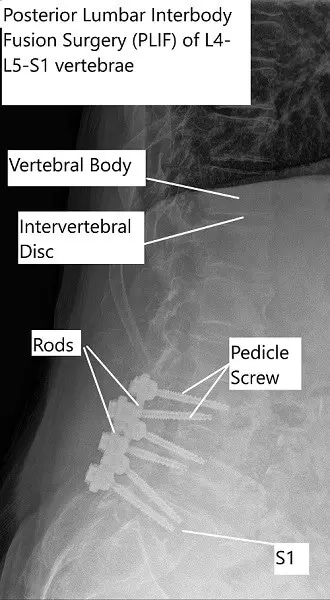
Posterior Lumbar Interbody Fusion (PLIF) is a surgical procedure performed to stabilize the spine and alleviate pain caused by various lumbar spine conditions. The surgery involves fusing one or more vertebral segments in the lower back, often using a prosthetic cage to maintain disc space and facilitate the fusion process. PLIF is typically recommended when conservative treatments for conditions such as sciatica, degenerative disc disease, or spinal instability have not provided adequate relief.
How Common It Is and Who Gets It? (Epidemiology)
Lumbar spine issues that require fusion surgery, including degenerative conditions like disc disease, spondylolisthesis, and spinal stenosis, are common, especially in individuals over 50 years of age. As the spine undergoes wear and tear over time, the risk of instability and nerve compression increases, leading to conditions that may necessitate lumbar fusion. PLIF is a frequently used technique, particularly for individuals whose pain and disability are not relieved by physical therapy or other non-surgical methods.
Why It Happens – Causes (Etiology and Pathophysiology)
Several conditions can lead to the need for posterior lumbar interbody fusion surgery:
- Degenerative Disc Disease: The natural wear and tear of spinal discs can lead to back pain and nerve compression.
- Spondylolisthesis: A condition in which one vertebra slips forward over the one below it, causing instability and pressure on the spinal nerves.
- Spinal Stenosis: Narrowing of the spinal canal that compresses the spinal cord or nerve roots.
- Traumatic Injury: Accidents or falls can cause fractures or instability in the spine.
- Congenital Instability: Some individuals are born with spinal deformities or weakened spinal structures, which may require fusion surgery to stabilize the spine.
How the Body Part Normally Works? (Relevant Anatomy)
The lumbar spine consists of five vertebrae (L1-L5) separated by intervertebral discs, which act as shock absorbers. These vertebrae form a canal that houses the spinal cord and nerve roots. Nerves branch out from the spinal cord through openings called foramina and supply various parts of the body. The lamina forms the back portion of the vertebra and helps protect the spinal cord. When these structures become damaged or degenerate, it can lead to pain, instability, and nerve compression, which may require fusion surgery to restore stability and function.
What You Might Feel – Symptoms (Clinical Presentation)
The symptoms indicating the need for PLIF surgery often involve severe back pain and nerve compression:
- Chronic lower back pain that doesn’t improve with conservative treatments.
- Radiating leg pain (sciatica) due to nerve root compression.
- Numbness, tingling, or weakness in the legs and feet.
- Difficulty walking or maintaining balance, especially when bending backward or walking downhill.
- Muscle weakness or loss of sensation in the lower extremities, especially in severe cases.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis of lumbar spine conditions typically involves:
- Physical Examination: To evaluate the range of motion, reflexes, and signs of nerve damage.
- MRI or CT Scan: To visualize the spinal canal, herniated discs, or any narrowing that might be compressing nerves.
- X-rays: To assess the alignment and structure of the spine.
- Electromyography (EMG): To evaluate nerve function and confirm the presence of nerve compression.
Classification
PLIF is typically classified by the approach used and the number of vertebrae fused:
- Single-Level PLIF: Fusion of one pair of vertebrae.
- Multi-Level PLIF: Fusion of two or more vertebral levels.
- Bilateral PLIF: Fusion performed on both sides of the vertebrae.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may mimic lumbar spinal issues include:
- Piriformis Syndrome: Compression of the sciatic nerve by the piriformis muscle in the buttocks.
- Hip Arthritis: Pain in the lower back or buttocks caused by degenerative changes in the hip joint.
- Kidney Stones: Can cause sharp pain in the lower back, often mistaken for spinal issues.
- Muscle Strains: May cause radiating pain, but typically doesn’t involve nerve compression.
Treatment Options
Non-Surgical Care
- Physical Therapy: Focuses on strengthening the back and improving flexibility.
- Medications: Pain relief through NSAIDs, corticosteroids, or muscle relaxants.
- Epidural Steroid Injections: To reduce inflammation and pain around the spinal nerves.
- Nerve Blocks: To target and alleviate specific pain areas.
Surgical Care
- Posterior Lumbar Interbody Fusion (PLIF): The primary surgical treatment for lumbar instability, performed from the back.
- Anterior Lumbar Interbody Fusion (ALIF): Fusion performed from the front of the spine.
- Minimally Invasive Fusion Techniques: Involves smaller incisions and less tissue disruption to achieve the same fusion outcomes.
Recovery and What to Expect After Treatment
Post-operative care involves:
- Pain Management: Using medications and gradual activity resumption.
- Physical Therapy: To improve strength, mobility, and flexibility.
- Follow-up Appointments: To monitor the fusion process and assess for complications.
- Activity Restrictions: Avoiding heavy lifting or strenuous activity to allow for healing.
Possible Risks or Side Effects (Complications)
Complications may include:
- Infection: At the surgical site.
- Nerve Injury: There is a risk of nerve damage during surgery.
- Bleeding: Excessive bleeding during the procedure.
- Fusion Failure: The vertebrae may not fuse as expected, leading to instability.
- Hardware Failure: Implants like screws or rods may fail.
Long-Term Outlook (Prognosis)
The prognosis for PLIF is generally positive, with most patients experiencing significant pain relief and improved function. The surgery stabilizes the spine, reduces nerve compression, and prevents further degeneration. However, some patients may experience adjacent segment degeneration, where the discs above or below the fused area begin to wear out.
Out-of-Pocket Cost
Medicare
CPT Code 22630 – Posterior Lumbar Interbody Fusion (PLIF) / Transforaminal Lumbar Interbody Fusion (TLIF): $387.42
Under Medicare, 80% of the approved amount for this procedure is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved spinal surgeries like posterior lumbar fusion. These supplemental plans work directly with Medicare to ensure full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or any uncovered charges. Most secondary plans have a modest deductible, typically between $100 and $300, depending on the specific policy and network status.
Workers’ Compensation
If your lumbar spine condition requiring this procedure is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your lumbar spine injury requiring posterior lumbar fusion surgery is caused by a motor vehicle accident, No-Fault Insurance will pay for all medical and surgical costs. The only possible out-of-pocket expense may be a small deductible depending on your specific policy terms.
Example
Michael, a 63-year-old patient with severe lumbar disc degeneration, underwent posterior lumbar interbody fusion (CPT 22630) to relieve nerve compression and stabilize his spine. His estimated Medicare out-of-pocket cost was $387.42. Since Michael had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. How long does it take to recover from PLIF surgery?
A. Recovery typically takes several weeks to a few months, with most patients able to return to normal activities within 6-8 weeks. Full recovery may take several months.
Q. What are the benefits of PLIF over other types of spinal fusion surgery?
A. PLIF provides stability to the spine and alleviates nerve compression while maintaining the natural curvature of the spine. It is especially effective for patients with disc degeneration or instability.
Q. Is PLIF surgery painful?
A. While there is some pain associated with surgery, it is generally less than the pain experienced before the procedure. The minimally invasive approach also reduces post-operative discomfort.
Summary and Takeaway
Posterior Lumbar Interbody Fusion (PLIF) is an effective surgical option for treating various lumbar spine conditions, especially when other treatments have failed. The procedure helps stabilize the spine, relieve nerve compression, and reduce pain. Although risks exist, such as nerve injury or fusion failure, PLIF often leads to significant improvements in pain relief and quality of life.
Clinical Insight & Recent Findings
A recent study aimed to assess the morphological changes in the spinal canal and dural sac cross-sectional area (CSA) following posterior lumbar interbody fusion (PLIF) in patients with lumbar spondylolisthesis. The results indicated a significant increase in both the spinal canal and dural sac CSAs after surgery, with spinal canal CSA increasing by 112.84% and dural sac CSA by 132.99%.
These findings suggest that PLIF not only restores vertebral alignment but also significantly enhances the available space for neural structures, which is critical for alleviating neurological symptoms associated with lumbar spondylolisthesis.
The study highlights the importance of considering these radiological improvements when planning and explaining surgical outcomes to patients. (“Study of spinal morphological change after PLIF – See PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
PLIF surgery is performed by:
- Spine Surgeons: Orthopedic or neurosurgeons specializing in spinal conditions.
- Anesthesiologists: For anesthesia management during surgery.
- Physical Therapists: To assist in rehabilitation and recovery.
When to See a Specialist?
If you experience persistent lower back pain, leg pain, numbness, or weakness that doesn’t respond to conservative treatments, it’s time to consult a spine specialist to discuss the possibility of PLIF surgery.
When to Go to the Emergency Room?
Seek emergency care if you experience:
- Sudden loss of bowel or bladder control.
- Severe, unmanageable pain.
- Sudden weakness or numbness in the legs.
What Recovery Really Looks Like?
Most patients experience significant pain relief and can begin walking shortly after surgery. Full recovery involves physical therapy and avoiding heavy lifting for several months.
What Happens If You Ignore It?
Ignoring symptoms of spinal instability or nerve compression can lead to worsening pain, permanent nerve damage, and decreased mobility. Early intervention with PLIF often results in better long-term outcomes.
How to Prevent It?
Maintaining a healthy weight, exercising regularly to strengthen the back, and practicing good posture can help prevent lumbar spine issues that may require PLIF surgery.
Nutrition and Bone or Joint Health
A balanced diet with adequate calcium and vitamin D supports bone health and reduces the risk of spine degeneration. Proper hydration and a healthy lifestyle are also important for recovery and spinal health.
Activity and Lifestyle Modifications
After surgery, light activities like walking and swimming are encouraged to promote healing. Avoid heavy lifting and high-impact activities until your spine is fully healed.
¿Tienes más preguntas?
What exactly is Posterior Lumbar Interbody Fusion (PLIF)?
PLIF is a surgical procedure that involves fusing one or more vertebral segments in the lower spine. It is performed from the back of the spine and typically involves the placement of a prosthetic cage to maintain disc space and aid in fusion.
How does PLIF relieve pain?
The procedure stabilizes the spine and relieves pressure on the spinal nerves by removing the damaged disc and replacing it with a bone graft and a prosthetic cage, which helps maintain proper spacing and alignment.
Why would someone need a PLIF surgery?
PLIF is often recommended for conditions like degenerative disc disease, spinal instability, scoliosis, spinal deformities, infections, tumors, and cases where previous spinal surgeries have failed.
What type of anesthesia is used during PLIF?
General anesthesia is used, meaning the patient will be completely asleep and unaware during the procedure.
Will I need to stay in the hospital after the surgery?
Yes, most patients stay in the hospital for a few days post-surgery for monitoring and initial rehabilitation.
What kind of physical therapy is required after PLIF?
Physical therapy focuses on strengthening the muscles of the lower back, improving flexibility, and gradually increasing activity levels to aid in recovery and prevent future issues.
How soon can I return to work after PLIF surgery?
his depends on the nature of your job and your individual recovery. Generally, patients may return to sedentary work within 4 to 6 weeks, but physically demanding jobs may require a longer recovery period.
How effective is PLIF in treating chronic back pain?
PLIF is generally effective in treating chronic back pain associated with conditions like degenerative disc disease and spinal instability, with many patients experiencing significant pain relief.
What happens if the fusion does not take?
If the fusion does not occur, additional surgery may be required. This can involve adding more bone graft material, adjusting the hardware, or other techniques to achieve proper fusion.
Is it normal to have pain after PLIF surgery?
Some pain and discomfort are normal after surgery, but it should gradually improve. Persistent or severe pain should be reported to your surgeon.
How will I know if the surgery was successful?
Success is typically measured by a reduction in pain, improvement in function, and evidence of fusion on imaging studies during follow-up visits.
Can PLIF surgery be performed on multiple levels of the spine?
Yes, PLIF can be performed on multiple levels if necessary, depending on the extent of the spinal issues and the surgeon’s assessment.
What should I do if I experience complications after surgery?
Contact your surgeon immediately if you experience symptoms like severe pain, swelling, fever, or any signs of infection or neurological issues.
How can I prepare for PLIF surgery?
Preparation involves medical evaluations, possibly stopping certain medications, arranging for post-operative care at home, and following pre-surgery instructions provided by your healthcare team.

