Epidural injections are corticosteroid injections used to manage several spine conditions. In the epidural injection, the corticosteroid helps to provide relief from radiating back pain caused by lumbar radiculopathy (pinched nerve). The epidural injections form an essential part of the nonsurgical management of sciatica.
Sciatica
Sciatica is the pain in the buttocks that may radiate down to the legs and feet. The pain is commonly associated with a feeling of pins and needles. In severe cases, there may be associated numbness and weakness of the legs.
The sciatic nerve is formed by the nerve roots exiting the neural foramen in the lower spine and functions to control the legs and feet’ muscles. The nerve also provides a conduit for sensation from the lower extremities to the brain.
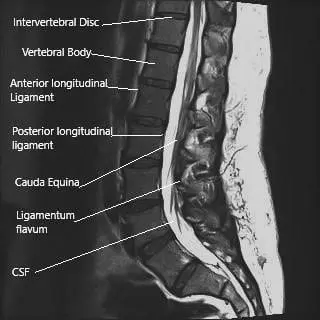
MRI of the lumbosacral spine in sagittal section.
The nerve may be compressed (pinched nerve) or irritated due to a herniated intervertebral disc, narrowing the neural canal due to spinal stenosis, or secondary to degenerative disc disease. The symptoms of sciatica occur due to the inflammation at the site of the compression/irritation. Inflammatory mediators are specific proteins released by certain cells at the site of aggravation.
Mechanism of Action of Corticosteroids
The epidural corticosteroid medications act by reducing the release of inflammatory proteins from cells. The corticosteroid also reduces the release of pain-causing chemicals from the damaged structures such as intervertebral discs. The steroid also acts to reduce the intensity of the pain signals due to inflammation.
The spinal cord ends at the level of lower L1/L2 vertebrae. The spinal cord continues below as a collection of spinal nerve roots that branch from their respective neural foramen. The spinal cord and the bunch of spinal nerves (cauda equina) are covered by a protective covering known as dura mater.
The epidural corticosteroid injections are aimed to be delivered just outside the dura mater (epidural space). The epidural space contains the exiting nerve roots, dural sac, blood vessels, and fat. The epidural corticosteroid injections provide a localized concentration of steroid.
Oral steroid medications have similar effects but act on the entire body rather than only the targeted nerve roots. The systemic administration of the steroid medications through the oral route may cause several side effects; therefore, the epidural route is considered safe while equally or more efficacious.
Role in Sciatica
Epidural injections help control the pain caused by sciatica by reducing the inflammation around the nerve roots. The reduction in pain leads to an improvement in the mobility of the patient. The increased mobility and reduced pain lead to better physical therapy participation to improve the back’s flexibility and strength.
The epidural injections also lead to decreased oral medications such as nonsteroidal anti-inflammatory (NSAID) medications. Long-term use of NSAID medications may cause stomach ulcers and kidney problems. The epidural injections also help to postpone the surgery for sciatica and, in some cases, potentially prevent the need for surgery.
Indications
The epidural corticosteroid injections in sciatica may be used after a trial of other conservative measures. Patients who do not benefit from conservative measures such as medications, physical therapy, heat, cold therapy, etc., for at least 3-4 weeks are candidates for epidural injections.
Types of Epidural Injection
Long-acting corticosteroids include medications such as methylprednisolone and triamcinolone, and short-acting steroids include dexamethasone. Long-acting steroids have a longer duration of action as compared to short-acting steroids.
The steroid medications are usually mixed with a local anesthetic (numbing medicine) such as lignocaine or bupivacaine. The local anesthetic helps to achieve immediate pain relief as it acts to numb the pain signals through the nerves. The steroids may take up to two weeks to start their anti-inflammatory action.
Routes of Epidural Injection
The Injection may be delivered to the epidural space via different routes. Caudal epidural injections utilize an area known as sacral hiatus just above the tailbone. Although easier to perform, the technique involves injecting a large amount of medication and is less efficacious.
The epidural injection is usually administered through the transforaminal or the interlaminar route. The transforaminal route targets the area of the vertebral column where the nerve roots exit the spine. The area is usually the site of compression of the nerve roots, and delivery of steroid medication at this site results in relief of symptoms. The injection is given from the side of the spine.
The interlaminar route utilized the space between the lamina of the two vertebrae. The injection is usually administered from the back of the spine to reach the epidural space.
Procedure
The epidural injections may be performed in a doctor’s office, surgical center, or hospital. The procedure is performed as an outpatient procedure, and the patients are free to go home the same day of the procedure. A fluoroscope or C-ARM machine is used to guide the injection in the epidural space.
The surgeon prepares the injection site to prevent infection and introduces some local anesthetic to numb the skin. A small amount of dye is then introduced to the targeted area. The dye’s spread is visualized under the fluoroscope, and the surgeon determines if the injection is at the correct site.
The corticosteroid, usually mixed with a numbing medication, is administered under live fluoroscopy guidance. The injection site is cleaned, and the patient is monitored for stable vitals, mostly half an hour. The patients can then go home and be instructed to avoid strenuous activities and hot baths or swimming to prevent infection.
Some pain at the injection site is common, and the patients are advised to apply ice at the site. The ice should be used in an ice bag and for no more than 15 mins at a stretch to prevent cold injury.
Success
The epidural injections may lead to relief of symptoms of sciatica for a few weeks to months. The amount of relief may vary in different patients. The epidural injections may be repeated in patients who experience significant relief from symptoms for at least one month.
Contraindications
Active infection or tumor in the body is a contraindication for a steroid injection. Similarly, a patient with bleeding disorders may not be able to receive an epidural injection. The injection may not be administered in patients with uncontrolled blood sugar levels or medical conditions such as osteoporosis or heart diseases.
Complications
There may be complications of a decrease in blood pressure, dizziness, the rise of blood sugar, bleeding, damage to the dural sac/spinal nerves during the procedure. There may be complications of infection, epidural abscess, epidural hematoma, paralysis, etc., after the injection. However, the complication rate is meager, and a vast majority of the patients experience significant relief of symptoms.
Out-of-Pocket Costs
Medicare
CPT Code 62321 – Epidural Steroid Injection (Cervical/Thoracic): $59.36
CPT Code 62323 – Epidural Steroid Injection (Lumbar/Sacral): $58.44
Under Medicare, 80% of the approved cost for these procedures is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, leaving most patients with little to no out-of-pocket expenses for Medicare-approved procedures like epidural steroid injections. These supplemental plans coordinate directly with Medicare to provide full coverage for the injection procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or any uncovered charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on the specific policy and network status.
Workers’ Compensation
If your spinal condition requiring an epidural steroid injection is work-related, Workers’ Compensation will fully cover all treatment-related costs, including the injection and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your injury requiring the epidural steroid injection is related to a motor vehicle accident, No-Fault Insurance will cover the full cost of the procedure. The only possible out-of-pocket cost may be a small deductible depending on your individual policy terms.
Example
Susan, a 65-year-old patient with lumbar radiculopathy, underwent an epidural steroid injection (CPT 62323) for pain relief. Her estimated Medicare out-of-pocket cost was $58.44. Since Susan had supplemental insurance through Blue Cross Blue Shield, the 20% not covered by Medicare was fully paid, leaving her with no out-of-pocket expenses for the injection.
¿Tienes más preguntas?
What exactly is a lumbar epidural injection?
A lumbar epidural injection involves delivering medication, typically a corticosteroid with or without an anesthetic, directly into the epidural space around the spinal cord. The goal is to reduce inflammation and pain associated with sciatica.
What types of medication are used in lumbar epidural injections?
The injections usually contain a corticosteroid, such as methylprednisolone or triamcinolone, which reduces inflammation. Sometimes, a local anesthetic like lidocaine or bupivacaine is also included to provide immediate pain relief.
How does a lumbar epidural injection help with sciatica?
The injection helps by delivering anti-inflammatory medication directly to the area of irritation or compression around the nerve roots, which can reduce swelling, relieve pain, and improve function.
How long do the effects of a lumbar epidural injection last?
The duration of pain relief varies. Some patients may experience relief for several weeks to months, while others may have a shorter duration of relief.
How many injections will I need?
This depends on your response to the first injection. Some patients may benefit from a series of three injections, spaced a few weeks apart, while others may require fewer or more injections.
What are the risks associated with lumbar epidural injections?
Risks are generally low but can include infection, bleeding, headache, nerve damage, or allergic reactions. Rarely, there can be more serious complications like a dural puncture or an epidural hematoma.
Who is a good candidate for a lumbar epidural injection?
Patients with acute or chronic sciatica that hasn’t responded well to conservative treatments like physical therapy, medications, or rest may be good candidates. It’s also suitable for patients looking to delay or avoid surgery.
How effective are lumbar epidural injections for sciatica?
Clinical studies suggest that lumbar epidural injections can provide significant short-term pain relief for many patients. However, the long-term effectiveness is variable, and some patients may not experience significant relief.
What should I expect during the procedure?
During the procedure, you will lie on your stomach or side. After cleaning the injection site, the doctor will numb the area with a local anesthetic. Using X-ray guidance, the doctor will insert a needle into the epidural space and inject the medication.
Will the injection help with back pain as well as leg pain?
Lumbar epidural injections primarily target leg pain (radiculopathy) due to sciatica. They may also help with associated lower back pain, but the primary benefit is usually seen in leg pain relief.
Are there any long-term side effects of lumbar epidural injections?
Long-term side effects are rare, but repeated corticosteroid injections can potentially weaken bones or tendons, and increase blood sugar levels in diabetic patients.
Can I receive a lumbar epidural injection if I am pregnant?
Lumbar epidural injections are generally avoided during pregnancy unless absolutely necessary, due to potential risks to the mother and fetus.
What should I do after the injection to ensure the best results?
After the injection, rest for the remainder of the day. Follow your doctor’s instructions, which may include resuming physical therapy or exercises to strengthen the back and reduce the risk of future flare-ups.

