Snapping hip syndrome, also known as coxa saltans or dancer’s hip, is a condition where patients experience or hear an audible click or snap when moving the hip. The snapping can be painless or accompanied by discomfort. It happens when muscles or tendons slide over bony structures near the hip joint. Over time, this repetitive motion may irritate the surrounding tissues, causing inflammation and pain during everyday activities.
How Common It Is and Who Gets It? (Epidemiology)
Snapping hip affects about 5–10% of the population and is more common among athletes, dancers, and young active adults. It occurs more often in women and individuals who perform repetitive hip movements such as running, jumping, or lifting. Teenagers engaged in ballet or sports are also more susceptible due to muscle tightness and flexibility changes during growth.
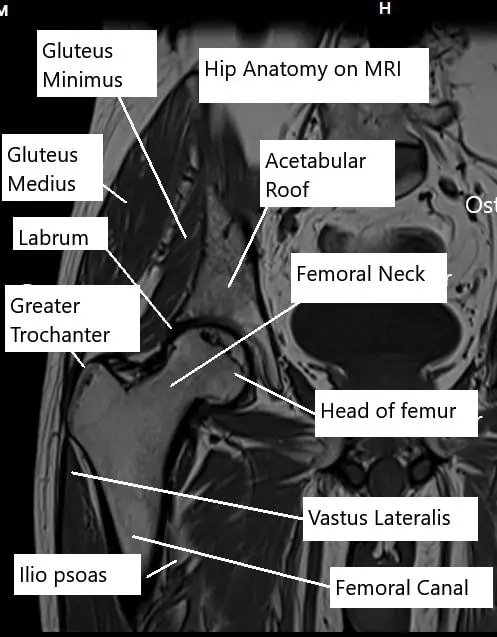
MRI of the hip joint showing various structures
Why It Happens – Causes (Etiology and Pathophysiology)
Snapping hip occurs when tendons or muscles repeatedly move over bony prominences, creating a clicking sensation. The causes can be divided into three types:
Internal snapping
Snapping is caused by tendons passing in front of the Hip joint. The patients’ illicit audible snapping by bending and extending their affected hip, pointing at the area in front of the Hip with their finger. This type of snapping is due to the tendon of the iliopsoas and rectus femoris passing over the knobby head of the femur bone repeatedly.
External snapping
Patients usually report the visible movement of snapping of structures around the later side of the Hip joint. The iliotibial band (ITB) acts like a tight band moving from behind to front over the outer side of Hip while bending the hip.
The greater trochanter is a projection on the outer side of the Hip joint, the ITB when tight moves and accompanies a snapping sensation. Over time the bursae overlying the greater trochanter becomes inflamed and causes pain.
The hamstrings are a large group of muscles behind the Hip joint. The tendon can sometimes cause snapping sound when passing over the ischial tuberosity, also known as the sitting bone.
Intra-articular
Labrum tears and foreign bodies inside the joint capsule cause snapping of the Hip joint. Snapping is usually accompanied by a locking sensation. The labrum and lose bodies cause physical obstruction to the movement of the Hip joint in some positions of the hip.
How the Body Part Normally Works? (Relevant Anatomy)
The hip is a ball-and-socket joint formed by the femoral head (ball) and the acetabulum (socket). Ligaments and muscles stabilize and move the joint, while tendons connect muscles to bone. Fluid-filled bursae cushion these tissues, allowing smooth motion. When the tendons or bands are tight or inflamed, they may rub or “snap” against the bone during hip movement.
What You Might Feel – Symptoms (Clinical Presentation)
The hallmark symptom is a snapping or popping sound during hip movement, such as when walking, standing up, or swinging the leg. Some patients also feel a visible flicking over the side or front of the hip. Pain may develop if bursae or tendons become irritated. Intra-articular snapping can cause catching, locking, or stiffness in the joint.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a detailed medical history and physical examination. The doctor may ask you to reproduce the snapping motion to identify the source. X-rays rule out bony abnormalities, while ultrasound or MRI arthrograms visualize tendons, bursae, and the labrum. In some cases, diagnostic anesthetic injections help pinpoint whether the snapping comes from inside or outside the joint.
Classification
Snapping hip syndrome is classified into:
- External: Caused by the iliotibial band snapping over the greater trochanter.
- Internal: Caused by the iliopsoas or rectus femoris tendon sliding over the front of the joint.
- Intra-articular: Caused by labral tears or loose bodies inside the hip.
Each type has distinct movement patterns and physical exam findings.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may mimic snapping hip include hip bursitis, gluteal tendinopathy, hip impingement, or labral tears. Lower back or sacroiliac joint disorders can also cause referred hip pain. Careful examination and imaging help distinguish between these causes.
Treatment Options
Non-Surgical Care – Most cases improve with conservative treatment:
- Modify or avoid activities that trigger snapping.
- Use over-the-counter pain relievers like acetaminophen or NSAIDs for short-term relief.
- Apply ice to reduce inflammation in acute cases.
- Physical therapy focusing on stretching tight muscles (especially iliotibial band and hip flexors) and strengthening hip stabilizers.
- Corticosteroid injections may relieve bursitis and reduce inflammation.
Surgical Care – Surgery is reserved for persistent cases that do not respond to therapy:
- Arthroscopic surgery uses a camera and small instruments to release tight structures or remove loose bodies. This minimally invasive procedure allows patients to walk the same day.
- Open surgery may be needed for more complex cases to release tight tendons or repair damaged tissues. Recovery is longer but typically successful.
Recovery and What to Expect After Treatment
Most patients recover well with rest and physical therapy, often within weeks to months. Pain relief after steroid injections may occur quickly, while full recovery from arthroscopic surgery typically takes a few months. Consistent stretching and strengthening are key to preventing recurrence.
Possible Risks or Side Effects (Complications)
Potential complications include persistent snapping, inflammation, or temporary weakness from surgery. Recurrence can occur if tightness returns or if stretching is not maintained. Serious complications are rare.
Long-Term Outlook (Prognosis)
The prognosis for snapping hip syndrome is excellent. With appropriate therapy and rehabilitation, most patients regain full hip function and return to normal activities. Surgery has a high success rate when required, and recurrence is uncommon with continued stretching and strengthening.
Out-of-Pocket Costs
Medicare
CPT Code 27006 – Open Iliopsoas Tendon Release (Tenotomy, Hip Flexor, Open): $167.71
CPT Code 27001 – Open Adductor or Iliotibial (IT) Band Release (Tenotomy, Adductor or Fascia Lata): $129.11
CPT Code 20610 – Corticosteroid Injection (Major Joint or Bursa – Hip): $15.12
Medicare Part B typically covers 80% of the approved cost for these procedures once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield usually cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved treatments. These plans coordinate with Medicare to fill the coverage gap and reduce financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans typically cover any remaining balance, including coinsurance or small deductibles, which generally range between $100 and $300, depending on your plan and provider network.
Workers’ Compensation
If your snapping hip syndrome is related to a work injury or repetitive movement at work, Workers’ Compensation will cover all related medical expenses, including surgery, corticosteroid injections, and rehabilitation. You will not have any out-of-pocket costs, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your snapping hip was caused or worsened by an automobile accident, No-Fault Insurance will typically cover the total cost of treatment, including injections or tendon release surgery. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
Samantha Brooks suffered from snapping hip syndrome and underwent an open iliopsoas tendon release (CPT 27006) after unsuccessful conservative treatment. Her estimated Medicare out-of-pocket cost was $167.71. She also received a hip corticosteroid injection (CPT 20610) with an additional $15.12 cost. Since Samantha had supplemental insurance through AARP Medigap, her remaining balance was fully covered, leaving her with no out-of-pocket expenses for her procedures.
Frequently Asked Questions (FAQ)
Q. Is snapping hip dangerous?
A. No. It’s usually harmless, but if pain or inflammation develops, it should be evaluated by a doctor.
Q. Can snapping hip go away on its own?
A, Yes, many cases resolve with rest, stretching, and strengthening exercises.
Q. Will I need surgery?
A. Surgery is rarely needed. It’s only considered when conservative measures fail to relieve symptoms.
Summary and Takeaway
Snapping hip syndrome causes a clicking or popping sound in the hip due to tendons or muscles moving over bony structures. It’s common in athletes and active individuals but rarely serious. Most cases improve with rest, physical therapy, and stretching. For persistent cases, arthroscopic or open surgery can effectively relieve symptoms and restore mobility.
Clinical Insight & Recent Findings
Snapping hip syndrome, particularly external snapping hip, can be a bothersome condition, especially for athletes and those engaging in repetitive motions like running, dancing, or weightlifting. While conservative treatments such as stretching and physical therapy often provide relief, persistent cases may require surgical intervention.
A recent study demonstrated the effectiveness of endoscopic iliotibial band (ITB) release in treating external snapping hip syndrome. In the study, patients who had not found relief through conservative methods experienced significant improvement in their hip function and pain following the endoscopic procedure.
This minimally invasive approach provided relief with minimal complications, making it a viable surgical option for managing this condition. (“Study on endoscopic iliotibial band release for external snapping hip syndrome – see PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Snapping hip syndrome is managed by orthopedic surgeons, particularly those specializing in sports medicine or hip arthroscopy. Physical therapists, radiologists, and rehabilitation specialists play important roles in diagnosis and recovery.
When to See a Specialist?
If hip snapping becomes painful, limits activity, or persists despite home exercises, you should see an orthopedic specialist. Early evaluation prevents chronic irritation and inflammation.
When to Go to the Emergency Room?
Seek emergency care if hip snapping is accompanied by sudden severe pain, inability to move the leg, or symptoms suggesting joint dislocation or infection.
What Recovery Really Looks Like?
Recovery involves consistent physical therapy and gradual stretching of tight muscles. Pain relief may occur within weeks, while full flexibility and strength may take several months. After arthroscopic surgery, walking is allowed immediately, and most patients return to sports in a few months.
What Happens If You Ignore It?
Ignoring snapping hip syndrome can lead to chronic inflammation, bursitis, or persistent pain. Over time, it may limit mobility or affect athletic performance.
How to Prevent It?
Regular stretching of hip flexors, iliotibial band, and gluteal muscles can prevent tightness. Warm up before exercise, use proper technique, and gradually increase activity levels. Avoid repetitive hip movements without rest.
Nutrition and Bone or Joint Health
A balanced diet rich in calcium, vitamin D, and lean protein supports joint health and muscle recovery. Staying hydrated and maintaining a healthy weight reduce stress on the hip joint.
Activity and Lifestyle Modifications
Low-impact activities like swimming or cycling are ideal during recovery. Incorporate flexibility exercises such as yoga or Pilates to maintain mobility. Avoid repetitive, high-impact activities until full strength and flexibility return.
¿Tienes más preguntas?
Can snapping hip syndrome lead to long-term damage or complications in the hip joint?
Snapping hip syndrome typically does not lead to long-term damage or complications in the hip joint, but persistent symptoms may affect quality of life and warrant further evaluation.
Are there different types of snapping hip syndrome, and how do they differ in presentation and treatment?
Yes, snapping hip syndrome can be classified into internal (intra-articular) and external (extra-articular) types, each with distinct causes, symptoms, and treatment approaches.
What diagnostic tests are used to confirm the diagnosis of snapping hip syndrome?
Diagnostic tests for snapping hip syndrome may include physical examination, imaging studies such as X-rays, MRI, or ultrasound, and occasionally diagnostic injections to localize the source of snapping.
Can snapping hip syndrome be treated without surgery, and what nonsurgical treatment options are available?
Yes, many cases of snapping hip syndrome can be successfully managed with nonsurgical treatments such as rest, activity modification, physical therapy, stretching exercises, anti-inflammatory medications, and corticosteroid injections.
Is surgery necessary for all cases of snapping hip syndrome, or are there specific criteria for considering surgical intervention?
Surgery for snapping hip syndrome is typically reserved for cases that do not respond to conservative treatments or when there is significant functional impairment or pain that affects daily activities.
What are the potential risks and complications of surgical treatment for snapping hip syndrome?
Risks and complications of surgical treatment for snapping hip syndrome may include infection, nerve injury, scar tissue formation, persistent pain, and failure to resolve symptoms.
How long does it take to recover from surgery for snapping hip syndrome, and what is the rehabilitation process like?
Recovery from surgery for snapping hip syndrome varies depending on the specific procedure performed and individual patient factors but may involve a period of immobilization followed by gradual rehabilitation to restore strength and mobility.
Can snapping hip syndrome occur in both hips simultaneously, or is it typically unilateral?
Snapping hip syndrome can occur unilaterally or bilaterally, with symptoms manifesting in one or both hips depending on the underlying cause and contributing factors.
Are there any specific exercises or stretches that can help alleviate symptoms of snapping hip syndrome?
Yes, targeted exercises and stretches aimed at improving flexibility, strengthening muscles around the hip joint, and correcting biomechanical imbalances can help alleviate symptoms of snapping hip syndrome.
What lifestyle modifications can individuals with snapping hip syndrome make to reduce symptoms and prevent recurrence?
Lifestyle modifications such as maintaining a healthy weight, avoiding repetitive movements that exacerbate symptoms, and incorporating proper warm-up and cool-down routines into physical activities can help reduce symptoms and prevent recurrence of snapping hip syndrome.
Can snapping hip syndrome be aggravated by certain activities or movements, and if so, which ones should be avoided?
Yes, snapping hip syndrome can be aggravated by activities or movements that involve repetitive hip flexion or extension, such as running, cycling, or certain dance movements. Avoiding or modifying these activities may help alleviate symptoms.
Are there any specific risk factors that predispose individuals to developing snapping hip syndrome?
Yes, risk factors for snapping hip syndrome may include participation in sports or activities that involve repetitive hip movements, tight hip muscles or tendons, structural abnormalities in the hip joint, and previous hip injuries.
Can snapping hip syndrome be a sign of a more serious underlying hip condition, such as hip impingement or labral tear?
Yes, in some cases, snapping hip syndrome may be associated with underlying hip conditions such as femoroacetabular impingement (FAI) or labral tears, which may require further evaluation and treatment.
How does the age of the individual impact the likelihood of developing snapping hip syndrome?
Snapping hip syndrome can occur in individuals of any age but may be more common in younger individuals, particularly athletes or dancers, due to increased hip mobility and participation in activities that stress the hip joint.
Can snapping hip syndrome affect athletic performance, and if so, are there strategies athletes can use to manage symptoms while continuing to participate in sports?
Yes, snapping hip syndrome can affect athletic performance by causing pain, discomfort, or limitations in movement. Athletes can work with sports medicine professionals to develop strategies for managing symptoms while optimizing performance, such as modifying training techniques or using supportive braces.
How does the severity of snapping hip syndrome influence treatment decisions, and are there different treatment approaches for mild versus severe cases?
Treatment decisions for snapping hip syndrome are influenced by the severity of symptoms and functional impairment. Mild cases may respond well to conservative treatments, while severe or refractory cases may require surgical intervention.
Can snapping hip syndrome cause referred pain or symptoms in other areas of the body, such as the lower back or knee?
Yes, snapping hip syndrome may cause referred pain or symptoms in other areas of the body, such as the lower back or knee, due to compensatory movements or altered biomechanics. Addressing the underlying hip dysfunction can help alleviate these secondary symptoms.
Are there any specific precautions individuals with snapping hip syndrome should take to prevent exacerbating symptoms during daily activities or exercise?
Yes, individuals with snapping hip syndrome may benefit from avoiding activities or movements that exacerbate symptoms, using proper body mechanics and posture, and incorporating regular stretching and strengthening exercises into their routine to maintain hip joint health.
Can snapping hip syndrome spontaneously resolve without treatment, or does it typically require intervention to improve symptoms?
Snapping hip syndrome may spontaneously resolve without treatment in some cases, particularly if it is caused by temporary muscle tightness or overuse. However, persistent or recurrent symptoms may require intervention to address underlying biomechanical issues.
How does the location of the snapping sensation (front, side, or back of the hip) influence the diagnostic approach and treatment plan?
The location of the snapping sensation in the hip (front, side, or back) can provide clues to the underlying cause of snapping hip syndrome and may influence the diagnostic approach and treatment plan. For example, anterior snapping may be related to iliopsoas tendon impingement, while lateral snapping may involve the iliotibial band or greater trochanter.
Can snapping hip syndrome be exacerbated by specific movements or positions, such as sitting for prolonged periods or climbing stairs?
Yes, snapping hip syndrome may be exacerbated by specific movements or positions that place stress on the hip joint, such as sitting for prolonged periods with the hip flexed or climbing stairs, which can increase friction or tension on the affected structures.
Are there any dietary or nutritional supplements that may help alleviate symptoms of snapping hip syndrome or support hip joint health?
While dietary or nutritional supplements alone may not directly treat snapping hip syndrome, maintaining a balanced diet rich in essential nutrients such as calcium, vitamin D, and omega-3 fatty acids may support overall musculoskeletal health and potentially reduce inflammation in the hip joint.

