Cortisone injections are used to reduce pain and inflammation in joints, tendons, and bursae. These injections are commonly given in the knee and shoulder but may also be used in the elbow, hip, ankle, wrist, and spine.
How Common It Is and Who Gets It? (Epidemiology)
Cortisone injections are widely used in people with arthritis and painful joint conditions. They are common because they offer relief without surgery and can be used for many joints throughout the body.
Why It Happens – Causes (Etiology and Pathophysiology)
Inflammation inside a joint, tendon, or bursa causes pain, swelling, and stiffness. Conditions like osteoarthritis, inflammatory arthritis, gout, and tendon irritation often lead to inflammation that may require a cortisone shot.
How the Body Part Normally Works? (Relevant Anatomy)
Joints, tendons, and bursae allow smooth motion. When these tissues become inflamed, the area becomes painful and swollen. Cortisone helps reduce inflammation so the joint or tendon can move more comfortably.
What You Might Feel – Symptoms (Clinical Presentation)
Patients often report pain, swelling, reduced movement, and discomfort during activity. Some may also have redness or tenderness in the affected joint.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis is made by physical examination. Doctors confirm that there is no active infection and review medications such as blood thinners before giving the injection.
Classification
Cortisone injections may be classified based on the size of the joint:
Large joints such as knee, hip, or shoulder.
Medium joints such as elbow, wrist, or ankle.
Small joints such as fingers and toes.
Other Problems That Can Feel Similar (Differential Diagnosis)
Joint pain may also be caused by fractures, ligament injuries, infections, or other sources of inflammation.
Treatment Options
Non-Surgical Care
Cortisone injections reduce pain and swelling. They can also help with conditions involving bursae and tendons. Ice, anti-inflammatory medication, and activity modification may also be used.
Surgical Care
Cortisone injections are a non-surgical treatment. Surgery is not part of the injection process.
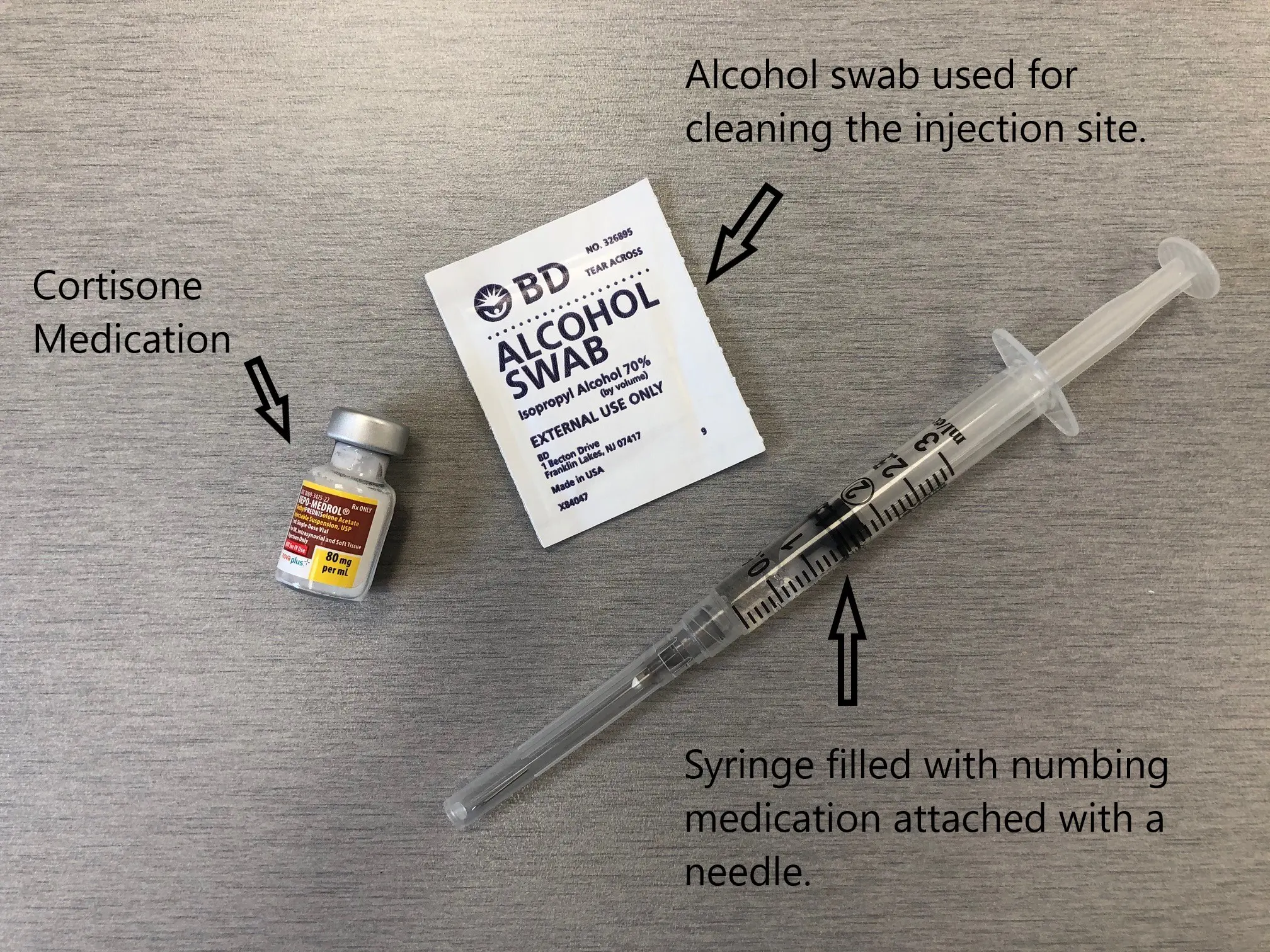
Cortisone vial, alcohol swab, and the syringe.
Conditions
The injection is most commonly given for osteoarthritis by orthopedic surgeons. The injection may also be used for joint pain caused by inflammatory arthritis such as rheumatoid arthritis and psoriatic arthritis. The shots may also be given for painful joint conditions such as gout. The steroid injections are helpful in back pain and inflammation of bursae and tendons.
Mechanism of action
The injections contain a steroid medication that is delivered locally in the joint, tendon, or bursae. The adrenal glands naturally release the steroid in the body. The steroids help to dampen the immune system and reduce inflammation. The reduction in inflammation leads to relief from pain and swelling.
Benefits of Cortisone Injections
Cortisone injections offer several benefits for individuals suffering from knee pain:
Pain Relief: Cortisone injections can provide significant pain relief, allowing you to resume activities that were previously difficult due to knee discomfort.
Improved Mobility: By reducing inflammation, cortisone injections can improve knee joint function and increase range of motion, making it easier to move around.
Non-Surgical Option: Cortisone injections offer a non-surgical alternative for managing knee pain, avoiding the need for invasive procedures in many cases.
Fast Acting: Many people experience relief shortly after receiving a cortisone injection, with the full effects usually kicking in within a few days to a week.
Long-lasting Relief: While cortisone injections may not provide permanent relief, the effects can last for several weeks to several months, allowing you to enjoy an extended period of pain-free living.
Procedure
The patients may receive a cortisone shot in the doctor’s office as an outpatient procedure. Before the procedure, the physician ensures that the patient is not on any blood thinners and is not having any active infection. Diabetic patients must have their blood sugar levels well-controlled before the shot as the blood sugar levels may shoot up after the injection.
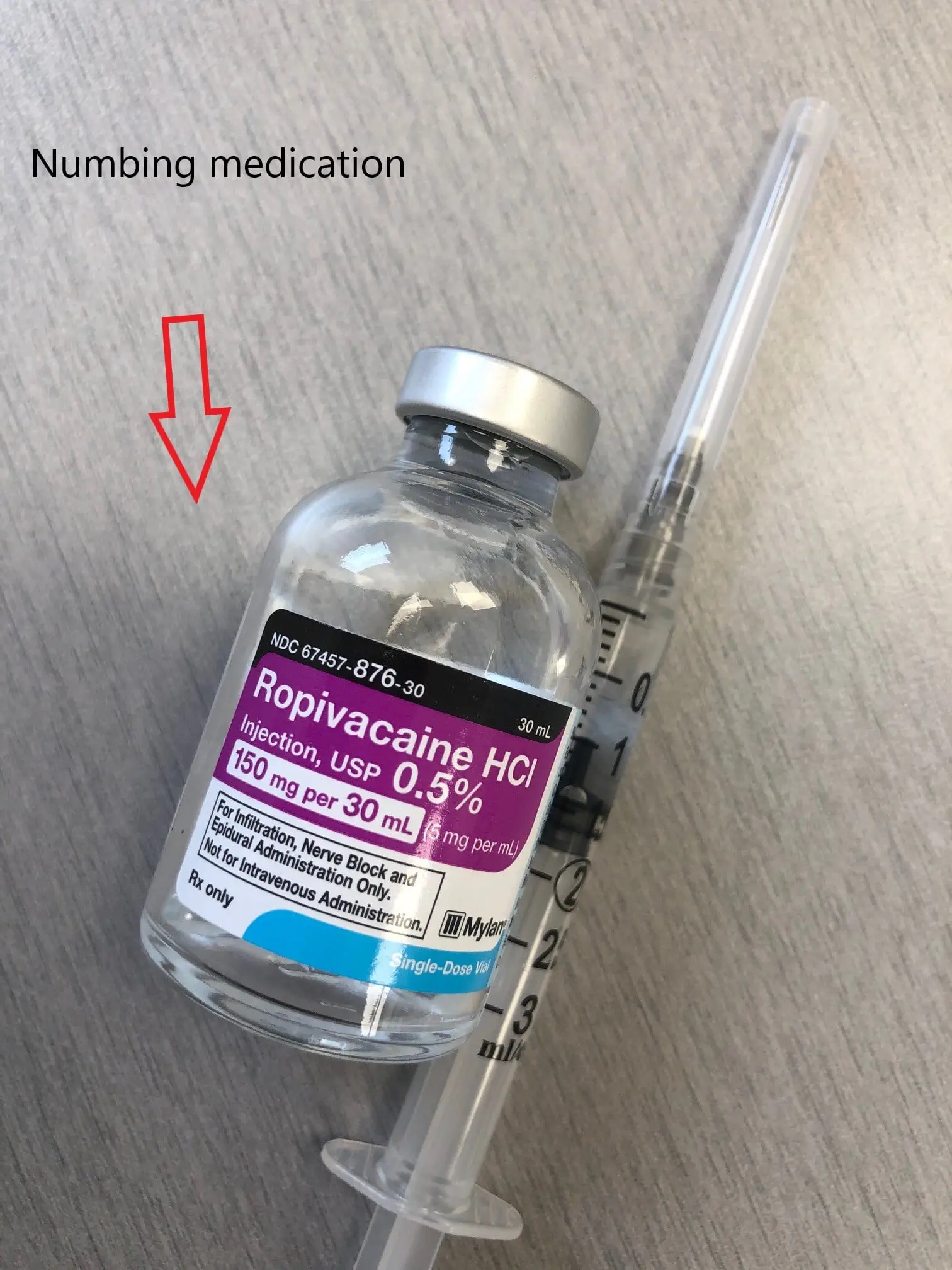
Numbing medication is usually injected along with the cortisone to provide immediate pain relief.
The patient is positioned for easy access to the involved joint. The site of injection and the adjacent area is cleaned with a povidone-iodine solution. Numbing medication is applied to the location of injection, to make it the injection less painful.
The physician marks the site of needle insertion with a sterile marker, and the injection is delivered. The injection site is covered with a sterile dressing. Often the physician might also use ultrasound guidance to deliver the injection at the correct location.
Post injection, the patient is advised to apply ice and take over the counter nonsteroidal anti-inflammatory and pain medications as needed for 1-3 days. Pain and redness are common short term side effects after injections and usually subside within 1-2 days. Patients are advised to keep the dressing dry for at least a day and avoid hot tub baths for a day. The patients are also encouraged to watch for any signs of infection.
Recovery and What to Expect After Treatment
After the injection, patients may apply ice and take over-the-counter anti-inflammatory medicine for one to three days. Pain and redness may occur briefly and usually fade within one to two days. The dressing should remain dry for at least a day, and hot tubs should be avoided for a day.
Possible Risks or Side Effects (Complications)
Frequent injections may damage cartilage or thin the bone or nearby tissues. Risks include joint infection, nerve irritation, tendon weakening, increased pain right after the shot, temporary facial redness, and increased blood sugar levels in diabetic patients.
Long-Term Outlook (Prognosis)
Most patients feel relief after a few days. Pain reduction may last for several months or even up to a year. Some may need repeat injections if symptoms return.
Out-of-Pocket Costs
Medicare
CPT Code 20610 – Large Joint Injection: $15.12
CPT Code 20605 – Medium Joint Injection: $12.58
CPT Code 20600 – Small Joint Injection: $12.36
Medicare typically covers most of the approved charge for these injection procedures, leaving you responsible for the usual twenty percent co-insurance. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield often remove that remaining portion completely. These plans are designed to work with Medicare by filling in the cost gap so most patients end up with little or no financial responsibility when the injection is a Medicare-approved service.
Secondary insurance plans, including employer-based coverage, TRICARE, or the Veterans Health Administration, become the next payer after Medicare and the supplemental plan. Once any deductible is met — commonly between one hundred and three hundred dollars — the secondary plan may cover the remaining balance. This often reduces or eliminates any remaining out-of-pocket cost for joint injections.
Workers’ Compensation
If the joint issue requiring the injection comes from a work-related injury, Workers’ Compensation covers the entire treatment. You will not have any out-of-pocket expense.
No-Fault Insurance
If the joint problem is related to a motor vehicle accident, No-Fault Insurance covers the cost of the injection. The only possible patient responsibility would be a small deductible depending on your policy.
Example
A patient received a large joint injection for persistent knee pain. Under Medicare, the estimated out-of-pocket cost would have been 15.12 dollars. Because the patient also had secondary insurance, the remaining balance was paid in full, leaving the patient with no out-of-pocket expense.
Frequently Asked Questions (FAQ)
Q. How long does it take for cortisone to work?
A. Relief usually starts after a few days.
Q. How long does the relief last?
A. Relief can last weeks to months and sometimes up to a year.
Q. Can I get cortisone injections often?
A. Frequent injections are avoided to prevent damage to cartilage and nearby tissues.
Q. Do injections hurt?
A. A numbing medicine is usually used to reduce discomfort.
Q. Do they raise blood sugar?
A. Yes. Diabetic patients may see a temporary rise in blood sugar.
Summary and Takeaway
Cortisone injections help reduce pain and inflammation in joints and tendons. They provide relief for many conditions and may last for months. While generally safe, they have risks that should be discussed with a doctor. When used carefully, cortisone injections can help patients move more comfortably and return to daily activities.
Clinical Insight and Recent Findings
A recent study evaluating cortisone injections for knee osteoarthritis found that patients experienced meaningful pain relief within two weeks, and the presence or absence of joint effusion on ultrasound did not significantly change how well the injection worked.
These findings support what your overview describes: cortisone reduces inflammation locally and can quickly improve mobility and comfort, regardless of whether swelling is visible on imaging. (“Study of cortisone response in knee osteoarthritis – See PubMed.”)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons and other trained providers perform cortisone injections. Medical assistants and nurses help with preparation and post-procedure care.
When to See a Specialist?
See a specialist when joint pain, swelling, or stiffness continues despite rest and medication.
When to Go to the Emergency Room?
Emergency evaluation is needed for severe redness, fever, uncontrolled pain, or signs of infection after the injection.
What Recovery Really Looks Like?
A small amount of soreness is normal shortly after the shot. Most patients feel improvement within a few days and may return to normal activity as pain decreases.
What Happens If You Ignore It?
If inflammation continues untreated, pain and swelling may worsen and joint movement may become more limited.
How to Prevent It?
Joint protection, proper activity modification, and early treatment of inflammation can reduce the need for injections.
Nutrition and Bone or Joint Health
A balanced diet supports joint health and overall recovery. Good hydration and healthy food choices help reduce inflammation.
Activity and Lifestyle Modifications
Patients may return to activity as comfort allows, avoiding overuse or heavy strain on the joint. Ice and rest may help if pain returns.
¿Tienes más preguntas?
How long does it take for cortisone injections to start working?
Cortisone injections typically start providing relief within a few days to a week after the injection.
How often can cortisone injections be administered?
Cortisone injections can be given every few months if necessary, but frequent injections may increase the risk of side effects.
Are cortisone injections suitable for all types of knee pain?
Cortisone injections are most effective for knee pain caused by inflammation, such as arthritis, bursitis, and tendinitis. They may not be as effective for other types of knee conditions, such as structural damage or severe degeneration.
Can cortisone injections be used alongside other treatments?
Yes, cortisone injections can be used in conjunction with other treatments such as physical therapy, medications, and lifestyle modifications to manage knee pain effectively.
Are cortisone injections painful?
The injection itself may cause some discomfort, but most people find the procedure tolerable. Your healthcare provider may use a local anesthetic to numb the area beforehand.
How long does the pain relief from cortisone injections last?
The duration of pain relief varies from person to person but can last from several weeks to several months.
Can cortisone injections cure knee pain permanently?
Cortisone injections provide temporary relief by reducing inflammation, but they do not cure the underlying cause of knee pain.
Are there any alternatives to cortisone injections for knee pain relief?
Yes, alternatives include physical therapy, oral medications, hyaluronic acid injections, platelet-rich plasma (PRP) therapy, and surgical options for severe cases.
How soon after a cortisone injection can I resume normal activities?
You may be able to resume normal activities immediately after the injection, but it’s best to avoid strenuous activities for a day or two to allow the medication to take effect.
Can cortisone injections cause weight gain?
Cortisone injections can cause temporary fluid retention, which may lead to slight weight gain in some individuals. However, this effect is usually minor and resolves on its own.
Are cortisone injections safe for long-term use?
While cortisone injections are generally safe for occasional use, long-term use may increase the risk of side effects such as joint damage and osteoporosis. Your healthcare provider will monitor your condition and adjust treatment accordingly.
Can cortisone injections worsen knee pain?
In rare cases, cortisone injections may initially worsen symptoms before providing relief. This is known as a “cortisone flare” and usually resolves on its own within a few days.
Are cortisone injections effective for all types of arthritis?
Cortisone injections can provide relief for arthritis-related knee pain, but their effectiveness may vary depending on the type and severity of arthritis.
Can cortisone injections be used to treat knee pain in children?
Cortisone injections may be considered for children with severe knee pain caused by conditions such as juvenile arthritis, but they are typically used cautiously and under close medical supervision.
How do cortisone injections compare to other knee pain treatments in terms of effectiveness?
Cortisone injections are often effective for providing short-term pain relief and reducing inflammation. However, their effectiveness may vary depending on individual factors and the specific cause of knee pain.
Can cortisone injections be used to treat knee pain during pregnancy?
Cortisone injections are generally avoided during pregnancy unless the benefits outweigh the potential risks. Alternative treatments may be considered for managing knee pain during pregnancy.
Are cortisone injections covered by insurance?
Cortisone injections are typically covered by insurance when deemed medically necessary for the treatment of knee pain. However, coverage may vary depending on your insurance plan and specific circumstances.
Can cortisone injections be used to treat knee pain in athletes?
Cortisone injections may be considered for athletes with knee pain caused by inflammation or overuse injuries. However, it’s essential to weigh the potential benefits and risks, especially in high-performance athletes.
Can cortisone injections interfere with other medications I’m taking?
Cortisone injections may interact with certain medications, so it’s essential to inform your healthcare provider about all medications, supplements, and herbal remedies you are taking before receiving a cortisone injection.
How long does it take for cortisone injections to wear off?
The effects of cortisone injections typically wear off gradually over time, ranging from several weeks to several months, depending on individual factors and the specific condition being treated.
Can cortisone injections be used to treat knee pain in older adults?
Cortisone injections can be used to treat knee pain in older adults, but they may be used cautiously due to the increased risk of side effects such as osteoporosis and joint damage.
Can cortisone injections be used to treat knee pain in individuals with diabetes?
Cortisone injections can be used to treat knee pain in individuals with diabetes, but close monitoring of blood sugar levels is essential, as cortisone injections can temporarily raise blood sugar levels.
Are cortisone injections effective for all types of knee injuries?
Cortisone injections may be effective for certain types of knee injuries, such as ligament sprains, tendonitis, and bursitis, but their effectiveness may vary depending on the specific injury and individual factors.
Can cortisone injections be administered by a primary care physician, or do I need to see a specialist?
Cortisone injections can be administered by a primary care physician or a specialist such as an orthopedic surgeon or rheumatologist, depending on your specific healthcare needs and the availability of services in your area.

