Gender-specific knee replacement is a type of knee replacement surgery designed to match differences between male and female knee anatomy. It is based on the same goals as traditional knee replacement: reducing pain, improving movement, and helping people return to daily activities.
How Common It Is and Who Gets It? (Epidemiology)
Knee replacement surgery is common in people with severe arthritis. Gender-specific implants are newer and used less often than traditional implants. They are designed mainly for females but may not be necessary for every patient.
Why It Happens – Causes (Etiology and Pathophysiology)
Osteoarthritis causes the cartilage of the knee to wear away, leading to pain, stiffness, and disability. When symptoms become severe and nonsurgical treatments are not enough, knee replacement surgery may be recommended.
How the Body Part Normally Works? (Relevant Anatomy)
The knee joint is formed by the thigh bone, shin bone, and kneecap. Men and women have some differences in knee shape. Males tend to have a wider femur and deeper groove for the kneecap. Women tend to have smaller bone sizes and different muscle attachment angles. These differences inspired the development of gender-specific implants.
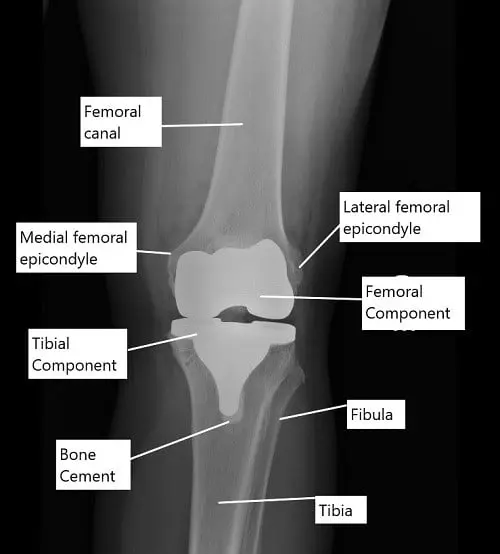
X-ray showing a total knee replacement in AP view.
The thigh muscles in front of the knee (quadriceps) that are responsible for straightening the leg are attached to the kneecap via the quadriceps tendon. The kneecap is attached to the upper end of the shin bone (tibia) via the patellar tendon. The angle formed by the thigh muscles’ attachment with the kneecap is different in males and females.
What You Might Feel – Symptoms (Clinical Presentation)
Patients usually experience knee pain, stiffness, swelling, reduced movement, and difficulty doing daily activities. These symptoms may worsen over time.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis is confirmed with physical examination and imaging such as X-rays. These tests show the severity of arthritis and help determine whether knee replacement is needed.
Classification
Knee replacement implants can be:
Traditional off-the-shelf implants in various sizes.
Gender-specific implants designed to match female anatomy.
Both are used to treat severe arthritis.
Other Problems That Can Feel Similar (Differential Diagnosis)
Symptoms may also come from ligament injuries, meniscus tears, inflammatory arthritis, or hip or spine problems that cause referred pain.
Treatment Options
Non-Surgical Care
Before surgery, most patients try options such as physical therapy, medications, weight management, or injections. These may help temporarily.
Surgical Care
Knee replacement removes damaged bone and replaces it with metal and plastic components. Gender-specific implants have a smaller side-to-side width, adjusted front-to-back length, and improved kneecap tracking designed for female knee anatomy. Traditional implants remain highly successful and are still widely used.
Knee replacement biomechanics
Knee replacement surgery is most commonly done to treat end-stage osteoarthritis. During the surgery, the bony ends forming the knee joint are replaced with metal alloy prosthetic parts. The lower end of the femur is replaced with a femoral component and the upper part of the tibia is replaced with a tibial component.
The size of the prosthetic metal implants is determined by the size of the bone removed during the surgery. The surgeon cuts the bone to remove the arthritic bone and as well as to correct any deformity caused by arthritis. The implants are capped at the bony ends using special bone cement.
The undersurface of the kneecap (patella) is usually covered by a prosthetic plastic part. A polyethylene plastic spacer is introduced in between the metal parts to smooth the movement and provide stability.
Balancing the knee joint is an important part of knee replacement surgery. The surgeon tries to equalize and balance the forces acting in front, back, and the sides of the knee. The balancing ensures that the prosthetic knee joint is stable and allows movement in the natural range of motion.
Gender-specific implants
A balanced prosthetic knee joint allows movements that closely resemble the natural knee. A balanced and stable knee joint also ensures the implants would last for many years or even a lifetime.
Traditionally, the size of implants used during the surgery is “off the shelf” implants. The off the shelf implants come in different sizes. Traditional implants are made to resemble an average knee and with sizes small and large.
The surgeon measures the amount of bone removed during the surgery and depending upon the size choose the best fitting off-the-shelf implants. Gender-specific implants are made keeping in mind the anatomy of the female knee.
While the traditional implant sizes used in females have been extremely successful, gender-specific implants were recently introduced to potentially make the implants resemble the natural knee as close as possible.
The gender-specific implants for female knees have a smaller medial to lateral distance so they resemble the natural knee. The front-to-back distance of the implant also closely matched the natural knee.
The modification in gender-specific implants prevents overhang or underhanging of the implant which may be encountered in traditional off-the-shelf implants. The patellar tracking is also optimized for the female anatomy in gender-specific implants.
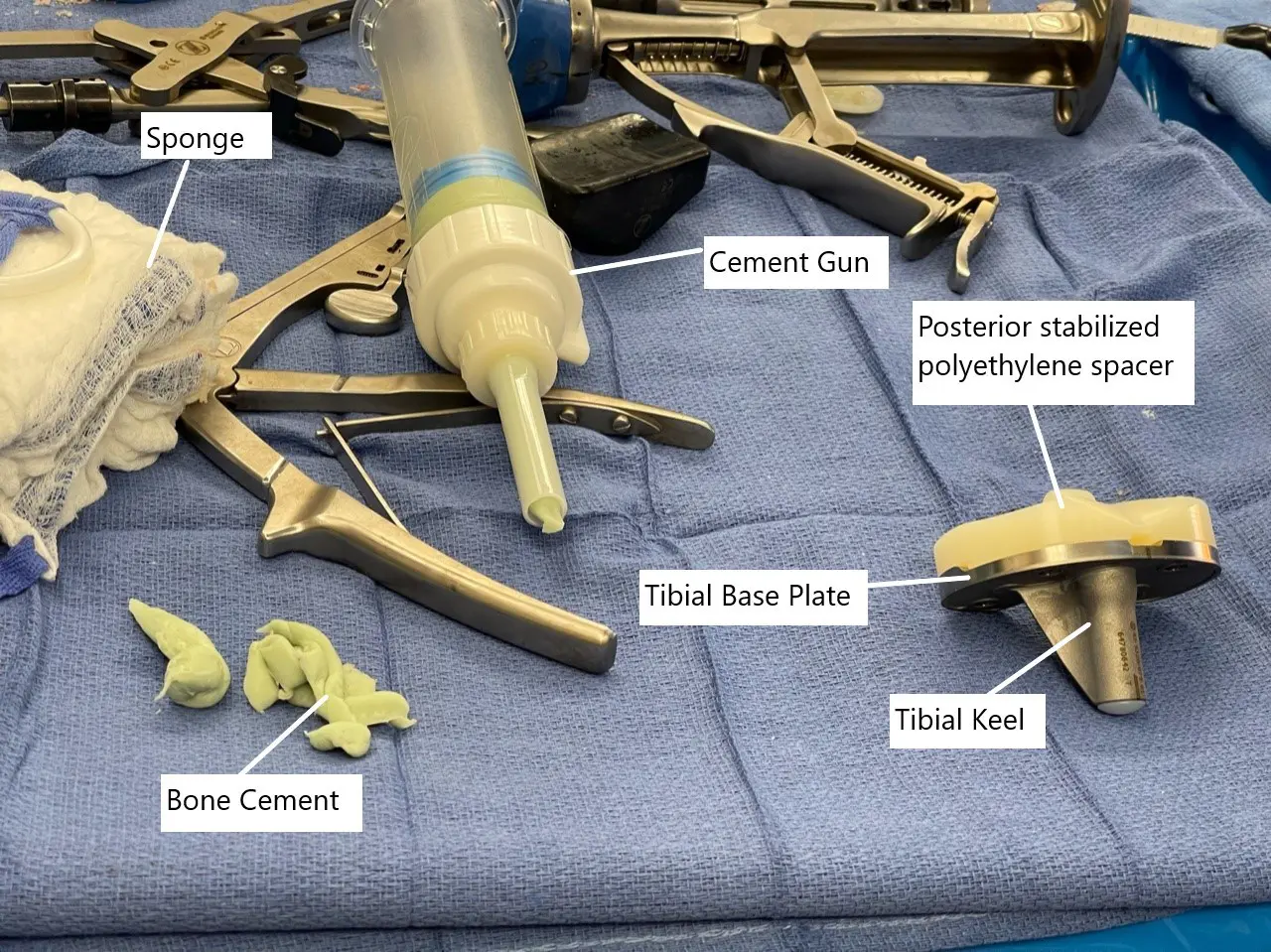
Intraoperative image showing the tibial component with polyethylene spacer.
Potential Benefits of Gender-Specific Knee Replacement:
Improved Fit and Function: By customizing the implant to match the individual’s anatomy, gender-specific knee replacement may result in better fit and alignment, leading to improved stability and range of motion.
Reduced Risk of Complications: A better-fitting implant may reduce the risk of complications such as implant loosening, dislocation, and uneven wear, which can prolong the lifespan of the artificial joint.
Enhanced Patient Satisfaction: With a knee replacement that feels more natural and comfortable, patients may experience higher satisfaction levels and better outcomes following surgery.
Considerations for Gender-Specific Knee Replacement
While gender-specific knee replacement offers promising benefits, there are several factors to consider before opting for this approach:
Individual Variability: Despite gender differences in knee anatomy, there is considerable variability among individuals. Therefore, the decision to pursue gender-specific implants should be based on a comprehensive assessment of each patient’s unique anatomical characteristics.
Surgical Expertise: Gender-specific knee replacement requires specialized surgical techniques and expertise. Surgeons should undergo proper training and have experience in performing these procedures to ensure optimal outcomes.
Cost Considerations: Gender-specific implants may be associated with higher costs compared to traditional implants. Patients should weigh the potential benefits against the additional expenses and consider factors such as insurance coverage and financial resources.
Long-Term Data: While early studies suggest positive outcomes with gender-specific knee replacement, long-term data on durability, effectiveness, and patient satisfaction are still evolving. Patients should discuss the latest research findings and consult with their healthcare provider to make informed decisions.
Recovery and What to Expect After Treatment
Recovery involves physical therapy, walking with assistance soon after surgery, and strengthening muscles. Most people return to daily activities gradually as swelling decreases and motion improves.
Possible Risks or Side Effects (Complications)
Risks are the same as traditional knee replacement, including infection, blood clots, stiffness, fractures, or issues with implant position. Gender-specific implants have no unique risks beyond those of standard knee replacement.
Long-Term Outlook (Prognosis)
Knee replacements, including gender-specific implants, are highly successful. Traditional implants can last 20 years or longer. Gender-specific implants may offer benefits in fit and feel, but long-term data is still being collected.
Out-of-Pocket Cost
Medicare
CPT Code 27447 – Gender-Specific Total Knee Replacement: $303.02
Medicare generally pays most of the approved charge for this type of knee replacement, leaving patients with the standard twenty percent share. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield usually cover that remaining portion. These supplemental plans work alongside Medicare to remove the co-insurance gap, so patients often have little to no remaining financial responsibility when the surgery is Medicare-approved.
Secondary insurance, including employer-based plans, TRICARE, or the Veterans Health Administration, acts as the next payer after Medicare. Once the secondary deductible is met — typically between $100 and $300 — the plan may pay the remaining balance connected to the knee replacement. This frequently reduces or eliminates any leftover expense.
Workers’ Compensation
If your need for a gender-specific knee replacement is tied to a work-related injury, Workers’ Compensation covers the entire cost of the operation and recovery. This leaves you with no out-of-pocket cost.
No-Fault Insurance
If the knee condition came from a motor vehicle accident, No-Fault Insurance covers the complete procedure. Your only responsibility may be a small deductible depending on your policy.
Example
A patient required a gender-specific total knee replacement due to severe arthritis and persistent pain. With Medicare, the estimated out-of-pocket cost was $303.02. Because the patient also had secondary insurance, the remaining portion was covered fully, resulting in no out-of-pocket expense.
Frequently Asked Questions (FAQ)
Q. Are gender-specific implants only for women?
A. They are designed for female anatomy but traditional implants often work well for both men and women.
Q. Do gender-specific implants last longer?
A. There is no long-term data yet to show they last longer than traditional implants.
Q. Do they feel more natural?
A. Some designs aim to mimic natural movement more closely, but results vary between patients.
Q. Are they more expensive?
A. They may cost more depending on the manufacturer and insurance coverage.
Q. Should everyone choose a gender-specific implant?
A. Not necessarily. The choice depends on anatomy, surgeon preference, and patient goals.
Summary and Takeaway
Gender-specific implants are designed with the anatomy of female knees in mind. They may improve fit, alignment, and comfort. However, traditional implants remain highly successful, and long-term research is still being completed. The best implant choice depends on individual needs and surgeon guidance.
Clinical Insight and Recent Findings
A recent study reviewing knee implant designs found that traditional components often struggle to match natural knee geometry—particularly variations in femoral shape, tibial slope, and joint-line orientation—which can influence outcomes such as stability, comfort, and patient satisfaction.
These findings relate directly to the concept of gender-specific knee replacement, which aims to address known anatomical differences between men and women by refining implant dimensions and patellar-tracking profiles.
While your overview explains that gender-specific designs offer a closer fit for some female patients but still lack long-term evidence, the study reinforces the broader point: implant shape and alignment matter, and improving conformity between prosthetic components and native anatomy may reduce complications and improve function. (“Study of knee implant geometry and personalized design – See PubMed.”)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons perform knee replacement surgery. The team includes anesthesiologists, nurses, and physical therapists who assist with recovery.
When to See a Specialist?
A specialist should be consulted when knee arthritis causes severe pain, reduced movement, or difficulty doing daily tasks despite nonsurgical treatments.
When to Go to the Emergency Room?
Emergency care is needed for sudden severe swelling, fever, uncontrolled pain, or signs of infection after surgery.
What Recovery Really Looks Like?
Recovery includes managing swelling, doing physical therapy, and slowly increasing activity. Most patients gain strength and motion over weeks to months.
What Happens If You Ignore It?
Ignoring severe arthritis may lead to worsening pain, deformity, and decreasing mobility, making daily life more difficult.
How to Prevent It?
Arthritis cannot always be prevented, but staying active, maintaining healthy weight, and treating injuries early may help reduce strain on the knee.
Nutrition and Bone or Joint Health
Balanced meals support healing after knee replacement. Adequate protein, hydration, and healthy foods help in recovery.
Activity and Lifestyle Modifications
After surgery, patients gradually return to activities. Avoiding high-impact stress on the knee helps protect the implant and maintain long-term function.
¿Tienes más preguntas?
How do I know if I’m a suitable candidate for gender-specific knee replacement?
Your orthopedic surgeon will assess various factors, including your knee anatomy, medical history, and severity of knee symptoms, to determine if gender-specific knee replacement is appropriate for you.
Are there any specific age requirements for undergoing gender-specific knee replacement?
Age alone is not a determining factor. The suitability for surgery depends more on your overall health, extent of knee damage, and your goals for surgery.
How long does the recovery process take after gender-specific knee replacement surgery?
Recovery time varies from person to person but typically involves several weeks of rehabilitation and physical therapy to regain strength, flexibility, and mobility in the knee.
Can gender-specific knee replacement surgery be performed using minimally invasive techniques?
Yes, minimally invasive approaches can be utilized for gender-specific knee replacement surgery, resulting in smaller incisions, less tissue damage, and potentially faster recovery.
What are the potential risks and complications associated with gender-specific knee replacement?
Common risks include infection, blood clots, implant loosening, and nerve or blood vessel injury. However, these risks are generally low with proper surgical technique and postoperative care.
How long do gender-specific knee replacement implants typically last?
The longevity of knee implants can vary depending on factors such as patient activity level, implant design, and overall health. On average, knee replacements can last 15-20 years or longer with proper care.
Are there any restrictions on physical activities after gender-specific knee replacement surgery?
While you may be able to resume many activities, high-impact or strenuous activities like running and jumping may be discouraged to avoid excessive wear on the implant.
Will I still need regular follow-up appointments with my orthopedic surgeon after gender-specific knee replacement surgery?
Yes, regular follow-up appointments are essential to monitor your progress, address any concerns, and ensure the long-term success of your knee replacement.
Can gender-specific knee replacement surgery be performed on both knees simultaneously?
Depending on your overall health and the recommendation of your surgeon, bilateral (both knees) gender-specific knee replacement surgery may be an option for some patients.
How soon can I expect to experience relief from knee pain after gender-specific knee replacement surgery?
Many patients experience significant pain relief shortly after surgery, although full recovery and optimal pain relief may take several weeks to months.
Are there any alternative treatments to gender-specific knee replacement for managing knee pain?
Depending on the severity of your knee symptoms, alternative treatments such as medication, physical therapy, injections, or other surgical procedures may be explored before considering knee replacement surgery.
Will I need to undergo any preoperative tests or evaluations before gender-specific knee replacement surgery?
Yes, your surgeon may order preoperative tests such as blood work, imaging scans, and a comprehensive physical examination to assess your overall health and identify any potential risks
How soon can I return to work or regular daily activities after gender-specific knee replacement surgery?
The timing of your return to work and daily activities will depend on factors such as your job requirements, the type of surgery performed, and your rate of recovery. Your surgeon will provide specific guidance based on your individual circumstances.
What steps can I take to optimize my recovery and maximize the success of gender-specific knee replacement surgery?
Following your surgeon’s postoperative instructions, participating in physical therapy, maintaining a healthy lifestyle, and attending regular follow-up appointments are crucial for a successful recovery.
Are there any specific dietary guidelines I should follow before or after gender-specific knee replacement surgery?
While there are no strict dietary restrictions, maintaining a balanced diet rich in nutrients can support healing and overall recovery. Your surgeon may provide personalized dietary recommendations based on your individual needs.
How do I manage pain and discomfort during the recovery period after gender-specific knee replacement surgery?
Your surgeon will prescribe pain medications and recommend other pain management strategies such as icing, elevation, and gentle exercises to help alleviate discomfort during the recovery process.
Will I need assistance at home following gender-specific knee replacement surgery?
Depending on your level of mobility and independence, you may require assistance with daily tasks such as cooking, cleaning, and personal care during the initial stages of recovery.
Can complications arise years after undergoing gender-specific knee replacement surgery?
While complications are rare in the long term, issues such as implant wear, loosening, or infection may occur several years after surgery. Regular follow-up appointments with your surgeon can help monitor for any potential complications.
Is gender-specific knee replacement surgery covered by insurance?
In many cases, gender-specific knee replacement surgery is covered by health insurance, although coverage may vary depending on your specific plan and provider. It’s important to check with your insurance company to understand your coverage options and any potential out-of-pocket costs.
How do I find a qualified orthopedic surgeon experienced in performing gender-specific knee replacement surgery?
You can start by asking for recommendations from your primary care physician or researching orthopedic surgeons specializing in knee replacement surgery in your area. Be sure to inquire about their experience, training, and patient outcomes related to gender-specific knee replacement.
Can I undergo gender-specific knee replacement surgery if I have other underlying health conditions?
Your surgeon will evaluate your overall health and medical history to determine if you’re a suitable candidate for surgery. While certain health conditions may increase the risks associated with surgery, they may not necessarily preclude you from undergoing gender-specific knee replacement.
Will I need to make any modifications to my home environment to accommodate my recovery after gender-specific knee replacement surgery?
Depending on your mobility and accessibility needs, you may need to make temporary modifications to your home, such as installing handrails, raised toilet seats, or removing trip hazards, to ensure a safe and comfortable recovery environment.
How can I manage swelling and inflammation in my knee after gender-specific knee replacement surgery?
Your surgeon may recommend techniques such as icing, compression therapy, elevation, and prescribed medications to help reduce swelling and inflammation during the recovery period.
What are the potential signs of complications or issues that I should watch out for after gender-specific knee replacement surgery?
Warning signs such as increased pain, swelling, redness, warmth, or drainage from the surgical site, as well as difficulty bearing weight or sudden changes in mobility, should be promptly reported to your surgeon for further evaluation and management.

