High tibial osteotomy is a surgical procedure used to treat knee osteoarthritis by realigning the knee joint. It shifts weight away from the damaged part of the knee and is often recommended for younger, active individuals who are not ready for a total knee replacement.
How Common It Is and Who Gets It? (Epidemiology)
High tibial osteotomy is less common than knee replacement and is most often performed in younger patients with knee malalignment such as bow legs or knock knees. It is also used in people who have early arthritis affecting only one side of the knee.
Why It Happens – Causes (Etiology and Pathophysiology)
Osteoarthritis causes cartilage, ligaments, meniscus, and other knee structures to wear down. Malalignment such as bow legs or knock knees places more pressure on one side of the knee, speeding up this wear. Injuries can also lead to early arthritis.
- Cartilage: Articular cartilage is a glistening white smooth tissue covering the ends of bones where it articulates with other bone and form a joint. It is toughened yet flexible enough to cushion the gliding of the bones forming a joint thereby reducing friction and acting as a shock absorber.
- Meniscus: They are pads of tissue between the joint dampening the impact. Both the meniscus and cartilage have a very limited blood supply therefore limiting any healing if subjected to damage.
- Ligament: These are tough tissues connecting one bone to another. Ligaments prevent slipping one bone over the other, maintaining stability.
- Synovium: A thin tissue lines the inside of the joint secreting a watery thin, sticky, clear lubrication called synovial fluid. Just like machine oil it helps in smooth movement of the joint.
- Bones and Muscles: End of the thigh bone(femur) and upper part of the shin bone(tibia) with muscles attached to them help to bend or straighten the knee joint. A proper alignment between both is necessary to perform the movements.
Alignment of the Knee
In a normal individual the thigh bone and shin bone are aligned so the weight is transmitted equally among the inner and the outer side of the joint. Any malalignment or mismatch leads to excessive weight being placed on one side of the knee. With repetitive loading parts of the cartilage and meniscus get torn on the side placed under undue force. Bow legs or knock knees are examples of malalignment.
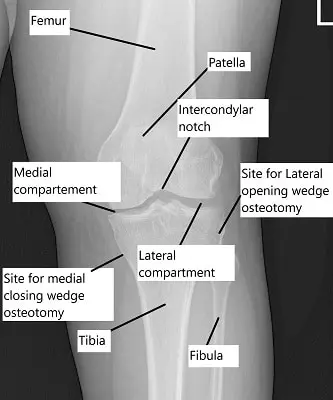
X-ray showing the knee joint
Osteoarthritis
With growing age the tissues forming the knee joint, including the bones, articular cartilage, tendons, ligaments, meniscus and muscles degenerate. The changes culminate into tears of the meniscus and cartilage leading to loss of smooth gliding of the joint. The joint(especially the synovium) becomes inflamed.
Risk factors and causes: Degenerative OA also called wear and tear arthritis, it is common in middle aged to elderly individuals. Age and obesity are common risk factors but a malaligned knee such as knock knees or bow legs can lead to early osteoarthritis. Injuries to the structures forming the knee joint lead to early OA.
How the Body Part Normally Works? (Relevant Anatomy)
The knee is a hinge joint formed by the thigh bone, shin bone, and kneecap. Cartilage cushions joint movement, the meniscus absorbs shock, ligaments stabilize the knee, the synovium lubricates the joint, and muscles support bending and straightening. Proper alignment allows forces to be shared evenly across the joint.
What You Might Feel – Symptoms (Clinical Presentation)
- Grinding/popping/clicking sensation in the knee.
- Inability to fully bend or straighten the knee.
- Knee Pain, especially with activity.
- Stiffness after periods of inactivity
- Swelling around the joint.
How Doctors Find the Problem? (Diagnosis and Imaging)
Medical History: The doctor will begin by asking about your symptoms, including the location and severity of pain, stiffness, swelling, and any limitations in movement. They’ll also inquire about your medical history, including any previous injuries or conditions that may contribute to joint problems.
Physical Examination: During the physical exam, the doctor will inspect and palpate the affected joints for tenderness, swelling, warmth, and range of motion. They may also assess your gait and posture to look for any signs of joint dysfunction.
Imaging Tests: Imaging tests can help confirm the diagnosis and assess the extent of joint damage. Common imaging modalities include:
X-rays: X-rays can reveal joint damage, such as loss of cartilage, bone spurs, and joint deformities characteristic of OA.
Magnetic Resonance Imaging (MRI): MRI scans provide detailed images of soft tissues like cartilage, ligaments, and tendons. They can help detect early signs of OA and assess the severity of joint damage.
Computed Tomography (CT) Scan: CT scans may be used to provide more detailed images of bone structures and detect bone abnormalities in cases where standard X-rays are inconclusive.
Laboratory Tests: While there’s no specific blood test for diagnosing OA, blood tests may be ordered to rule out other conditions that can cause joint pain and inflammation, such as rheumatoid arthritis. Blood tests can also help assess overall health and check for markers of inflammation.
Joint Aspiration (Arthrocentesis): In some cases, joint aspiration may be performed to analyze the synovial fluid (fluid within the joint) for signs of inflammation, infection, or crystals (as in gout).
Diagnostic Criteria: The American College of Rheumatology (ACR) provides diagnostic criteria for OA, which include a combination of symptoms, physical examination findings, and imaging results. However, it’s important to note that these criteria are primarily used for research purposes and may not always align with clinical practice.
Classification
High tibial osteotomy may be classified into:
Lateral closing wedge osteotomy, where a wedge of bone is removed.
Medial opening wedge osteotomy, where the bone is opened and supported with graft.
Both methods rely on plates and screws or casts for fixation.
Other Problems That Can Feel Similar (Differential Diagnosis)
Symptoms may also come from ligament injuries, meniscus tears, patellofemoral arthritis, or advanced arthritis affecting multiple parts of the knee.
Treatment Options
Non-Surgical Care
Options include anti-inflammatory medications, physical therapy, weight management, bracing, and injections such as corticosteroids or hyaluronic acid. Some patients may not respond well to nonsurgical treatments if arthritis is advanced.
Surgical Care
High tibial osteotomy cuts and realigns the shin bone to shift weight off the damaged side of the knee. It is considered when only one side of the knee is affected, knee motion is preserved, ligaments are stable, and the patient is typically younger than sixty.
Procedure
Osteotomy in Osteoarthritis
It is a surgical procedure literally meaning cutting of bone. When performed near the upper end of the shin bone either on outer side or inner side is known as high tibial(shin bone) osteotomy.
Goals & Principles: Two compartments are mainly affected in OA of the knee joint, the outer or the inner compartment. In a malaligned knee the body weight force is transferred mainly through one compartment leading to excessive wear and tear. So the goal of HTO is to reshape and relieve the pressure of the damaged side.
Ideal candidates:
- Patients younger than 60 years of age.
- Knee joint movements are not restricted i.e can fully bend or straighten the knee.
- One compartment involvement either the inner or outer side.
- Normal knee ligaments which balance the knee.
- Patient who are not obese or having inflammatory diseases like rheumatoid arthritis.
Types and procedure:
- Lateral Closing Wedge: A predetermined wedge of bone is removed from the upper part of the shin bone to correct the alignment. Different methods such as casts or plate and screws may be used to fix the cut ends together.
- Medial Opening Wedge: Here a cut is made on the inner side of the upper shin bone. The cut is opened up and usually filled with a bone graft. Again it may be fixed with a plate and screws.
Post Surgery: Weight bearing is delayed and patient walks on crutches as long as 12 weeks with regular physical therapy.
Advantages: The anatomy of the knee is maintained. With corrected alignment the degenerative process of osteoarthritis halts or slows down. Younger age group of patients with limited single compartment involvement are to benefit more.
Disadvantages: Various complications may arise post surgery
- Full recovery is usually prolonged to many weeks or months.
- Pain relief at times is not predictable and many patients complain of residual pain.
- Postoperative complications such as infection and stiffness may occur.
- A potential damage to the nerves which make the foot work or the blood vessels supplying blood to the leg.
- Majority of patients opting for HTO end up having a total knee replacement in the coming years. Although the surgical technique for Total Knee Replacement becomes much more challenging after HTO.
- HTO requires cutting of the bone. The cutting site sometimes fail to heal and a second surgery is then needed to heal it. Moreover, when a bone graft from a person’s own body is used to fill in the gap of cutting, there could be potential complications of bone graft site.
- There could be problems of leg lengthening or leg shortening after the surgery.
- In case there is evidence of kneecap arthritis(patellofemoral arthritis) HTO cannot be performed in such cases.
Total Knee replacement
Knee replacement surgeries have revolutionized the treatment of osteoarthritis. The joint ends are replaced or resurfaced with metal and plastic parts. The prosthetic parts recreate the joint movements.
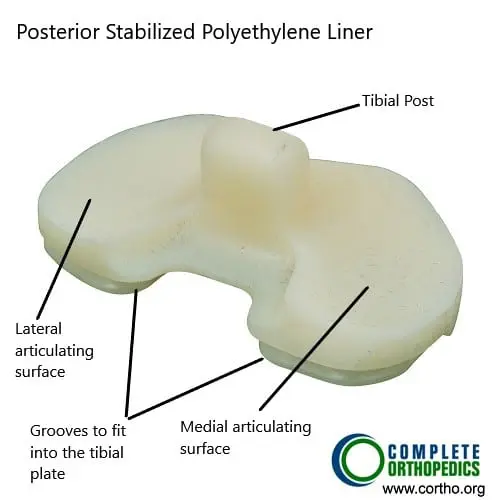
Polyethylene Insert (Posterior Stabilized)
The tibial post on the polyethylene insert allows femoral rollback during bending of the knee. The post along with the femoral cam reduplicates the function of the posterior cruciate ligament.

Tibial component (undersurface)
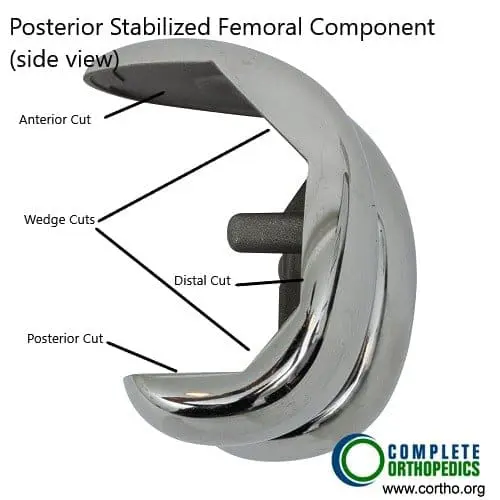
Femoral Component (side view)
The prosthetic parts include metallic (cobalt chromium) femoral and tibial components and a highly cross linked polyethylene bearing insert. The femoral component fits in the lower end of the thigh bone on the cuts made during surgery. The tibial components sits on top the upper end of the shin bone. Both the metal components are fixed to the respective bones using bone cement.
Excellent stability is achieved as the parts reduplicate the function of ligaments and meniscus. Alignment of the joint line is created as it was before the disease process.
For Total Knee Replacement procedure and cost information, please click here.
Advantages
- Can be performed even in individuals more than 60 years of age.
- Early rehabilitation as most patients start to bear weight the very next day
- Excellent survival of the implant even in second decade of surgery.
- Pain relief is complete and the patient satisfaction rates are very high.
- Most patients carry on their daily activities without feeling any difference from the native knee.
- Revisions are being carried out without any complications.
A primary total knee arthroplasty is emerging as a better option than high tibial osteotomy even in stages of early Osteoarthritis. The success rate of surgery and patient satisfaction rates are unparalleled.
Recovery and What to Expect After Treatment
Weight bearing is delayed after surgery, and patients may use crutches for up to twelve weeks. Physical therapy is required to restore movement and strength. Full recovery may take several weeks or months. Some patients may still experience pain after surgery.
Possible Risks or Side Effects (Complications)
Complications include infection, stiffness, nerve injury, blood vessel injury, failure of the bone to heal, leg length changes, and the possibility that pain relief may be unpredictable. In some cases, a second surgery may be needed to heal the bone. High tibial osteotomy cannot be done if there is patellofemoral arthritis.
Long-Term Outlook (Prognosis)
Corrected alignment can slow or halt osteoarthritis progression. However, many patients eventually need a total knee replacement. Knee replacement after high tibial osteotomy is more challenging for surgeons.
Out-of-Pocket Cost
Medicare
CPT Code 27457 – High Tibial Osteotomy: $226.71
Medicare usually covers most of the approved charge for this alignment procedure, leaving the patient with the standard twenty percent portion. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield typically remove that remaining share. These supplemental policies work alongside Medicare and are meant to fill the co-insurance gap, which often results in little or no remaining cost when the procedure is Medicare-approved.
Secondary insurance, including employer-based coverage, TRICARE, or the Veterans Health Administration, becomes the next payer after Medicare. Once any deductible is met — usually between $100 and $300 — the secondary plan may pay whatever balance remains. This often reduces or eliminates the remaining cost tied to the osteotomy.
Workers’ Compensation
If your knee condition requiring a high tibial osteotomy is linked to a work-related injury, Workers’ Compensation pays the full cost of the surgery and all related care. This leaves you with no out-of-pocket expense.
No-Fault Insurance
If the need for the osteotomy stems from a motor vehicle accident, No-Fault Insurance covers the entire procedure. Your only possible cost may be a small deductible depending on your specific policy.
Example
A patient needed a high tibial osteotomy to correct knee malalignment. Under Medicare, the estimated out-of-pocket cost was $226.71. Because the patient also carried secondary insurance, the remaining portion was covered fully, leaving the patient with no out-of-pocket expense.
Frequently Asked Questions (FAQ)
Q. Is high tibial osteotomy only for young patients?
A. It is most beneficial for younger individuals with arthritis in one compartment of the knee.
Q. How long is recovery?
A. Weight bearing is restricted for weeks, and full recovery may take months.
Q. Will I need knee replacement later?
A. Many patients eventually need total knee replacement.
Q. Can this fix bow legs or knock knees?
A. Yes, high tibial osteotomy corrects malalignment that contributes to arthritis.
Q. What if the bone does not heal?
A. A second surgery may be required if the bone fails to unite.
Summary and Takeaway
High tibial osteotomy realigns the knee to relieve pressure on the arthritic side. It is helpful for younger patients with arthritis in one compartment. Recovery takes time, and complications are possible. Many patients eventually need knee replacement, but the procedure can delay that need and improve function.
Clinical Insight and Recent Findings
A recent study comparing high tibial osteotomy performed with and without a tourniquet found that although tourniquet use reduced intraoperative bleeding and shortened operative time, it did not decrease total blood loss and was linked to higher postoperative pain, more swelling, elevated inflammatory markers, and slower early knee motion.
These findings complement your overview of high tibial osteotomy, reinforcing that the procedure’s success depends heavily on early rehabilitation, careful alignment correction, and minimizing postoperative inflammation.
By avoiding a tourniquet when modern bleeding-control methods such as tranexamic acid are used, surgeons may support faster recovery and better early function in the younger, active patients who typically undergo this joint-preserving surgery. (“Study of tourniquet use in high tibial osteotomy – See PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons specializing in knee surgery perform high tibial osteotomy. Physical therapists assist in recovery.
When to See a Specialist?
A specialist should be consulted when knee pain, swelling, stiffness, or malalignment continues despite nonsurgical treatments.
When to Go to the Emergency Room?
Emergency care is needed for high fever, severe swelling, uncontrollable pain, or signs of infection after surgery.
What Recovery Really Looks Like?
Recovery includes limited weight bearing, physical therapy, and gradual return to activity. Patients must follow instructions to help the bone heal correctly.
What Happens If You Ignore It?
Ignoring malalignment or arthritis may lead to worsening pain, faster joint damage, and reduced mobility.
How to Prevent It?
Maintaining healthy weight, treating injuries early, and protecting knee alignment may help slow arthritis progression.
Nutrition and Bone or Joint Health
Healthy meals support bone healing and overall joint recovery. Adequate protein and hydration assist in recovery after surgery.
Activity and Lifestyle Modifications
Activity increases slowly after surgery. Patients must avoid heavy weight-bearing early on. Physical therapy guides safe return to walking and exercise.
¿Tienes más preguntas?
How long does the recovery process typically take after a high tibial osteotomy (HTO)?
The recovery process after HTO can vary depending on the individual patient and the extent of the surgery. Generally, patients can expect to be back to light activities within a few weeks to a couple of months, but full recovery may take several months to a year.
What are the main factors that determine if someone is a good candidate for high tibial osteotomy (HTO)?
The main factors that determine candidacy for HTO include the severity and location of the osteoarthritis, the patient’s age, activity level, and overall health. Ideal candidates are typically younger, active individuals with early to mid-stage osteoarthritis localized to one side of the knee joint.
Can high tibial osteotomy (HTO) be performed on both knees at the same time?
While it is technically possible to perform HTO on both knees simultaneously, it’s not commonly done due to the increased risks and challenges associated with recovery and rehabilitation. It’s generally recommended to stage the surgeries, addressing one knee at a time to optimize outcomes and minimize complications.
How long do the results of a high tibial osteotomy (HTO) typically last?
The results of HTO can be long-lasting, especially when combined with appropriate lifestyle modifications and physical therapy. However, the progression of osteoarthritis may continue over time, eventually necessitating further interventions such as total knee replacement (TKR).
What types of exercises are typically recommended during the recovery period after high tibial osteotomy (HTO)?
During the recovery period after HTO, gentle range of motion exercises, strengthening exercises for the quadriceps and hamstrings, and low-impact activities like walking or stationary cycling are usually recommended. Physical therapy will provide specific exercises tailored to individual needs and stage of recovery.
Are there any dietary or nutritional recommendations that can help support recovery after high tibial osteotomy (HTO)?
While there are no specific dietary guidelines for recovery after HTO, maintaining a balanced diet rich in nutrients like protein, vitamins, and minerals can support healing and overall health. Adequate hydration is also important for tissue repair and recovery.
Are there any dietary or nutritional recommendations that can help support recovery after high tibial osteotomy (HTO)?
While there are no specific dietary guidelines for recovery after HTO, maintaining a balanced diet rich in nutrients like protein, vitamins, and minerals can support healing and overall health. Adequate hydration is also important for tissue repair and recovery.
What are the potential complications associated with high tibial osteotomy (HTO)?
Complications of HTO can include infection, blood clots, nerve or blood vessel damage, failure of bone healing (nonunion), and continued pain or stiffness in the knee joint. However, with proper surgical technique and postoperative care, these risks can be minimized.
How soon after high tibial osteotomy (HTO) can I expect to see improvements in my knee pain and function?
While some patients experience immediate relief of symptoms after HTO, it may take several weeks to months for full benefits to be realized as the knee joint heals and rehabilitates. Consistent adherence to postoperative instructions and physical therapy can help optimize outcomes.
Can high tibial osteotomy (HTO) be repeated if the initial surgery does not provide sufficient relief?
In some cases, a revision HTO may be considered if the initial surgery does not achieve the desired outcomes. However, the success of revision HTO depends on various factors, including the cause of failure and the condition of the knee joint.
Will I need to wear a brace or use assistive devices after high tibial osteotomy (HTO)?
A brace or assistive devices such as crutches or a walker may be recommended temporarily after HTO to support the knee joint and aid in walking during the early stages of recovery. Your surgeon will provide guidance on when and how to use these devices.
How soon after high tibial osteotomy (HTO) can I return to work or normal activities?
The timing of return to work or normal activities will depend on the type of work or activities you engage in, as well as your rate of recovery. Most patients can expect to return to sedentary or light-duty work within a few weeks to a couple of months after HTO, with gradual progression to more strenuous activities over time.
Are there any alternative treatments to high tibial osteotomy (HTO) for knee osteoarthritis?
Yes, alternative treatments for knee osteoarthritis include conservative measures such as medications, injections, physical therapy, and lifestyle modifications. Additionally, other surgical options like arthroscopic procedures or total knee replacement (TKR) may be considered depending on individual circumstances.
How long do the effects of high tibial osteotomy (HTO) typically last before further intervention is needed?
The effects of HTO can vary from patient to patient, but in many cases, the benefits can last for several years to decades before further intervention such as total knee replacement (TKR) becomes necessary. However, ongoing monitoring and follow-up with your orthopedic surgeon are important to assess the progression of osteoarthritis and determine if additional treatment is needed.
What are the differences between high tibial osteotomy (HTO) and total knee replacement (TKR)?
High tibial osteotomy (HTO) is a joint-preserving surgery that realigns the knee joint to redistribute weight and reduce pain in cases of localized osteoarthritis. Total knee replacement (TKR), on the other hand, involves removing damaged joint surfaces and replacing them with artificial components to restore function and alleviate pain in more advanced cases of osteoarthritis.
How does high tibial osteotomy (HTO) compare to other surgical treatments for knee osteoarthritis, such as partial knee replacement?
High tibial osteotomy (HTO) and partial knee replacement are both surgical options for treating knee osteoarthritis, but they differ in their approach and indications. HTO is typically recommended for younger, active patients with localized osteoarthritis, while partial knee replacement may be considered for select patients with damage limited to one compartment of the knee joint.
Will I be able to participate in sports or high-impact activities after high tibial osteotomy (HTO)?
While many patients are able to return to sports and high-impact activities after HTO, it’s important to discuss your specific goals and expectations with your surgeon. Your ability to participate in certain activities will depend on factors such as the type of sport, the condition of your knee joint, and the success of the surgery and rehabilitation.
Can high tibial osteotomy (HTO) be performed arthroscopically?
Yes, high tibial osteotomy (HTO) can be performed using arthroscopic techniques in some cases. Arthroscopic HTO may offer advantages such as smaller incisions, less tissue trauma, and potentially faster recovery compared to traditional open surgery. However, not all patients are candidates for arthroscopic HTO, and the decision will depend on various factors including the surgeon’s expertise and the specific characteristics of the patient’s condition.
What are the long-term risks of high tibial osteotomy (HTO), and how can they be minimized?
Long-term risks of HTO include progression of osteoarthritis, development of arthritis in other parts of the knee joint, and potential need for additional surgeries such as total knee replacement (TKR). These risks can

