Cervical corpectomy is a surgical procedure designed to relieve severe spinal cord and/or nerve compression in the neck. It involves the removal of one or more vertebral bodies and the associated intervertebral discs, which may be causing pain, numbness, weakness, and other neurological symptoms. This procedure is often recommended when conservative treatments fail to provide relief and when conditions such as degenerative disc disease, vertebral fractures, or tumors cause significant compression of the spinal cord.
How Common It Is and Who Gets It? (Epidemiology)
Cervical corpectomy is typically performed in patients with severe cervical spinal stenosis, cervical spondylosis, or fractures of the cervical vertebrae. It is also used in cases of tumors compressing the spinal cord. The surgery is usually considered after conservative treatments have been exhausted, and it is often necessary when there is significant weakness, sensory loss, or loss of bowel or bladder control.
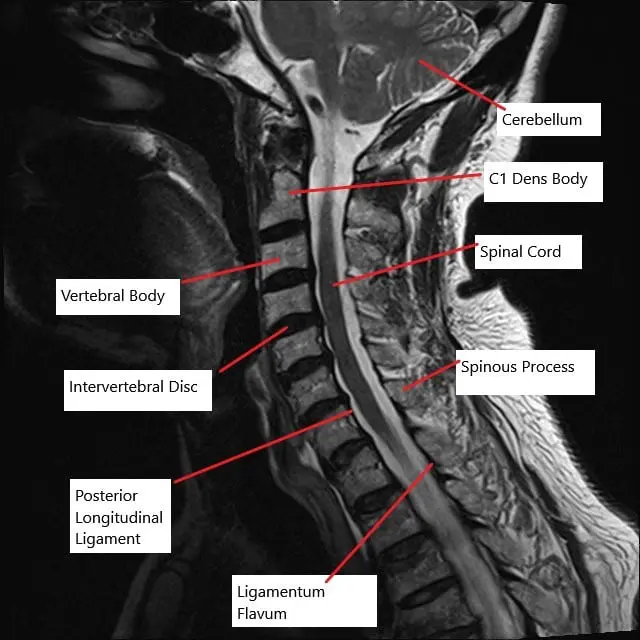
MRI of the cervical spine in the sagittal section showing multiple bulging intervertebral discs.
Why It Happens – Causes (Etiology and Pathophysiology)
The primary cause of the need for cervical corpectomy is the compression of the spinal cord or nerve roots due to conditions such as degenerative disc disease, bone spurs (osteophytes), or trauma. In cervical spinal stenosis, the space around the spinal cord narrows, putting pressure on the cord or nerves, leading to pain, weakness, or loss of function. Tumors or fractures may also cause compression, further necessitating surgical intervention.
How the Body Part Normally Works? (Relevant Anatomy)
The cervical spine consists of seven vertebrae that are separated by intervertebral discs. These discs act as shock absorbers, allowing for movement while also protecting the spinal cord, which runs through the spinal canal formed by the vertebrae. The spinal cord gives off nerves at each vertebral level, which control various body functions. When the vertebrae or discs degenerate, the spinal canal can narrow, compressing the spinal cord or nerves and leading to various neurological symptoms.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of cervical spine compression include neck pain, numbness, tingling, or weakness in the arms, shoulders, and hands. In severe cases, patients may experience difficulty walking, loss of balance, and bowel or bladder incontinence. These symptoms typically worsen over time if untreated and can severely affect daily functioning.
How Doctors Find the Problem? (Diagnosis and Imaging)
Cervical spine conditions are diagnosed through a combination of physical examination and imaging studies. X-rays, MRI, and CT scans help identify the extent of compression in the spinal cord and nerves. In some cases, additional tests such as electromyography (EMG) or nerve conduction studies may be used to evaluate the function of the nerves.
Classification
Cervical corpectomy is classified based on the surgical approach and the number of levels treated:
- Anterior Cervical Corpectomy and Fusion (ACCF): This approach involves accessing the spine from the front of the neck, removing the vertebrae and intervertebral discs, and stabilizing the spine with a bone graft or implant and a plate and screws.
- Posterior Total Laminectomy: This involves accessing the spine from the back, removing the lamina, and decompressing the spinal cord without fusion.
Anterior Cervical Corpectomy and Fusion (ACCF):
-
- Anterior Approach: The surgeon accesses the spine from the front of the neck.
- Fusion: Bone grafts and plates are used to stabilize the spine after the vertebra is removed.
- Advantages: Less post-operative pain and quicker recovery times.
- Considerations: Suitable for multi-level decompressions but involves delicate dissection around vital structures like the esophagus and carotid arteries.
Posterior Total Laminectomy:
-
- Posterior Approach: The spine is accessed from the back.
- Laminectomy: Removal of the lamina (the back part of the vertebra) to relieve pressure.
- Advantages: Provides a broad decompression area.
- Considerations: Larger incisions and more post-operative discomfort compared to anterior approaches.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions that can cause similar symptoms include cervical herniated discs, cervical spondylosis, thoracic outlet syndrome, and other forms of spinal stenosis. Accurate diagnosis is essential to ensure the correct treatment plan.
Treatment Options
- Non-Surgical Care: Conservative treatments such as physical therapy, anti-inflammatory medications, and epidural steroid injections are often tried before surgery.
- Surgical Care: When conservative treatments fail, cervical corpectomy is an option. This surgery involves removing the affected vertebra and disc, decompressing the spinal cord or nerve roots, and stabilizing the spine with bone grafts or implants.
Recovery and What to Expect After Treatment
After cervical corpectomy, patients typically stay in the hospital for a few days for monitoring and pain management. Physical therapy is often recommended to improve strength and mobility. Patients are generally advised to avoid heavy lifting and strenuous activities for several weeks or months while the spine heals. Full recovery can take several months, with the fusion process continuing over the course of 6 to 12 months.
Possible Risks or Side Effects (Complications)
Potential risks of cervical corpectomy include:
- Infection: As with any surgery, there is a risk of infection.
- Nerve Damage: Damage to the spinal cord or nerves can occur during the procedure.
- Nonunion: The bone graft may fail to fuse properly, requiring additional surgery.
- Implant Issues: The hardware used to stabilize the spine may shift or break.
- Anesthesia Reactions: Some patients may have adverse reactions to anesthesia.
Long-Term Outlook (Prognosis)
Patients undergoing cervical corpectomy typically experience significant relief from pain and neurological symptoms, especially if the surgery is performed before severe damage occurs. The recovery process can take several months, but many patients are able to return to normal activities once the spine has stabilized.
Out-of-Pocket Cost
Medicare
CPT Code 63081 – Cervical Corpectomy: $433.45
Under Medicare, 80% of the approved cost for this procedure is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved cervical spine surgeries like corpectomy. These supplemental plans work directly with Medicare to ensure full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer after Medicare has processed your claim. Once your deductible is satisfied, the secondary plan may cover any remaining balance, including coinsurance or any uncovered charges. Most secondary plans have a modest deductible, typically ranging from $100 to $300, depending on the specific policy and whether the surgery is performed in-network.
Workers’ Compensation
If your cervical spine condition requiring corpectomy is work-related, Workers’ Compensation will cover the full cost of the procedure, including surgery, hospitalization, and rehabilitation. You will not have any out-of-pocket costs under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your cervical spine injury requiring corpectomy resulted from a motor vehicle accident, No-Fault Insurance will pay for all related medical and surgical costs. The only potential out-of-pocket expense may be a small deductible depending on your specific policy terms.
Example
David, a 65-year-old patient with cervical myelopathy and spinal instability, required cervical corpectomy (CPT 63081). His estimated Medicare out-of-pocket cost was $433.45. Since he had supplemental insurance through Blue Cross Blue Shield, the remaining 20% not covered by Medicare was fully paid, leaving him with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. What are the benefits of cervical corpectomy over other procedures?
A. Cervical corpectomy effectively decompresses the spinal cord and nerve roots while also stabilizing the spine. It is ideal for severe cases of cervical stenosis or spinal fractures where other treatments have failed.
Q. How long does recovery take after cervical corpectomy?
A. Recovery typically takes several months. Most patients experience relief from symptoms within a few weeks, but full recovery, including fusion of the vertebrae, may take 6 to 12 months.
Summary and Takeaway
Cervical corpectomy is a critical surgery for patients suffering from severe spinal cord compression caused by conditions like degenerative disc disease, spinal stenosis, or fractures. The procedure effectively relieves symptoms, restores stability to the spine, and improves quality of life. Though there are risks, the overall prognosis for most patients is positive, especially with timely intervention and adherence to post-surgical care.
Clinical Insight & Recent Findings
A recent study explored the impact of forearm bone mineral density (BMD) on the risk of titanium mesh cage (TMC) subsidence following anterior cervical corpectomy and fusion (ACCF). The study found that lower forearm BMD significantly increased the risk of TMC subsidence, with each 0.1 g/cm² decrease in forearm BMD correlating with a 6.6% higher risk.
Additionally, the study identified that lower vertebral body Hounsfield unit (HU) values also played a role in predicting subsidence risk. The study suggests that forearm BMD and lower vertebral HU values are effective predictors for titanium mesh subsidence, highlighting the importance of evaluating bone density in patients undergoing ACCF to reduce postoperative complications.
(“Study of forearm BMD and titanium mesh subsidence – See PubMed.”)
Who Performs This Treatment? (Specialists and Team Involved)
Cervical corpectomy is typically performed by orthopedic surgeons or neurosurgeons specializing in spinal surgery. The procedure may be supported by anesthesiologists, nurses, and physical therapists to ensure comprehensive care throughout the surgical and recovery process.
When to See a Specialist?
If you experience persistent neck pain, weakness, or neurological symptoms such as numbness or loss of coordination that do not improve with conservative treatments, it may be time to consult a spine specialist.
When to Go to the Emergency Room?
Seek immediate medical attention if you experience sudden weakness, difficulty breathing, or loss of bowel or bladder control, as these can be signs of a spinal emergency.
What Recovery Really Looks Like?
Recovery from cervical corpectomy involves a gradual improvement in symptoms, with many patients returning to normal activities after a few months. Physical therapy plays a key role in strengthening the neck and spine.
What Happens If You Ignore It?
Ignoring severe cervical spine conditions can lead to permanent nerve damage, loss of motor function, and further disability. Early surgical intervention can help prevent further deterioration and improve overall outcomes.
How to Prevent It?
Maintaining good posture, avoiding excessive strain on the neck, and performing neck-strengthening exercises can help prevent cervical spine issues. Regular check-ups with a healthcare provider can also help identify potential issues early.
Nutrition and Bone or Joint Health
Adequate intake of calcium and vitamin D is essential for bone health, which supports the cervical spine. A diet rich in these nutrients helps prevent degenerative changes and promotes healing after surgery.
Activity and Lifestyle Modifications
Post-surgery, patients should focus on gentle exercises that improve neck mobility and strength. It’s important to avoid heavy lifting and high-impact activities during the recovery phase.
¿Tienes más preguntas?
What are the primary conditions that necessitate a corpectomy?
Corpectomy is primarily indicated for conditions such as cervical spondylotic myelopathy, spinal cord compression due to trauma, severe degenerative disc disease, and tumors affecting the vertebral bodies.
How is the decision made between an anterior and a posterior approach for corpectomy?
The decision depends on the location and extent of the spinal cord compression, the patient’s anatomy, and the presence of previous surgeries or scar tissue. Anterior approaches are preferred for single or multilevel decompressions at the front of the spine, while posterior approaches are used for more extensive decompressions.
What preoperative tests are required before undergoing corpectomy?
Preoperative tests typically include MRI and CT scans to assess the spine’s condition, blood tests to evaluate general health, and sometimes electrodiagnostic studies to assess nerve function.
How long does the corpectomy surgery take?
The duration of the surgery can vary but typically ranges from 3 to 5 hours, depending on the complexity and number of levels involved.
Are there non-surgical alternatives to corpectomy?
Non-surgical treatments include physical therapy, pain management, and lifestyle modifications. However, these are usually insufficient for severe cases requiring corpectomy.
What types of anesthesia are used during corpectomy?
General anesthesia is used, ensuring the patient is unconscious and pain-free throughout the procedure.
How is the removed vertebral body replaced during the surgery?
The removed vertebral body is typically replaced with a bone graft or a synthetic cage filled with bone graft material, which is then secured with metal plates and screws.
What are the main risks associated with corpectomy?
Risks include infection, bleeding, nerve damage, non-fusion of the bone graft, and complications related to the hardware used for stabilization.
How do surgeons avoid damaging the spinal cord during corpectomy?
Surgeons use advanced imaging techniques, careful surgical planning, and precise microsurgical tools to minimize the risk of spinal cord damage.
What measures are taken to prevent infection during surgery?
Surgeons follow strict sterilization protocols, administer prophylactic antibiotics, and use sterile techniques to reduce the risk of infection.
What can patients expect immediately after surgery?
Patients can expect to stay in the hospital for a few days for monitoring, pain management, and initial physical therapy.
How is post-operative pain managed?
Pain is managed through medications such as opioids, NSAIDs, and muscle relaxants, alongside other methods like ice therapy and gradual mobilization.
When can patients resume normal activities after corpectomy?
Patients can typically resume light activities within a few weeks, but heavy lifting and strenuous activities should be avoided for several months. The exact timeline depends on individual recovery.
What are the signs of complications that patients should watch for?
Signs of complications include increased pain, redness or swelling at the incision site, fever, numbness, or weakness. Patients should contact their surgeon immediately if they experience any of these symptoms.
Will patients need physical therapy after corpectomy?
Yes, physical therapy is an essential part of recovery to restore strength, flexibility, and function in the neck and back muscles.
Are there any long-term lifestyle changes required after corpectomy?
Patients may need to adopt ergonomic practices, avoid high-impact activities, and maintain a healthy weight to prevent further spinal issues.
How effective is corpectomy in relieving symptoms and improving quality of life?
Studies have shown that corpectomy is highly effective in relieving pain and neurological symptoms, with most patients experiencing significant improvements in quality of life.
What follow-up care is required after corpectomy?
Follow-up care includes regular visits to the surgeon, imaging studies to monitor fusion, and adherence to physical therapy and activity restrictions.
Can corpectomy be performed minimally invasively?
While traditional corpectomy is an open procedure, minimally invasive techniques are being developed but are not yet widely adopted due to their complexity.
How do surgeons handle multiple level compressions during corpectomy?
Surgeons may perform multilevel corpectomies or combine corpectomy with other procedures like discectomy to address multiple compressions.
What role does patient age play in corpectomy outcomes?
Age can affect recovery, with younger patients generally healing faster. However, older patients can still achieve good outcomes with proper post-operative care.
Are there any dietary recommendations post-surgery?
A balanced diet rich in protein, calcium, and vitamin D can support bone healing. Patients should also stay hydrated and avoid smoking, as it impairs bone healing.

