At Complete Orthopedics, we specialize in diagnosing and treating neck and spine conditions using advanced, patient-centered care. Our board-certified surgeons use both non-surgical and surgical approaches to relieve pain, restore movement, and protect long-term spinal health.
Our clinics are conveniently located across New York City and Long Island, connected with six leading hospitals and equipped with the latest surgical and diagnostic technology. Scheduling an appointment with one of our spine specialists is easy—online or by phone.
How Common It Is and Who Gets It? (Epidemiology)
Cervical Spondylotic Myelopathy (CSM) is one of the most common causes of spinal cord compression in adults over age 50. It results from age-related wear and tear of the neck bones, joints, and discs. Men tend to be affected slightly more often than women. People born with a naturally narrow spinal canal (a condition called congenital stenosis) are at higher risk of developing symptoms earlier in life.
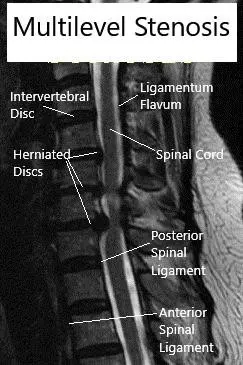
MRI (Sagittal) Cervical spine with multilevel stenosis
Why It Happens – Causes (Etiology and Pathophysiology)
CSM occurs when the spinal cord in the neck becomes squeezed by age-related changes. Over time, the discs that act as cushions between the neck bones lose height and flexibility. As they wear down, the surrounding joints and ligaments can thicken or stiffen, narrowing the spinal canal.
This narrowing puts pressure on the spinal cord, which can interfere with nerve signals traveling between the brain and body. Reduced blood flow to the cord may also contribute to the symptoms. Even minor trauma or sudden movement can trigger worsening of the condition in someone with existing spinal narrowing.
How the Body Part Normally Works? (Relevant Anatomy)
The cervical spine consists of seven small bones (C1–C7) stacked on top of one another. These bones are separated by soft discs that cushion the neck and allow smooth movement. The spinal cord passes through a central canal in these bones, carrying nerve signals to and from the arms, legs, and the rest of the body.
Strong ligaments, such as the ligamentum flavum, support and stabilize the spine. When these ligaments or surrounding structures thicken due to age-related changes, they can press against the spinal cord and cause myelopathy—meaning damage to the spinal cord itself.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of cervical spondylotic myelopathy can vary from mild to severe. Some patients notice only subtle changes, while others develop major weakness or loss of coordination. Common symptoms include:
- Numbness or tingling in the hands, arms, or legs
- Weakness or clumsiness when using the hands
- Trouble walking or balancing
- Electric shock-like sensations down the back or limbs when bending the neck (Lhermitte’s sign)
- Stiffness or tightness in the arms or legs
- Difficulty with fine motor skills such as buttoning a shirt
- In advanced cases, problems with bladder or bowel control
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a detailed medical history and physical examination. Doctors test reflexes, muscle strength, coordination, and walking ability to assess spinal cord function.
Imaging studies confirm the diagnosis and show how much pressure is on the spinal cord:
- X-rays reveal bone alignment and age-related changes.
- MRI is the best test to visualize the spinal cord, discs, and ligaments.
- CT scans provide detailed images of bone structure, especially when MRI is not possible.
- Electromyography (EMG) may help measure how well the nerves and muscles are working.
These studies together determine the severity of compression and guide treatment planning.
Classification
Doctors classify CSM based on severity and the number of spinal levels involved:
- Mild CSM: Subtle symptoms such as hand clumsiness or mild weakness.
- Moderate CSM: Noticeable gait or balance issues, stiffness, and weakness in arms or legs.
- Severe CSM: Significant loss of strength, coordination, and bladder or bowel control.
The number of affected levels (single-level vs. multilevel disease) also influences treatment options.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions that can mimic CSM include:
- Cervical disc herniation pressing on a single nerve root (radiculopathy)
- Multiple sclerosis or other inflammatory nerve disorders
- Vitamin B12 deficiency
- Amyotrophic lateral sclerosis (ALS)
- Spinal cord tumors or infections
Advanced imaging and nerve studies help rule out these possibilities.
Treatment Options
Non-Surgical Care
Patients with mild symptoms or early disease may initially be treated without surgery. Non-surgical care can include:
- Physical therapy: Gentle exercises to strengthen neck and shoulder muscles and improve balance.
- Medications: Anti-inflammatory drugs or pain relievers to reduce stiffness and discomfort.
- Lifestyle adjustments: Avoiding sudden neck movements or heavy lifting.
These treatments focus on symptom relief and slowing progression but do not reverse spinal cord compression.
Surgical Care
Surgery is recommended when symptoms worsen or spinal cord pressure is severe. The goal is to remove the source of compression and stabilize the spine. The approach depends on alignment, number of affected levels, and individual anatomy.
Anterior Cervical Discectomy and Fusion (ACDF):
The surgeon approaches the spine from the front of the neck, removes the damaged disc or bone spurs, and stabilizes the area using a small bone graft and plate.
Posterior Cervical Laminectomy and Fusion:
Through an incision at the back of the neck, the surgeon removes portions of bone (lamina) to decompress the spinal cord and then stabilizes the spine with rods and screws.
Laminoplasty (Non-Fusion Surgery):
In selected cases, the lamina is hinged open to enlarge the spinal canal without fusing the bones, preserving more motion.
Surgery generally prevents further neurological decline and may improve strength, coordination, and pain.
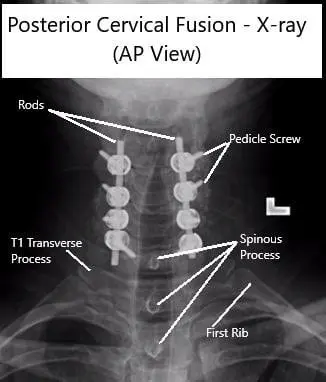
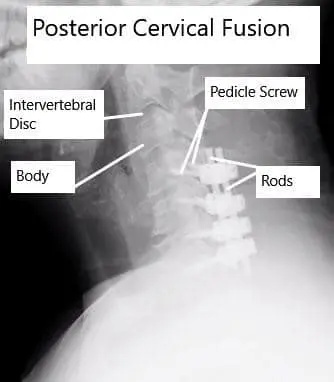
AP and Lateral View X-rays of Posterior Cervical Laminectomy and Fusion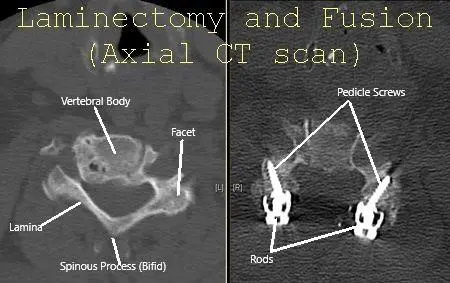
Cervical Spine Axial CT scan showing Laminectomy and fusion.
Recovery and What to Expect After Treatment
Recovery varies depending on the type of surgery and the severity of the condition. Most patients stay in the hospital for a few days. Physical therapy starts soon after surgery to restore movement, balance, and strength.
- Short-term recovery: Patients often notice reduced tingling and improved coordination within weeks.
- Long-term recovery: Nerve healing continues for months and may take up to a year.
- Rehabilitation: A structured program helps rebuild function and confidence in daily activities.
Patients who had mild symptoms before surgery tend to recover faster and more completely than those with long-standing or severe compression.
Possible Risks or Side Effects (Complications)
Like all spinal procedures, surgery for CSM carries potential risks, including:
- Infection or bleeding
- Injury to the spinal cord or nerves
- Difficulty swallowing (temporary after anterior surgery)
- Fusion not healing properly (nonunion)
- Hardware failure requiring revision surgery
- Blood clots, lung issues, or bedsores during recovery
These risks are minimized through careful planning, modern techniques, and close postoperative care.
Long-Term Outlook (Prognosis)
Patients treated early generally experience excellent improvement. Once the spinal cord has been compressed for a long time, some symptoms may persist even after surgery. However, surgery typically stops progression and improves quality of life.
Patients with mild disease can often be managed non-surgically, while those with moderate or severe disease usually benefit most from surgical decompression.
Out-of-Pocket Costs
Medicare
CPT Code 22551 – Anterior Cervical Discectomy and Fusion (ACDF): $417.50
CPT Code 63081 – Corpectomy (Anterior Decompression of Vertebral Body): $433.45
CPT Code 63045 – Posterior Cervical Decompression (Laminectomy): $319.26
CPT Code 22600 – Posterior Cervical Fusion: $322.92
CPT Code 63050 – Cervical Laminoplasty: $362.34
Under Medicare, patients typically pay 20% of the approved amount for these spine procedures after meeting the yearly deductible. Supplemental insurance plans, such as Medigap, AARP, or Blue Cross Blue Shield, usually cover this remaining 20%, effectively reducing or eliminating out-of-pocket costs for Medicare-covered surgeries. These supplemental plans coordinate directly with Medicare to ensure patients face minimal or no financial responsibility for approved treatments.
Secondary insurance plans, including Employer-Based Plans, TRICARE, or Veterans Health Administration (VHA) coverage, serve as secondary payers once Medicare has been billed. After your deductible is met, these secondary policies often pay the remaining coinsurance or balance due. Some plans carry a small deductible, usually between $100 and $300, depending on policy specifics and whether the surgery is performed in-network.
Workers’ Compensation
If your cervical spine condition or injury is related to your job, Workers’ Compensation will cover the full cost of all necessary procedures—whether it involves anterior (ACDF, corpectomy) or posterior (laminectomy, fusion, or laminoplasty) surgery. This includes hospital care, surgeon fees, and rehabilitation, leaving you with no out-of-pocket expenses.
No-Fault Insurance
If your neck injury was caused by a motor vehicle accident, No-Fault Insurance will cover the entire cost of the medically necessary procedures, including decompression, fusion, or laminoplasty. You may only be responsible for a minor deductible based on your specific insurance plan, but most patients have no out-of-pocket costs for approved surgical care.
Example
David, a 59-year-old construction worker, required an anterior cervical discectomy and fusion (ACDF) followed by posterior fusion to stabilize his neck after a traumatic injury. His Medicare out-of-pocket cost for the combined procedures would have been $417.50 and $322.92. Because he had supplemental coverage through AARP Medigap, the 20% not paid by Medicare was fully covered, resulting in no out-of-pocket expenses for his surgeries.
Frequently Asked Questions (FAQ)
Q. Is CSM the same as a pinched nerve?
A. Not exactly. A pinched nerve affects a single nerve root, while CSM involves pressure on the spinal cord itself, often affecting both arms and legs.
Q. Will I recover fully after surgery?
A. Many patients improve significantly, especially if surgery is done early, but recovery varies depending on how long the cord was compressed.
Q. Can CSM get better without surgery?
A. Mild cases may remain stable with therapy and careful monitoring, but most patients with moderate or severe symptoms eventually need surgery.
Q. How long is recovery after surgery?
A. Most people return to light activity within a few weeks and to full activity in several months, depending on the procedure.
Summary and Takeaway
Cervical Spondylotic Myelopathy is a condition where the spinal cord in the neck becomes compressed due to age-related changes. Symptoms can include numbness, weakness, coordination problems, and difficulty walking. Early diagnosis and treatment—whether non-surgical or surgical—are key to preventing permanent nerve damage. With timely care, most patients regain function and live active, independent lives.
Clinical Insight & Recent Findings
A recent study investigated the link between spinal cord compression and high-signal changes seen on MRI in patients with cervical spondylotic myelopathy (CSM).
Using kinematic MRI, researchers observed that spinal cord compression worsens as the neck moves from flexion to extension, and patients showing a high-signal intensity on T2-weighted MRI had significantly greater dynamic compression. The study found that when the ratio of extension to flexion compression exceeded 1.4, the likelihood of developing a high signal—and therefore worse neurological impairment—rose sharply.
These findings emphasize the importance of early recognition of dynamic cervical stenosis and careful surgical planning to relieve compression and prevent progressive cord injury. (Study on dynamic MRI findings in cervical spondylotic myelopathy – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is performed by orthopedic spine surgeons or neurosurgeons with specialized training in spinal disorders. The care team may include neurologists, physical therapists, and rehabilitation specialists to assist in diagnosis, surgery, and recovery.
When to See a Specialist?
You should see a spine specialist if you experience:
- Persistent neck pain
- Numbness or weakness in the hands or legs
- Trouble walking or balancing
- Difficulty with fine hand movements
Early evaluation helps prevent permanent nerve damage.
When to Go to the Emergency Room?
Seek emergency care if you experience:
- Sudden loss of movement or sensation in the arms or legs
- Loss of bladder or bowel control
- Severe neck trauma followed by weakness or paralysis
These may signal spinal cord compression requiring urgent treatment.
What Recovery Really Looks Like?
Recovery after CSM surgery is gradual. Most patients regain independence within weeks but continue improving for months. Some stiffness or mild numbness may persist, especially if the spinal cord was compressed for a long time. Commitment to physical therapy is vital for regaining full strength and flexibility.
What Happens If You Ignore It?
Untreated CSM can lead to progressive nerve damage, resulting in difficulty walking, chronic pain, weakness, or even paralysis. Over time, the condition can permanently affect bladder or bowel control.
How to Prevent It?
While aging changes can’t be stopped, maintaining good spine health can delay or reduce progression:
- Maintain good posture when sitting or standing
- Avoid repetitive neck strain or sudden jerking movements
- Keep neck and shoulder muscles strong through regular exercise
- Quit smoking and maintain a healthy weight
Nutrition and Bone or Joint Health
A balanced diet rich in calcium, vitamin D, and protein helps maintain strong bones and muscles. Staying hydrated and avoiding smoking improves blood circulation to spinal tissues.
Activity and Lifestyle Modifications
After recovery, patients should continue low-impact activities such as walking, swimming, and yoga to maintain flexibility and strength. Ergonomic adjustments at work, proper neck support, and avoiding heavy lifting help prevent recurrence.
¿Tienes más preguntas?
What are the early signs of cervical spondylotic myelopathy?
Early signs of cervical spondylotic myelopathy (CSM) often include neck pain, stiffness, and subtle changes such as tingling or numbness in the arms and hands. Patients may also experience slight balance issues or difficulty with fine motor tasks, such as buttoning a shirt or writing.
How quickly does cervical spondylotic myelopathy progress?
The progression of CSM varies widely among individuals. Some may experience a rapid decline in function, while others may have a slow, insidious onset of symptoms over many years. Regular monitoring and early intervention are key to managing the disease effectively.
Can lifestyle changes help manage cervical spondylotic myelopathy?
Yes, lifestyle changes can play a significant role in managing CSM. Maintaining good posture, using ergonomic tools, avoiding heavy lifting, and engaging in regular low-impact exercises can help alleviate symptoms and potentially slow the progression of the condition.
Are there any non-invasive treatments for cervical spondylotic myelopathy?
Non-invasive treatments for CSM include physical therapy to strengthen neck muscles and improve flexibility, pain management with medications such as NSAIDs or muscle relaxants, and lifestyle modifications like improving posture and using cervical collars to support the neck.
When is surgery necessary for cervical spondylotic myelopathy?
Surgery is typically considered necessary for CSM when symptoms are moderate to severe, when there is significant spinal cord compression visible on imaging studies, or when non-surgical treatments fail to provide adequate relief. Surgery aims to decompress the spinal cord and stabilize the spine.
What are the risks associated with surgery for cervical spondylotic myelopathy?
As with any surgical procedure, there are risks associated with surgery for CSM. These can include infection, bleeding, nerve damage, spinal cord injury, complications from anesthesia, and the potential need for further surgeries. However, for many patients, the benefits of surgery outweigh these risks.
How successful is surgery for cervical spondylotic myelopathy?
Surgery for CSM is generally successful, with many patients experiencing significant relief from symptoms. The extent of recovery can vary depending on the severity and duration of spinal cord compression prior to surgery, as well as the patient’s overall health.
Can cervical spondylotic myelopathy recur after surgery?
While surgery aims to decompress the spinal cord and stabilize the spine, there is always a possibility of recurrence. Factors such as ongoing degenerative changes in the spine or inadequate initial decompression can contribute to the recurrence of symptoms.
What kind of rehabilitation is required after surgery?
Rehabilitation after surgery for CSM typically involves physical therapy to improve neck mobility, strengthen muscles, and enhance overall function. This may include guided exercises, posture correction, and possibly occupational therapy to help with daily activities.
How long does recovery take after surgery for cervical spondylotic myelopathy?
Recovery time after surgery for CSM varies but generally ranges from several weeks to months. Most patients can return to normal activities within 3-6 months, depending on the type and extentof the surgery, the patient’s health, and adherence to rehabilitation protocols. Individual recovery can differ, and some patients might experience a quicker return to normal activities, while others might take longer to fully recover.
What are the potential complications if cervical spondylotic myelopathy is left untreated?
If left untreated, CSM can lead to severe and permanent spinal cord damage, resulting in significant neurological deficits such as chronic pain, pronounced muscle weakness, loss of sensation, and severe difficulty in walking or performing daily activities. In extreme cases, it can lead to paralysis or severe disability.
Are there alternative therapies for managing cervical spondylotic myelopathy?
Yes, alternative therapies such as acupuncture, chiropractic care, and yoga might provide some symptom relief for certain patients. However, these should complement, not replace, conventional medical treatments. It is crucial to discuss any alternative therapies with a healthcare provider to ensure they are safe and appropriate for the condition.
Can cervical spondylotic myelopathy affect other parts of the spine?
While CSM specifically affects the cervical spine, the degenerative processes causing it can also impact other parts of the spine, such as the thoracic or lumbar regions. This can lead to similar conditions, like lumbar spondylosis, which can cause lower back pain and nerve compression.
Is cervical spondylotic myelopathy hereditary?
There can be a genetic predisposition to developing spinal degenerative diseases, including CSM. However, environmental factors, lifestyle choices, and occupational hazards also significantly contribute to the condition’s development.
Can cervical spondylotic myelopathy be prevented?
While aging and genetic factors cannot be controlled, certain measures can help reduce the risk of developing CSM. These include maintaining a healthy weight, avoiding smoking, practicing good posture, using ergonomic furniture and tools, and engaging in regular exercise to strengthen the neck and back muscles.
How does cervical spondylotic myelopathy affect daily life?
CSM can significantly impact daily life by causing pain, stiffness, and neurological deficits. These symptoms can make it difficult to perform routine activities, affect work productivity, and reduce overall quality of life. In severe cases, it can lead to loss of independence and the need for assistance with daily tasks.
What is the difference between cervical spondylosis and cervical spondylotic myelopathy?
Cervical spondylosis refers to the general degenerative changes in the cervical spine, such as disc degeneration, bone spur formation, and ligament thickening. Cervical spondylotic myelopathy occurs when these changes compress the spinal cord, leading to neurological symptoms.
Can physical activity worsen cervical spondylotic myelopathy?
High-impact or strenuous physical activities that strain the neck can worsen CSM symptoms. It is essential to engage in low-impact exercises, such as swimming or walking, and follow medical advice on safe physical activities to avoid exacerbating the condition.
How is cervical spondylotic myelopathy different from a herniated disc?
A herniated disc occurs when the soft inner material of a disc bulges out through a tear in the outer layer, potentially compressing nearby nerves or the spinal cord. CSM involves broader degenerative changes that result in spinal cord compression from multiple sources, such as disc herniation, bone spurs, and ligament thickening.
Can cervical spondylotic myelopathy cause cognitive issues?
While CSM primarily affects motor and sensory functions, severe cases can indirectly impact cognitive function due to chronic pain, discomfort, and decreased quality of life, leading to issues like difficulty concentrating, memory problems, and emotional stress.
What role does age play in the development of cervical spondylotic myelopathy?
Age is a significant factor in developing CSM, as degenerative changes in the spine naturally occur with aging. Individuals over 50 are more likely to experience these changes, leading to an increased risk of spinal cord compression and CSM.
Can cervical spondylotic myelopathy be detected through routine check-ups?
CSM might not be detected during routine check-ups unless specific symptoms are reported. Detailed neurological examinations and imaging studies, such as MRI or CT scans, are necessary to diagnose CSM accurately.
What advancements are being made in the treatment of cervical spondylotic myelopathy?
Advances in CSM treatment include minimally invasive surgical techniques, improved imaging technology for early detection, and research into regenerative therapies aimed at repairing spinal cord damage and halting the progression of degenerative changes.
How does cervical spondylotic myelopathy impact mental health?
Chronic pain and disability from CSM can significantly affect mental health, leading to anxiety, depression, and decreased quality of life. Psychological support, counseling, and sometimes medications are necessary to help manage these mental health issues.
Is it safe to drive with cervical spondylotic myelopathy?
Driving can be challenging for individuals with severe CSM symptoms affecting coordination, strength, and reaction times. It is essential to consult with a healthcare provider to assess driving safety and, if necessary, make adjustments or consider alternatives to ensure safety.

