Juvenile Idiopathic Arthritis (JIA) is a type of arthritis that affects children under the age of 16. It causes inflammation in one or more joints that lasts at least six weeks. The condition can affect any joint in the body—including the spine, particularly the neck (cervical spine). JIA was once called juvenile rheumatoid arthritis, but it is now recognized as a group of conditions with different symptoms and causes. The exact cause remains unknown.
How Common It Is and Who Gets It? (Epidemiology)
JIA is the most common type of arthritis in children, affecting roughly 1 in every 1,000. It can appear at any age in childhood, though it often starts between ages 2 and 12. Girls are more likely to develop it than boys. Genetics and immune system responses are believed to play a role, but environmental factors may also contribute.
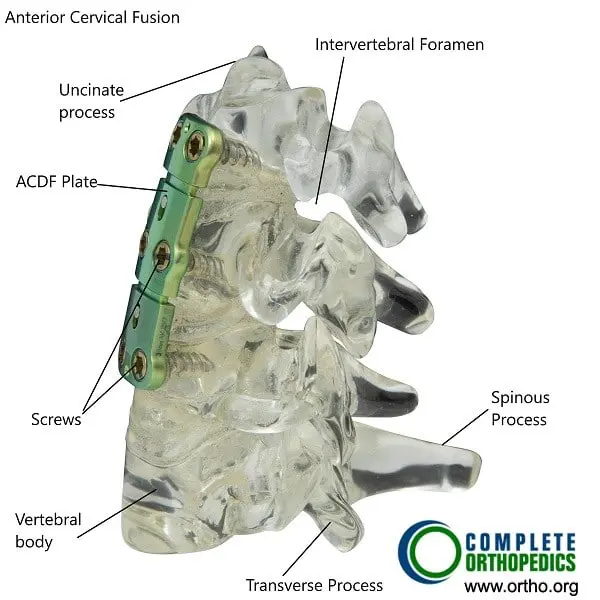
Anterior cervical fusion may be done in severe cases of arthritis and instability of the cervical spine resulting from juvenile idiopathic arthritis.
Why It Happens – Causes (Etiology and Pathophysiology)
The cause of JIA is not fully understood. It occurs when the body’s immune system mistakenly attacks its own tissues, leading to inflammation inside the joints.
Possible contributing factors include:
- Genetic predisposition: Certain genes increase susceptibility.
- Immune dysregulation: The body’s defense system attacks healthy joint tissue.
- Environmental triggers: Infections or stress may trigger the immune response in genetically prone children.
Inflammation damages the joint lining and can lead to swelling, pain, and stiffness. In some cases, the inflammation affects other organs such as the eyes or heart.
How the Body Part Normally Works? (Relevant Anatomy)
A healthy joint contains cartilage and synovial fluid that allow smooth movement without pain. In JIA, inflammation of the synovial membrane—the tissue lining the joint—causes it to thicken and produce excess fluid. This leads to swelling and stiffness. Over time, untreated inflammation can erode cartilage and bone, resulting in joint deformity or instability. The facet joints in the cervical spine are synovial joints and are sometimes affected in children with JIA.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms vary from child to child but commonly include:
- Joint pain and stiffness, especially in the morning or after inactivity
- Swelling and warmth in one or more joints
- Fatigue and low energy
- Reduced mobility or limping
- Fever or rash, especially in systemic JIA (Still’s disease)
- Eye inflammation (uveitis), causing redness, pain, or blurry vision
Neck stiffness or pain can occur when the cervical spine is involved. Severe cases may cause spinal instability that requires surgical stabilization.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis involves a detailed medical history, examination, and several tests to confirm inflammation and rule out other conditions.
Common diagnostic steps include:
- Blood tests: To check for inflammation markers such as ESR and CRP, or antibodies like ANA and rheumatoid factor.
- Physical exam: Evaluates swelling, tenderness, range of motion, and joint function.
- Imaging: X-rays, MRI, or ultrasound may reveal joint damage or cervical spine instability.
- Eye examination: To detect inflammation of the eye early.
Classification
JIA is classified by how many joints are affected and whether other organs are involved:
- Oligoarticular JIA: Affects four or fewer joints, often larger joints like knees or ankles.
- Polyarticular JIA: Involves five or more joints, often smaller ones such as hands and wrists.
- Systemic JIA (Still’s disease): Includes inflammation in organs such as the heart or liver and is associated with fever and rash.
- Enthesitis-related JIA: Affects where tendons and ligaments attach to bones, often involving the spine and hips.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions that may mimic JIA include:
- Rheumatic fever
- Infections such as Lyme disease
- Lupus (systemic lupus erythematosus)
- Bone or joint infections (osteomyelitis)
- Leukemia (in rare cases)
Proper testing helps distinguish JIA from these conditions.
Treatment Options
Non-Surgical Care
The goal of treatment is to control inflammation, relieve pain, prevent joint damage, and maintain mobility.
- Medications:
- NSAIDs (e.g., ibuprofen): Reduce pain and inflammation.
- DMARDs (e.g., methotrexate, hydroxychloroquine): Slow disease progression.
- Biologic agents (e.g., etanercept, adalimumab): Target specific parts of the immune system.
- Corticosteroids: Used short-term for severe inflammation.
- Physical therapy: Maintains flexibility, strength, and range of motion.
- Occupational therapy: Helps with daily activities and joint protection techniques.
- Regular eye exams: Detect eye inflammation early to prevent vision loss.
Surgical Care
Surgery is rarely needed, but it may be required if joints are severely damaged or unstable, especially in the neck.
Procedures include:
- Cervical fusion: Stabilizes the neck in cases of severe arthritis or spinal instability.
- Joint replacement: For older adolescents with permanent damage once growth is complete.
Recovery and What to Expect After Treatment
Most children respond well to medications and therapy. Regular follow-ups are essential to adjust treatments and monitor growth. Physical activity and school participation are encouraged, though adjustments may be needed during flare-ups. With consistent care, many children achieve remission or long periods without symptoms.
Possible Risks or Side Effects (Complications)
Without proper treatment, JIA can cause:
- Permanent joint damage or deformity
- Growth disturbances in affected limbs
- Chronic pain or fatigue
- Eye complications leading to vision loss
- Cervical spine instability
Medication side effects—such as immune suppression or gastrointestinal irritation—require regular monitoring by the physician.
Long-Term Outlook (Prognosis)
Many children with JIA lead active, independent lives. Some may experience complete remission, while others require ongoing medication. Early diagnosis and multidisciplinary care improve long-term outcomes and help prevent permanent joint damage.
Out-of-Pocket Costs
Medicare
CPT Code 20610 – Joint Aspiration/Injection (Large Joint): $15.12
CPT Code 27323 – Synovial Biopsy (Open): $63.18
CPT Code 29870 – Arthroscopy, Diagnostic: $131.77
CPT Code 29876 – Arthroscopic Synovectomy: $155.89
CPT Code 27340 – Open Synovectomy: $90.62
Under Medicare, patients are responsible for 20% of the approved amount for these procedures after meeting their annual deductible. Supplemental insurance plans, such as Medigap, AARP, or Blue Cross Blue Shield, typically cover this remaining 20%, meaning most patients have little to no out-of-pocket costs for Medicare-approved procedures. These supplemental plans are designed to work directly with Medicare, providing full coverage for both diagnostic and therapeutic joint interventions used to manage Juvenile Idiopathic Arthritis.
If you have a secondary insurance plan—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer after Medicare has processed the claim. Once your deductible is met, the secondary plan may pay any remaining coinsurance or other balances. Most secondary insurance policies include a small deductible, typically between $100 and $300, depending on your plan and whether the services are performed in-network.
Workers’ Compensation
If the arthritis or joint inflammation occurred due to repetitive joint strain or occupational injury, Workers’ Compensation will fully cover all treatment costs, including joint aspiration, biopsy, or surgical synovectomy. You will not have any out-of-pocket costs for covered procedures.
No-Fault Insurance
If the joint inflammation or damage was aggravated by an automobile accident, No-Fault Insurance will pay for all medically necessary treatments, including arthroscopy or open surgery, as part of your post-accident care. The only possible charge may be a small deductible depending on your policy’s terms.
Example
Emma, a 16-year-old patient with Juvenile Idiopathic Arthritis, required an arthroscopic synovectomy (CPT 29876) to reduce chronic knee swelling and pain. Her Medicare out-of-pocket cost was $155.89. Because her family carried supplemental insurance through Blue Cross Blue Shield, the 20% portion that Medicare did not cover was fully paid, leaving Emma’s family with no out-of-pocket expenses for the procedure.
Frequently Asked Questions (FAQ)
Q. Can children outgrow JIA?
A. Some children experience long-term remission, while others require ongoing care into adulthood.
Q. Is JIA the same as adult rheumatoid arthritis?
A. No. While they share features, JIA has distinct patterns, causes, and outcomes.
Q. Can exercise help JIA?
A. Yes. Regular gentle exercise improves flexibility, strength, and mood.
Q. Can JIA affect the eyes?
A. Yes. Eye inflammation (uveitis) is common and requires regular eye checkups.
Summary and Takeaway
Juvenile Idiopathic Arthritis causes chronic joint inflammation in children and can affect multiple joints, including the spine. Early diagnosis, modern medications, and physical therapy help control symptoms and prevent long-term damage. With proper treatment and family support, most children can live active, fulfilling lives.
Clinical Insight & Recent Findings
A recent study published in Science Translational Medicine developed a detailed cellular atlas of the inflamed joint tissue in children with juvenile idiopathic arthritis (JIA) using advanced single-cell and spatial transcriptomic techniques. Researchers analyzed biopsies from treatment-naïve children early in their disease and discovered that inflammation in JIA is organized into distinct cellular niches composed of specific immune and stromal cell populations.
The study identified SPP1⁺ macrophages and fibrin-associated myeloid cells as key drivers of inflammation and disease severity, with these cells expressing genes linked to JIA progression and treatment resistance. Additionally, children with JIA showed a unique enrichment of TGF-β–responsive fibroblast populations and greater vascularity compared to adults with rheumatoid arthritis, emphasizing age-specific disease mechanisms.
These findings provide critical insights for developing targeted, tissue-based treatments tailored to pediatric patients. (Study of synovial tissue architecture and pathogenic niches in juvenile idiopathic arthritis – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
JIA care involves a multidisciplinary team of pediatric rheumatologists, orthopedic surgeons, physical therapists, ophthalmologists, and rehabilitation specialists, working together to manage all aspects of the condition.
When to See a Specialist?
Seek care if your child has:
- Persistent joint swelling or stiffness lasting more than 6 weeks
- Unexplained fever or rash
- Painful, swollen joints limiting movement
- Red or irritated eyes
When to Go to the Emergency Room?
Go to the ER if your child experiences:
- Sudden severe neck pain or stiffness
- Loss of limb movement or coordination
- Visual changes or eye pain
- Unexplained high fever with rash and joint pain
What Recovery Really Looks Like?
Children typically experience symptom relief with consistent treatment. Physical therapy and an active lifestyle help maintain strength and flexibility. Emotional and family support play a vital role in long-term adjustment and confidence.
What Happens If You Ignore It?
Untreated JIA can cause irreversible joint damage, growth delays, and spinal instability. Eye inflammation can lead to blindness if not detected early.
How to Prevent It?
There is no known prevention for JIA, but early diagnosis and treatment prevent complications. Regular follow-ups and adherence to therapy reduce flare-ups and long-term damage.
Nutrition and Bone or Joint Health
A balanced diet rich in calcium, vitamin D, and protein supports bone strength. Omega-3 fatty acids and antioxidants from fish, nuts, and fruits may help reduce inflammation. Maintaining a healthy weight eases stress on joints.
Activity and Lifestyle Modifications
Encourage low-impact activities like swimming or cycling to keep joints flexible without strain. Adequate rest, good posture, and supportive footwear help reduce pain. Ongoing physical therapy ensures strength and stability as the child grows.

