Sacroiliac (SI) Joint Dysfunction occurs when the joint between the sacrum (the base of the spine) and the iliac bones of the pelvis becomes inflamed, unstable, or degenerative. The SI joint connects the spine to the pelvis and helps absorb the impact of walking, lifting, and twisting. Dysfunction in this joint can lead to lower back pain, buttock pain, or pain radiating down the legs.
In severe or chronic cases where conservative treatments fail, SI joint fusion surgery may be recommended to stabilize the joint and relieve pain.
How Common It Is and Who Gets It? (Epidemiology)
SI joint dysfunction is responsible for 15% to 30% of chronic lower back pain cases. It can affect people of all ages but is most common in adults over 40 and in women, particularly after pregnancy. Individuals who have had prior lumbar spinal fusion or pelvic trauma are also at higher risk.
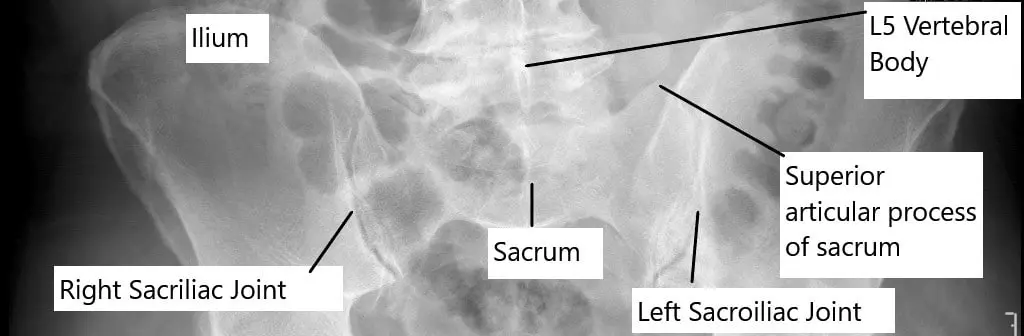
Bilateral sacroiliac joints as seen on X-ray of the pelvis in anteroposterior view.
Why It Happens – Causes (Etiology and Pathophysiology)
The SI joint can become painful or unstable due to:
- Repetitive stress or trauma
- Degenerative arthritis or wear and tear with age
- Inflammatory diseases such as ankylosing spondylitis or Reiter’s disease
- Pregnancy or childbirth, which loosens pelvic ligaments
- Previous spine surgery, especially lumbar fusion, which alters biomechanics
- Infections or tumors (rare causes)
Over time, these factors can lead to inflammation, degeneration, and eventually restricted or painful movement in the joint.
How the Body Part Normally Works? (Relevant Anatomy)
The sacroiliac joint lies between the sacrum (a triangular bone at the base of the spine) and the iliac bones of the pelvis. Strong ligaments and muscles provide stability while allowing small gliding and rotating movements.
This limited motion helps distribute forces from the upper body to the legs and acts as a shock absorber during daily activities.
When the joint becomes inflamed or unstable, pain can develop in the lower back, buttocks, or legs.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of SI joint dysfunction can mimic other spine or hip problems. Common signs include:
- Dull or aching pain in the lower back or buttocks
- Pain radiating down the thigh or leg (sometimes mistaken for sciatica)
- Increased discomfort when standing, climbing stairs, or sitting for long periods
- Relief with a tight belt or brace that supports the pelvis
- Stiffness or limited motion in the lower back
- Difficulty turning in bed or getting out of a car
Pain is usually felt on one side but can occur on both sides of the pelvis.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis requires a careful combination of physical examination and imaging:
- Physical tests: Maneuvers such as the FABER test (Flexion, Abduction, External Rotation) and Gaenslen’s test reproduce SI joint pain.
- Imaging: X-rays, CT scans, or MRI may reveal degeneration or inflammation, though findings are often nonspecific.
- Diagnostic injection: A local anesthetic injected into the SI joint under imaging guidance can confirm the diagnosis if pain relief follows.
Classification
SI joint dysfunction can be classified based on its cause:
- Degenerative: Age-related or mechanical wear.
- Inflammatory: Related to systemic conditions like ankylosing spondylitis.
- Traumatic: Caused by injury or repetitive strain.
- Post-surgical: After lumbar fusion or pelvic surgery.
It can also be described as hypermobility (too much motion) or hypomobility (too little motion).
Other Problems That Can Feel Similar (Differential Diagnosis)
SI joint dysfunction may be mistaken for:
- Lumbar disc herniation or spinal stenosis
- Hip arthritis
- Piriformis syndrome
- Facet joint arthritis
- Sciatica or nerve compression
Treatment Options
Non-Surgical Care
Most patients improve with conservative therapy.
- Physical therapy: Strengthens core, pelvic, and back muscles to stabilize the joint.
- Medications: NSAIDs reduce inflammation and pain.
- Injections: Corticosteroid injections provide temporary relief by reducing inflammation.
- Pelvic belts: Help stabilize hypermobile joints, particularly after pregnancy.
- Lifestyle modifications: Avoid prolonged sitting or uneven weight-bearing.
Interventional Care
If symptoms persist after conservative management, interventional procedures may be recommended:
- Radiofrequency ablation (RFA): Uses heat to destroy pain-transmitting nerves in the SI joint.
- SI joint fusion surgery: Fuses the sacrum and ilium to eliminate movement and stabilize the joint.
Understanding SI Joint Fusion Surgery
SI joint fusion is a surgical procedure designed to permanently stabilize the joint by fusing the sacrum and ilium.
Indications for surgery include:
- Persistent SI joint pain despite 6 months of conservative care
- Confirmed diagnosis via SI joint injection
- Significant joint instability or degeneration
Techniques:
- Open fusion: Larger incision, direct visualization of the joint.
- Minimally invasive fusion: Smaller incisions and specialized implants for faster recovery.
Recovery:
Most patients go home the same day or after one night. Full recovery takes several months, with physical therapy starting after initial healing. Fusion eliminates joint motion but significantly reduces pain in most cases.
Recovery and What to Expect After Treatment
- Early recovery: Patients may use crutches or a walker initially.
- Rehabilitation: Gradual return to activity with guided physical therapy.
- Long-term: Pain relief is typically achieved within 3–6 months as the bone fully fuses.
Minimally invasive techniques allow faster healing and reduced postoperative pain.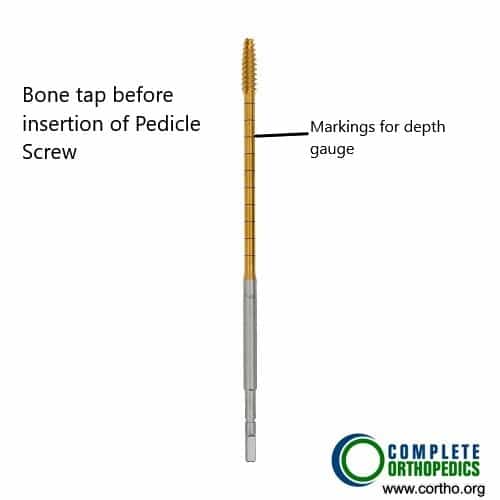
Bone tap
The bone is used for creating the path for the screw to engage in the bone. The bone tap has markings used to limit the depth of insertion during surgery.
Instruments used in posterior sacral fusion
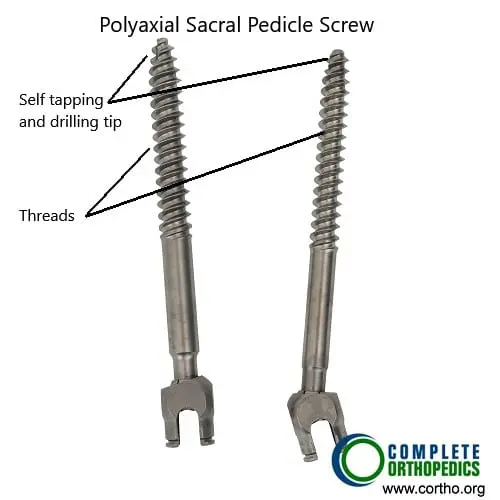
Poly-axial sacral pedicle screws
The pedicle screws with the help of instruments shown above are used in sacral fusion and with the lumbar vertebra and the iliac bone to achieve stabilization at the sacroiliac and the L5-S1 joint.
Possible Risks or Side Effects (Complications)
Complications are rare but may include:
- Infection or bleeding
- Nerve irritation or numbness
- Implant loosening or failure
- Non-union (failure of bones to fuse)
- Persistent or recurrent pain
Proper patient selection and surgical technique minimize these risks.
Long-Term Outlook (Prognosis)
Most patients experience significant and lasting relief after SI joint fusion surgery. Studies report improvement in pain and function in over 80% of cases. Physical therapy and weight management help maintain long-term results.
Out-of-Pocket Costs
Medicare
CPT Code 27279 – Minimally Invasive SI Fusion: $190.37
CPT Code 27280 – Open SI Fusion: $332.18
CPT Code 27096 – Diagnostic/Therapeutic SI Joint Injection (if applicable): $37.59
Under Medicare, 80% of the approved amount for these procedures is covered once the annual deductible is met. Patients are responsible for the remaining 20%. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—typically cover this 20%, meaning most patients have little to no out-of-pocket cost for Medicare-approved SI joint procedures. These supplemental plans work directly with Medicare to ensure that patients undergoing minimally invasive or open SI fusion experience minimal financial burden.
If you have secondary insurance—such as Employer-Based Plans, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer after Medicare. Once your deductible is satisfied, these plans can cover the remaining coinsurance or balance. Secondary plans usually carry a small deductible ranging from $100 to $300, depending on your policy and provider network.
Workers’ Compensation
If your SI joint dysfunction or instability was caused by a work-related injury, Workers’ Compensation will pay for all treatment-related expenses, including injections, minimally invasive, or open fusion procedures. You will have no out-of-pocket costs for approved treatments under Workers’ Compensation coverage.
No-Fault Insurance
If your SI joint condition resulted from a motor vehicle accident, No-Fault Insurance will cover all necessary medical and surgical costs, including diagnostic injections and fusion surgery. The only potential charge may be a small deductible depending on your specific policy terms.
Example
Michelle, a 66-year-old patient, underwent minimally invasive sacroiliac fusion (CPT 27279) following persistent SI joint pain unresponsive to injections. Her Medicare out-of-pocket cost was $190.37. Because she carried supplemental insurance through AARP Medigap, the 20% that Medicare did not cover was fully paid, leaving her with no out-of-pocket expenses for the procedure.
Frequently Asked Questions (FAQ)
Q. What causes sacroiliac joint dysfunction?
A. The condition may result from wear and tear, previous back surgery, trauma, pregnancy, or inflammatory diseases like ankylosing spondylitis.
Q. How is SI joint dysfunction diagnosed?
A. Diagnosis involves physical tests, imaging studies, and a confirmatory SI joint injection that relieves pain.
Q. When is SI joint fusion surgery recommended?
A. Surgery is considered only after conservative treatments—like therapy, injections, and medication—fail to provide lasting relief.
Q. What is recovery like after SI joint fusion?
A. Most patients return to light activities within weeks and experience long-term pain relief once the joint fully fuses in 3–6 months.
Summary and Takeaway
Sacroiliac Joint Dysfunction is a common cause of lower back and pelvic pain, often misdiagnosed as a spinal problem. When conservative measures fail, SI joint fusion surgery offers a reliable solution by stabilizing the joint and relieving pain. With modern minimally invasive techniques, most patients experience fast recovery and durable results.
Clinical Insight & Recent Findings
A recent meta-analysis protocol outlined a systematic approach to evaluate the surgical and clinical efficacy of minimally invasive sacroiliac joint (SIJ) fusion compared with conservative treatment. The authors noted that SIJ dysfunction accounts for up to 30% of chronic low back pain cases, yet conservative therapies such as medications, physical therapy, and injections relieve symptoms in only about 50% of patients.
Advances in technology have made minimally invasive SIJ fusion a common procedure, offering shorter recovery times and fewer complications compared with traditional open surgery. The meta-analysis aims to synthesize recent data showing fusion rates ranging from 13% to 100% and assess patient-reported outcomes using measures such as the Visual Analogue Scale and Oswestry Disability Index.
The review emphasizes the need for standardized imaging criteria—preferably CT confirmation of trabecular bone bridging—to define true fusion success. Findings are expected to clarify the long-term benefits, fusion durability, and cost-effectiveness of minimally invasive SIJ fusion, providing evidence to guide surgical decision-making. (Study of minimally invasive sacroiliac joint fusion outcomes – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is performed by orthopedic spine surgeons or neurosurgeons, often working with pain specialists, physical therapists, and rehabilitation teams.
When to See a Specialist?
You should consult a spine or orthopedic specialist if you experience:
- Chronic pain in the lower back or buttocks
- Pain radiating down the leg not caused by a herniated disc
- Worsening pain when standing or climbing stairs
When to Go to the Emergency Room?
Seek emergency care if you develop:
- Severe lower back pain with fever (possible infection)
- Sudden inability to walk or move your legs
- Loss of bladder or bowel control
What Recovery Really Looks Like?
Patients gradually return to normal activity over several months. Pain and stiffness decrease as fusion stabilizes the joint. Physical therapy enhances strength and flexibility for long-term stability.
What Happens If You Ignore It?
Untreated SI joint dysfunction may lead to chronic pain, pelvic instability, and reduced mobility. Long-term inflammation can also contribute to arthritis in nearby joints.
How to Prevent It?
- Maintain strong core and pelvic muscles.
- Practice good posture and proper lifting techniques.
- Avoid repetitive twisting or impact activities.
- Manage body weight and stay active.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and omega-3 fatty acids supports bone strength and reduces inflammation. Staying hydrated helps joint function and healing.
Activity and Lifestyle Modifications
Engage in low-impact activities such as walking, swimming, or yoga to keep joints mobile. Avoid prolonged sitting and use proper ergonomic support when standing or working.
¿Tienes más preguntas?
What are the most common causes of sacroiliac joint dysfunction?
Common causes include trauma (like falls or car accidents), degenerative conditions like osteoarthritis, pregnancy (due to hormonal changes and increased joint laxity), inflammatory conditions (like ankylosing spondylitis), and previous spinal surgeries that alter the biomechanics of the joint.
How can I tell if my lower back pain is due to SI joint dysfunction?
SI joint dysfunction often causes pain in the lower back, buttocks, and sometimes the legs. The pain is typically on one side and worsens with activities like sitting, standing, or walking. Specific tests performed by a doctor, like the FABER or Gaenslen test, can help identify SI joint pain.
Can SI joint dysfunction resolve on its own, or does it always require treatment?
In some cases, mild SI joint dysfunction may resolve with rest, activity modification, and over-the-counter pain medications. However, persistent or severe cases typically require medical intervention, such as physical therapy, injections, or in some cases, surgery.
What are the main differences between SI joint dysfunction and sciatica?
SI joint dysfunction pain is usually localized to the lower back and buttocks, potentially radiating down the leg but not past the knee. Sciatica, however, involves nerve compression in the spine and causes pain that radiates down the leg to the foot, often accompanied by tingling or numbness.
What types of exercises are recommended for SI joint dysfunction?
Exercises that strengthen the core, improve flexibility, and stabilize the pelvic region are beneficial. This includes stretching the iliopsoas and piriformis muscles, strengthening the gluteal muscles, and performing gentle yoga or Pilates exercises designed for lower back stability.
How effective is physical therapy for treating SI joint dysfunction?
Physical therapy is highly effective for many patients with SI joint dysfunction. A well-structured program focusing on strengthening the core, pelvic floor, and stabilizing muscles around the joint can reduce pain and improve function significantly.
Are there any specific activities I should avoid if I have SI joint dysfunction?
Avoid activities that place excessive strain on the lower back and pelvis, such as heavy lifting, high-impact sports, prolonged sitting or standing, and twisting motions. It’s also advisable to avoid uneven surfaces when walking or running.
What is the role of injections in treating SI joint dysfunction?
Injections, particularly corticosteroids, can reduce inflammation and provide pain relief in the SI joint. These are often used when other conservative treatments have failed. Diagnostic injections can also confirm if the SI joint is the source of pain.
How long does the relief from SI joint injections typically last?
The relief from SI joint injections varies; some patients experience relief for several weeks to months, while others may only get temporary relief. The effectiveness can depend on the underlying cause of the dysfunction and the severity of the condition.
When should I consider SI joint fusion surgery?
SI joint fusion is considered when conservative treatments, such as physical therapy, injections, and medications, have not provided sufficient relief, and the pain significantly impacts daily activities. It’s typically a last resort for chronic, severe cases.
What is radiofrequency ablation, and how does it help with SI joint pain?
Radiofrequency ablation (RFA) is a procedure that uses heat generated by radio waves to disrupt nerve signals transmitting pain from the SI joint. It can provide long-term relief for patients who haven’t responded well to other treatments.
What are the risks associated with SI joint fusion surgery?
Risks include infection, nerve damage, blood clots, and complications from anesthesia. There’s also the potential for continued pain if the surgery doesn’t fully resolve the dysfunction. Recovery can take several months, and there may be limitations on activity during this time.
What is the recovery process like after SI joint fusion?
Recovery involves a period of limited activity to allow the joint to heal, followed by physical therapy to restore strength and mobility. Full recovery can take several months, during which patients gradually return to normal activities.
How successful is SI joint fusion in relieving pain?
SI joint fusion has a high success rate in relieving pain for patients with confirmed SI joint dysfunction, with many patients experiencing significant or complete pain relief. Success depends on accurate diagnosis and appropriate surgical technique.
Will I be able to return to normal activities after SI joint fusion surgery?
Most patients can return to their normal activities, including work and exercise, after completing their recovery and rehabilitation. However, high-impact activities may need to be modified to avoid placing excessive stress on the fused joint.
Is there anything I can do to prevent SI joint dysfunction from recurring?
Maintaining a healthy weight, staying active with regular exercise, practicing good posture, and avoiding activities that strain the lower back and pelvis can help prevent recurrence. Strengthening the core and pelvic muscles is particularly important.
Can SI joint dysfunction be misdiagnosed as another condition?
Yes, SI joint dysfunction can be misdiagnosed as lumbar spine issues, hip problems, or sciatica because the symptoms often overlap. Accurate diagnosis requires a thorough evaluation by a healthcare professional, including specific tests and possibly imaging studies.
Are there any long-term consequences of untreated SI joint dysfunction?
If left untreated, SI joint dysfunction can lead to chronic pain, decreased mobility, and compensatory issues in other parts of the spine or hips. It may also contribute to degenerative changes in the joint, worsening the condition over time.
If left untreated, SI joint dysfunction can lead to chronic pain, decreased mobility, and compensatory issues in other parts of the spine or hips. It may also contribute to degenerative changes in the joint, worsening the condition over time.
Pregnancy increases SI joint mobility due to hormonal changes that relax the ligaments. This, combined with the additional weight and altered posture, can lead to SI joint pain. Treatments include wearing a pelvic support belt, physical therapy, and modifying activities to reduce strain.
Can weight loss improve symptoms of SI joint dysfunction?
Yes, losing excess weight can reduce the strain on the SI joint, potentially improving symptoms and reducing the risk of further joint degeneration. A healthy diet combined with regular exercise can be beneficial.
Is SI joint dysfunction common in athletes, and what sports are most likely to cause it?
SI joint dysfunction is relatively common in athletes, particularly in sports that involve repetitive or asymmetric loading, such as running, gymnastics, soccer, and football. Proper training, conditioning, and technique are crucial to prevent injury.
Can lifestyle changes alone be enough to manage SI joint dysfunction?
In mild cases, lifestyle changes such as improving posture, regular exercise, avoiding triggers, and maintaining a healthy weight may be sufficient to manage SI joint dysfunction. However, more severe cases often require additional medical treatments.
What should I expect during my first consultation for SI joint dysfunction?
During your first consultation, the specialist will take a detailed medical history, perform a physical examination, and may order imaging tests. They will discuss your symptoms, potential causes, and treatment options tailored to your condition.
How can I find the right specialist to treat my SI joint dysfunction?
Look for a healthcare provider who specializes in musculoskeletal conditions, such as an orthopedic surgeon or a pain management specialist. It’s important to find someone with experience in diagnosing and treating SI joint dysfunction specifically.

