Spondylolisthesis is a condition in which one vertebra slips forward over the one beneath it. This slippage most commonly occurs in the lower back (lumbar spine) and can range from mild to severe. Depending on how much the vertebra has shifted, patients may experience lower back pain, leg pain, numbness, or, in rare cases, paralysis or loss of bladder and bowel control.
The condition can occur in young athletes from stress injuries or in older adults due to degenerative (wear-and-tear) changes. Most cases respond well to non-surgical treatment, while surgery is reserved for severe or persistent symptoms.
How Common It Is and Who Gets It? (Epidemiology)
Spondylolisthesis affects about 4–6% of the population. It is more common in:
- Young athletes, especially those involved in sports that require repetitive bending and twisting, such as gymnastics, football, or weightlifting.
- Older adults, where it develops due to arthritis and degeneration of the spine.
- Women, who are slightly more likely to develop degenerative spondylolisthesis.
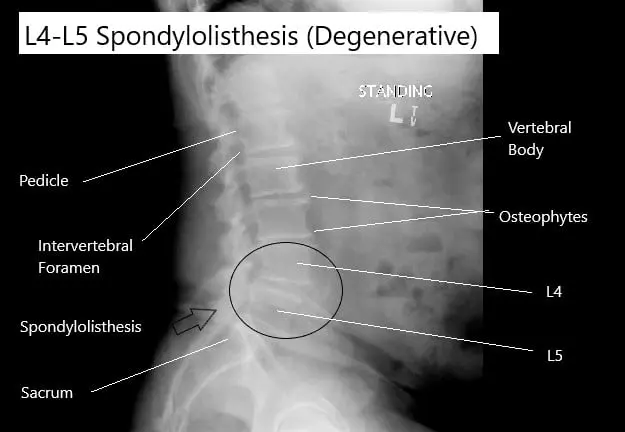
X-ray showing degenerative spondylolisthesis of the L4-L5 vertebrae.
Why It Happens – Causes (Etiology and Pathophysiology)
Spondylolisthesis can have different causes based on age and underlying spinal conditions:
- Developmental (congenital): A malformation of the vertebra present at birth makes the spine more vulnerable to slipping.
- Isthmic (pars fracture): A stress fracture in a small section of bone (pars interarticularis) weakens the spine, leading to slippage.
- Degenerative: Age-related wear of discs and joints causes instability, most often at the L4–L5 level.
- Traumatic: Direct injury from accidents may fracture the vertebra.
- Pathological: Bone diseases or tumors weaken the spine.
In degenerative spondylolisthesis, disc dehydration and joint arthritis reduce spinal stability, allowing vertebrae to shift out of alignment.
How the Body Part Normally Works? (Relevant Anatomy)
The spine is made up of 24 vertebrae stacked on top of each other. Each vertebra connects through facet joints and intervertebral discs that act as cushions, allowing flexibility and stability.
When a vertebra slips forward, it can narrow the spinal canal or pinch nearby nerves, causing pain, muscle weakness, or numbness.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms depend on the severity of slippage and whether nerves are compressed. Common signs include:
- Low back pain, often worse with activity or standing.
- Pain radiating to the buttocks or legs (sciatica).
- Tight hamstrings and stiffness.
- Weakness or numbness in the legs or feet.
- Difficulty walking or standing upright.
- Bowel or bladder dysfunction in severe cases (cauda equina syndrome).
Patients may notice pain when bending backward, with relief while resting or leaning forward.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis involves medical history, physical exam, and imaging tests:
- X-rays: Identify and grade the degree of slippage.
- Oblique X-rays: Reveal fractures of the pars interarticularis.
- MRI: Shows soft tissue and nerve compression.
- CT scan: Provides detailed images of bone structures.
- Bone scan: Detects active stress fractures or recent injuries.
Spondylolisthesis is graded using the Meyerding classification based on the percentage of vertebral slippage.
Classification
There are several types of spondylolisthesis:
- Type I – Congenital (Dysplastic): Vertebral malformation present at birth.
- Type II – Isthmic: Caused by stress fracture in the pars interarticularis.
- Type III – Degenerative: Age-related wear of discs and joints.
- Type IV – Traumatic: Due to spinal injury.
- Type V – Pathological: Caused by bone disease, infection, or tumor.
It can also be classified by severity of slip:
- Grade I: <25% slippage
- Grade II: 25–50%
- Grade III: 50–75%
- Grade IV: >75%
- Grade V: Complete slippage (spondyloptosis)
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may mimic spondylolisthesis include:
- Lumbar disc herniation
- Spinal stenosis
- Degenerative disc disease
- Hip arthritis
- Sacroiliac joint dysfunction
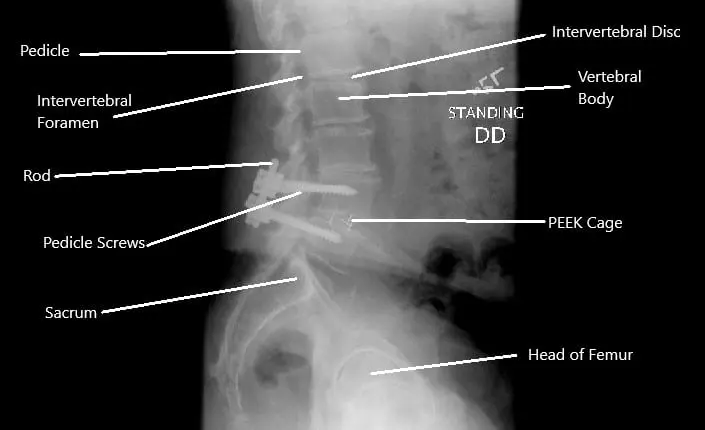
X-ray showing decompression and fusion of the L4-L5 vertebrae.
Treatment Options
Non-Surgical Care
Most cases improve with conservative management:
- Rest and activity modification: Avoid heavy lifting or twisting.
- Medications: NSAIDs and muscle relaxants reduce pain and inflammation.
- Physical therapy: Focused on core strengthening, stretching, and posture training.
- Bracing: May help stabilize the spine in acute or athletic injuries.
- Epidural steroid injections: Reduce nerve irritation and inflammation.
Surgical Care
Surgery is considered for patients with:
- Severe or progressive slippage (Grade III or IV)
- Persistent pain after 6–9 months of conservative therapy
- Neurological deficits (numbness, weakness, or bowel/bladder issues)
Common surgical options include:
- Pars repair: Fixes small fractures in the pars interarticularis.
- Decompression (laminectomy): Removes tissue pressing on the nerves.
- Spinal fusion: Stabilizes the affected vertebrae using screws, rods, or bone grafts.
- Vertebrectomy: Rarely performed in complete slippage cases.
Minimally invasive techniques allow quicker recovery and less blood loss.
Recovery and What to Expect After Treatment
- Non-surgical recovery: Most patients improve within 3–6 months with therapy.
- Post-surgery recovery: Patients usually walk within a day and return to light activities in 4–6 weeks.
- Fusion recovery: Full recovery may take several months while the bone heals.
Physical therapy is vital after surgery to restore movement and strength.
Possible Risks or Side Effects (Complications)
- Infection or bleeding
- Nerve injury
- Hardware failure or non-fusion
- Persistent back pain or recurrence
- Blood clots or anesthesia risks
Long-Term Outlook (Prognosis)
The outlook for spondylolisthesis is excellent with proper treatment. Most patients regain full mobility and return to normal activity. Early treatment of pain and nerve symptoms prevents long-term complications or deformity.
Out-of-Pocket Costs
Medicare
CPT Code 63047 – Decompression (Laminectomy): $271.76
CPT Code 63030 – Discectomy (Removal of Herniated Disc): $225.06
CPT Code 22612 – Posterior Lumbar Fusion (PLF): $382.85
CPT Code 22630 – Interbody Fusion (PLIF/TLIF): $387.42
CPT Code 22842 – Instrumentation (Rods, Screws, Plates – 3–6 Segments): $185.26
Under Medicare, 80% of the approved cost for these spinal procedures is covered after the annual deductible has been met. Patients are responsible for the remaining 20%. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—typically cover this 20%, meaning that most patients have little or no out-of-pocket costs for Medicare-approved spinal surgeries. These supplemental plans are designed to work alongside Medicare, providing full coverage for decompression and stabilization procedures like laminectomy, discectomy, and fusion.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it functions as a secondary payer after Medicare has processed your claim. Once your deductible is met, the secondary plan often pays the remaining coinsurance or balance. Most secondary insurance plans include a small deductible, usually between $100 and $300, depending on your specific policy and provider network.
Workers’ Compensation
If your lumbar spine condition requiring decompression or fusion resulted from a work-related injury, Workers’ Compensation will pay all costs related to your treatment, including surgery, hospitalization, and rehabilitation. You will not have any out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your spinal condition or injury was caused or worsened by an automobile accident, No-Fault Insurance will cover all necessary medical and surgical procedures, including decompression, discectomy, and fusion. The only potential cost would be a small deductible based on the terms of your policy.
Example
James, a 67-year-old patient with lumbar stenosis and disc herniation, underwent decompression (CPT 63047) and posterior lumbar interbody fusion (CPT 22630) for pain relief and stability. His Medicare out-of-pocket costs were $271.76 and $387.42, respectively. Because he had supplemental coverage through Blue Cross Blue Shield, the remaining 20% that Medicare did not pay was covered in full, leaving him with no out-of-pocket expense for his surgery.
Frequently Asked Questions (FAQ)
Q. What causes spondylolisthesis?
A. It can result from birth defects, stress fractures in young athletes, or degeneration of spinal discs and joints in older adults.
Q. Can spondylolisthesis heal on its own?
A. Mild cases often improve with rest, physical therapy, and medications. Severe or unstable cases may require surgery.
Q. Is exercise safe with spondylolisthesis?
A. Yes. Physical therapy focused on core strengthening and posture correction is highly beneficial. Avoid activities involving heavy lifting or back extension.
Q. What is recovery like after fusion surgery?
A. Most patients walk within a day or two after surgery, and full recovery usually takes 3–6 months, depending on the fusion type.
Summary and Takeaway
Spondylolisthesis occurs when one vertebra slips forward over another, causing back pain, leg pain, or nerve compression. Most cases respond well to non-surgical treatments such as rest, therapy, and injections. Surgery—typically decompression or fusion—is reserved for severe or persistent symptoms. With early diagnosis and modern treatment, patients enjoy excellent pain relief and restored mobility.
Clinical Insight & Recent Findings
A recent review on spondylolisthesis provided an updated understanding of its causes, classifications, and modern treatment strategies. The condition, defined as the forward slippage of one vertebra over another—most commonly at L4-L5 or L5-S1—may arise from congenital, isthmic, degenerative, traumatic, or pathologic factors, as categorized by the Wiltse classification.
Degenerative spondylolisthesis, prevalent in older adults (especially postmenopausal women), results from progressive disc and facet joint degeneration, while isthmic types are associated with stress fractures in young athletes. Diagnosis involves clinical assessment, dynamic radiographs, and MRI to evaluate neural compression. The North American Spine Society (NASS) guidelines recommend conservative treatment—NSAIDs, physiotherapy, and bracing—as first-line therapy, with surgery indicated for persistent pain, instability, or neurological deficits.
Decompression combined with spinal fusion remains the standard for symptomatic degenerative and isthmic cases, improving long-term outcomes. Advances in minimally invasive fusion techniques have reduced complications and recovery times, emphasizing the importance of restoring sagittal balance and optimizing spinopelvic parameters for durable results. (Study of classification and management strategies for spondylolisthesis – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is provided by orthopedic spine surgeons or neurosurgeons, often supported by pain management specialists, physical therapists, and rehabilitation experts.
When to See a Specialist?
You should see a specialist if you experience:
- Chronic back pain unrelieved by rest
- Leg pain, tingling, or numbness
- Difficulty standing upright or walking
- Weakness or loss of coordination in the legs
When to Go to the Emergency Room?
Seek immediate care if you have:
- Loss of bladder or bowel control
- Sudden severe leg weakness or paralysis
- Unrelenting pain not relieved by medication
What Recovery Really Looks Like?
Patients undergoing non-surgical treatment usually resume daily activity within weeks. After surgery, mobility and strength gradually improve with guided physical therapy. Long-term outcomes are excellent when rehabilitation is followed diligently.
What Happens If You Ignore It?
Ignoring spondylolisthesis can lead to worsening pain, nerve compression, and permanent neurological damage. Severe cases can cause spinal deformity or cauda equina syndrome.
How to Prevent It?
- Maintain strong core and back muscles.
- Use proper lifting techniques.
- Avoid repetitive spinal extension movements.
- Treat spinal arthritis or disc problems early.
Nutrition and Bone or Joint Health
A balanced diet rich in calcium, vitamin D, and protein supports bone health and healing. Avoid smoking and excessive alcohol, as both slow bone recovery.
Activity and Lifestyle Modifications
Low-impact exercises such as swimming, yoga, and walking help maintain spinal flexibility and strength. Avoid high-impact sports or excessive bending and twisting of the back.
¿Tienes más preguntas?
What causes spondylolisthesis?
It can be caused by degenerative changes, congenital defects, trauma, or stress fractures. Degenerative spondylolisthesis is common in older adults due to aging and wear and tear.
What are the symptoms of spondylolisthesis?
Symptoms include lower back pain, stiffness, muscle tightness, pain radiating to the legs, and sometimes numbness or weakness in the legs.
What are the treatment options for spondylolisthesis?
Treatment options include physical therapy, medications, braces, and surgery. Surgery, such as spinal fusion, is considered when conservative treatments fail.
How is spondylolisthesis diagnosed?
Diagnosis involves a physical examination, medical history, and imaging studies such as X-rays, MRI, or CT scans to assess the extent of vertebral slippage.
What is XLIF surgery?
XLIF (extreme lateral interbody fusion) is a minimally invasive surgical technique used to treat spinal conditions like spondylolisthesis. It involves accessing the spine from the side of the body to remove the damaged disc and fuse the vertebrae.
How does XLIF compare to traditional open spinal surgery?
XLIF is less invasive, involves smaller incisions, results in shorter hospital stays, less blood loss, and faster recovery compared to traditional open spinal surgery.
What are the risks associated with XLIF surgery?
Risks include nerve damage, particularly to the lumbar plexus at the L4-5 level, infection, blood loss, and complications from anesthesia.
What are the benefits of XLIF surgery?
Benefits include reduced pain, improved spinal stability, shorter recovery time, and less postoperative discomfort compared to traditional open surgery.
What are the benefits of XLIF surgery?
Benefits include reduced pain, improved spinal stability, shorter recovery time, and less postoperative discomfort compared to traditional open surgery.
How long is the recovery period after XLIF surgery?
Most patients can resume normal activities within a few weeks, with full recovery taking several months. Physical therapy is often recommended to aid in recovery.
Is XLIF surgery suitable for all patients with spondylolisthesis?
XLIF is suitable for patients with grade 2 spondylolisthesis and certain degenerative conditions. However, the suitability depends on individual patient factors, which should be assessed by a surgeon.
What are the outcomes of XLIF surgery?
Outcomes include significant pain relief, improved function, and high patient satisfaction. Studies show durable clinical and radiographic improvements over time.
Are there any complications specific to the XLIF approach?
Complications specific to XLIF include potential nerve damage, particularly at the L4-5 level, due to the proximity of the lumbar plexus. Careful surgical technique and monitoring can minimize these risks.
What preoperative preparations are needed for XLIF surgery?
Preoperative preparations include a thorough medical evaluation, imaging studies, and possibly pre-surgical physical therapy to strengthen the surrounding muscles.
How is postoperative care managed after XLIF surgery?
Postoperative care involves pain management, wound care, physical therapy, and follow-up visits to monitor healing and spinal stability.
Can XLIF surgery be performed on multiple spinal levels?
Yes, XLIF can be performed on multiple spinal levels, although the complexity and risks may increase. A thorough evaluation is necessary to determine the best approach.
What are the success rates of XLIF surgery?
Success rates are high, with most patients experiencing significant pain relief and improved quality of life. Satisfaction rates are also high, with nearly all patients willing to undergo the procedure again if needed.
What is the role of neurologic monitoring during XLIF surgery?
Neurologic monitoring helps ensure the safety of the lumbar plexus and other neural structures during surgery, reducing the risk of nerve damage.
How does obesity affect the outcomes of XLIF surgery?
While obesity can pose challenges, studies show that BMI/obesity does not significantly impact the radiographic or clinical outcomes of XLIF surgery.
How does XLIF surgery address spinal stability?
XLIF surgery removes the damaged disc and places an interbody cage filled with bone graft material to maintain disc height and promote fusion, thereby stabilizing the spine.
What is the role of bone grafts in XLIF surgery?
Bone grafts, often containing demineralized bone matrices, are used to promote bone growth and fusion between the vertebrae.
What are the long-term outcomes of XLIF surgery?
Long-term outcomes are positive, with sustained pain relief, improved function, and high rates of spinal fusion. Radiographic stability is typically maintained over time.
Can XLIF surgery be combined with other surgical techniques?
Yes, XLIF can be combined with other techniques, such as posterior instrumentation, to enhance stability and achieve optimal outcomes.
How does the presence of comorbidities affect XLIF surgery outcomes?
While comorbidities can complicate surgery and recovery, studies show that they do not significantly affect the overall outcomes of XLIF surgery. Individual assessment and careful perioperative management are crucial.
What are the indications for choosing XLIF over other fusion techniques?
Indications for XLIF include the need for a minimally invasive approach, the presence of spondylolisthesis up to grade 2, and the requirement for indirect decompression.

