If spine pain becomes so severe that it disrupts daily life or is accompanied by swelling, tenderness, or redness, it’s important to seek medical attention.
At Complete Orthopedics, our expert spine specialists are adept at treating spine pain through both surgical and non-surgical means. We examine symptoms, diagnose the condition, and recommend suitable treatments, including surgery if necessary.
Serving New York City and Long Island, we partner with six hospitals to offer cutting-edge spine surgery and comprehensive orthopedic care. You can schedule a consultation with our orthopedic surgeons online or by phone.
Learn about the common causes of spine pain and the treatment options available, including when surgery might be the best choice.
Overview
Reherniation of the intervertebral disc is the recurrence of symptoms of prolapsed intervertebral disc after conservative. The re-herniation may occur through the same location, on the opposite side or there may be herniation of the disc at an adjoining level. Various factors may be responsible for re-herniation, although the incidence is low (less than 15%). The management of re-herniation may be nonsurgical or surgical depending upon the underlying condition.
The prolapsed intervertebral disc may either be a protrusion or an extrusion. In disc protrusion, the inner soft nucleus pulposus herniates through the annulus ring without an actual breach of the ring. The protrusion of the nucleus leads to thinning of the outer ring as the ring is stretched. Microdiscectomy for protrusion may increase the risk of re-herniation through a thinned-out part of the annulus.
In cases of disc extrusion, the nucleus pulposus herniates out through a defect in the annulus. The extruded disc material is removed during microdiscectomy and re-herniation may occur through the same defect if the defect in the annulus during primary herniation was large.
During a microdiscectomy surgery, the surgeon utilizes a small incision (1-1.5 inches) at the back to access the diseased intervertebral disc. The surgeon uses a magnifying operating microscope to better visualize the disc. During microdiscectomy, the surgeon proceeds to remove only a small part of the nucleus as compared to an aggressive complete discectomy during the open technique.
In the case of protrusion, the surgeon uses a blunt incision to enter the disc space and remove the free lying fragments. The surgeon removes the free lying fragments outside the disc space in the case of disc extrusion. The defect in the annulus is often closed to prevent re-herniation.
The type of surgical technique used during microdiscectomy and the type of herniation may correlate with the re-herniation risk after the surgery. The removal of insufficient disc material and inadequate closure of a large gap in the annulus may lead to re-herniation. Similarly, the thinned and stretched-out annulus is at risk of re-herniation. Wide incisions of the annulus during surgery also increase the risk of re-herniation.
Other Cuases
Other factors such as uncontrolled diabetes mellitus, smoking, obesity, may contribute to re-herniation after microdiscectomy surgery. Patients are motivated to continue normal day-to-day activities after the surgery, however, inadequate precautions and poor posture after microdiscectomy may lead to re-herniation.
The re-herniation may occur in the immediate postoperative period, few weeks to few months after the surgery, or after years following the surgery. The symptoms of re-herniation may however not be as clear as the initial symptoms for surgery. The re-herniation symptoms may be easily mistaken with continued symptoms of initial disc herniation. A long pain-free interval after microdiscectomy and subsequent development of symptoms may more clearly point towards a possible re-herniation.
The patients may complain of symptoms similar to the original complaints of disc herniation. The symptoms of disc herniation include radicular pain radiating in the thighs and the legs. The patients may also report numbness and tingling in the lower extremities.
There may be a weakness in the lower extremity muscles. However, during re-herniation, the patients may report pain different in location, intensity, and its relation with any physical activity. The difference may be due to compression at a different site or a tethering of the nerve root to epidural fibrosis.
Diagnosis
Diagnosis is made by physical examination findings which are correlated with imaging studies. During the physical examination, the surgeon may look for pain during specific maneuvers and power/sensory examination of the lower extremities. The physician may also perform a diagnostic nerve root injection in cases when the clinical diagnosis is not evident.
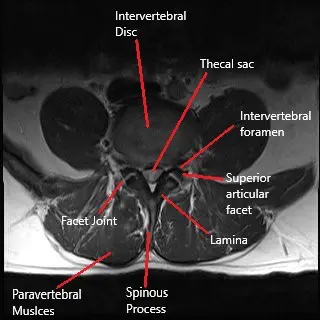
An imaging study in the form of an MRI is used to diagnose re-herniation. MRI studies with gadolinium may be used to differentiate between scar tissue and re-herniation. Other imaging studies such as an X-ray and a CT scan are more commonly used to visualize the bony anatomy of the patient. The evaluation of the bony anatomy helps in the planning of a subsequent surgery if needed.
Treatment
The management of re-herniation is similar to the primary disc prolapse. The mainstay treatment is conservative in the form of pain medications, physical therapy, and activity modification. An epidural steroid injection may also be used for the management of the symptoms.
Surgical management in the form of repeat microdiscectomy is done for re-herniation. The indications for repeat surgery are more strict as compared to primary surgery due to a high number of false-positive cases. Further, the repeat surgery may be complicated due to the presence of fibrous tissue and tethering of the nerves. Depending upon the underlying condition the surgeon may access the spine through the same incision or a different incision.
In some patients who require surgery, lumbar interbody fusion surgery may be indicated. Patients with multiple re-herniations and instability of the spinal segment are better managed with lumbar fusion surgery. During a lumbar fusion surgery, the surgeon completely removes the intervertebral disc material and uses a bone graft to weld/fuse the two adjoining vertebrae together to create stability.
¿Tienes más preguntas?
What are the signs and symptoms of reherniation?
The signs and symptoms of reherniation can include: Recurrence of radicular pain that radiates down the legs. Numbness and tingling in the lower extremities. Weakness in the muscles of the lower extremities. Pain that may differ in location and intensity from the initial herniation. A long pain-free interval followed by the return of symptoms can be indicative of reherniation.
How is reherniation diagnosed?
Diagnosis is typically made through a combination of physical examination and imaging studies. An MRI is the preferred imaging technique as it can clearly show the intervertebral disc and any recurrent herniation. MRI with gadolinium contrast can help differentiate between scar tissue and true reherniation. X-rays and CT scans can be used to evaluate the bony structures and plan for any potential surgery.
What factors increase the risk of reherniation?
Several factors can increase the risk of reherniation, including: Uncontrolled diabetes mellitus. Smoking. Obesity. Poor posture and inadequate precautions after surgery. The type of initial herniation (protrusion vs. extrusion) and the surgical technique used.
How can I reduce my risk of reherniation after surgery?
To reduce the risk of reherniation, it is important to: Follow postoperative instructions carefully. Maintain a healthy weight. Avoid smoking. Practice good posture and body mechanics. Engage in regular physical therapy and strengthening exercises as recommended.
What are the potential complications of repeat surgery for reherniation?
Complications of repeat surgery can include: Increased risk of nerve damage due to scar tissue and fibrosis. Higher likelihood of surgical complications. Potential need for lumbar fusion if there is spinal instability. Longer recovery time and potential for reduced mobility.
Can lifestyle changes help in managing reherniation?
Yes, lifestyle changes can play a significant role in managing reherniation. Maintaining a healthy weight, quitting smoking, and practicing good posture and ergonomics can help reduce the strain on the spine and lower the risk of reherniation. Regular exercise and physical therapy can also help strengthen the muscles supporting the spine.
Is it possible to fully recover from a reherniation without surgery?
Yes, it is possible to recover from a reherniation without surgery through conservative treatments. These may include physical therapy, pain management, and lifestyle modifications. However, if symptoms persist or worsen, surgical intervention may be necessary.
How effective is repeat microdiscectomy compared to the initial surgery?
Repeat microdiscectomy can be effective, but the success rate may be slightly lower compared to the initial surgery due to the presence of scar tissue and fibrosis. Careful patient selection and advanced surgical techniques can improve outcomes
Are there any new or advanced treatments for preventing reherniation?
Advanced treatments for preventing reherniation include biologic therapies such as platelet-rich plasma (PRP) and stem cell injections to promote healing and regenerate disc tissue. Minimally invasive surgical techniques and improved postoperative care protocols also contribute to better outcomes.
What lifestyle modifications are recommended after surgery to prevent reherniation?
Recommended lifestyle modifications include: Maintaining a healthy weight. Engaging in regular low-impact exercise. Avoiding smoking and excessive alcohol consumption. Practicing good posture and ergonomics. Following a balanced diet rich in nutrients that support bone and joint health.
How does smoking affect the risk of reherniation?
Smoking negatively affects the healing process by reducing blood flow and oxygen delivery to the tissues, impairing the healing of the annulus fibrosus and increasing the risk of reherniation. Quitting smoking can significantly reduce this risk and improve overall spinal health.
What should I expect during recovery from repeat microdiscectomy or lumbar fusion surgery?
Recovery from repeat microdiscectomy or lumbar fusion surgery may involve: Hospital stay of 1-3 days for lumbar fusion, with same-day discharge possible for repeat microdiscectomy. Gradual return to normal activities over several weeks to months. Physical therapy to strengthen the spine and improve mobility. Pain management strategies, including medications and possibly injections. Follow-up appointments to monitor healing and progress.

