Hip replacement surgery, or Total Hip Arthroplasty (THA), is a highly effective solution for individuals suffering from chronic hip pain or stiffness, often caused by conditions like osteoarthritis or rheumatoid arthritis. As technology has advanced, two main fixation techniques have emerged for securing the prosthetic components to the natural bone: cemented hip replacement and uncemented hip replacement. Both techniques offer distinct benefits and are chosen based on the patient’s specific needs and anatomy.
How Common It Is and Who Gets It? (Epidemiology)
Hip replacement surgery is a common procedure, especially for older adults suffering from osteoarthritis. Uncemented hip replacements are more frequently performed today, particularly in younger, healthier patients with good bone stock. Cemented hip replacements are typically used in patients with poor bone quality, such as those with osteoporosis, or those who have received bone irradiation in the past.
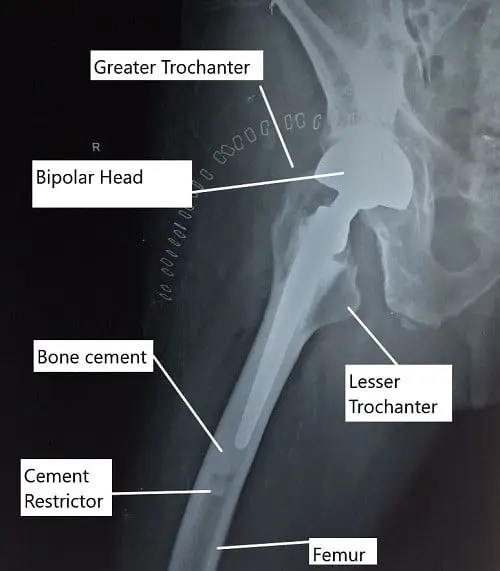
X-ray of the hip in lateral view showing a partial cemented hip replacement.
Cemented and uncemented hip arthroplasties differ in how the prosthetic implant is fixed to the natural bone. A cemented hip arthroplasty relies on bone cement to fix the implants to the bone interface. Uncemented hip replacements rely on bone on-growth over specially designed implants.
Cemented Hip Replacement
A cemented hip replacement uses a polymethylmethacrylate (PMMA) bone cement to fix the implant surface to the bone. The bone cement creates a grout and fixes the implant by acting as an interlocking surface between the implant and the bone rather than simply gluing the implant to the bone.
The bone cement is made by mixing powder and liquid components. The mixing and cementing techniques have evolved in the past decades to achieve maximum fixation. The modern mixing in the operating room involves the use of a vacuum mixer. The bone cement hardens in about 10 minutes in the OR temperature.
The modern technique of cementing involves:
- Preparation of the femoral canal using serial broaching and using a pulsatile lavage to wash the canal and remove debris.
- A cement restrictor is placed at an appropriate distance to prevent the cement from traveling down the canal.
- The cement is filled in the canal using a cement gun that pressurizes the cement injection in the canal. The gun ensures the cement is not eviscerated by the bleeding in the canal.
- The femoral stem is inserted to pressurize the cement and the tapered stem design ensures the cement pressure is maintained during the insertion. A proximal seal is made to ensure adequate pressure during the polymerization of the cement.
- The acetabulum cementing is rarely done but is similarly done to ensure adequate fixation. Beads may be used at the cement implant prosthesis to ensure an even cement distribution and to prevent bottoming out of the cement.
The cemented hip replacements are indicated only in limited cases:
- Osteopenic or osteoporotic patients have thin and porous bones. The porous bones may not support the uncemented implant due to poor bone ingrowth. A cemented implant has a better fixation as a result of cement penetration of the porous bone.
- Patients with a history of bone irradiation as a result of any malignancy who may need a hip replacement are best managed with a cemented hip replacement. The irradiated bone has poor potential for bone on-growth or bone in-growth.
- Patients with abnormally wide femoral canal are ill-suited for an uncemented hip replacement. The cement mantle ensures adequate fixation in patients with a wide femur (Dorr C).
Uncemented Hip Replacement
Uncemented hip replacement uses specially designed prosthetic components for the bone to implant fixation. The femoral component is usually covered with a porous surface on the upper end. The porous sprayed surface has microscopic contoured troughs and ridges.
The natural bone grows on and in the porous surface creating a gridlock that binds the implant to the bone. Uncemented fixation is the most common method of total hip replacement in the United states.
The operating surgeon prepares the bony femoral canal by broaching and inserting the implant slightly bigger than the final broach. The insertion of a slightly larger implant ensures a press-fit prosthesis that is snuggly fit.
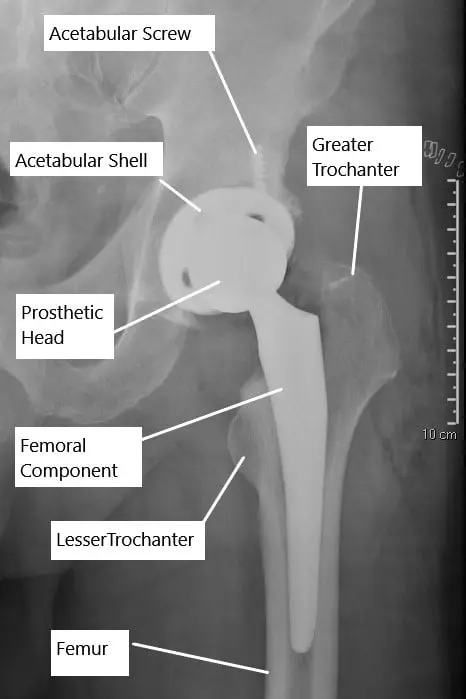
X-ray showing an uncemented total hip replacement.
The acetabular component is mostly uncemented unless the patient has poor bone stock or has a history of irradiation. The fixation is usually aided with the screws that help secure the acetabulum shell in place until the bone ingrowth occurs. The uncemented type of fixation is the preferred type of fixation in elderly patients with a good bone stock, young patients, and in the setting of a revision hip replacement surgery.
Comparison of cemented and uncemented fixation
The uncemented prosthetic designs were advanced to overcome the complication faced with cemented fixations. Cemented fixation was liable to cement breakage and subsequent inflammation around the prosthesis. The breakage, micromotion, and inflammation may lead to implant loosening.
Bone cement implantation syndrome (BCIS) is a rare complication associated with cementing during joint replacement surgery. The cement material is hypothesized to travel in the bloodstream which may cause difficulty breathing, and cardiac arrest. Pulsatile lavage is aimed to prevent cement and fat globules from leaking into the bloodstream.
The uncemented fixation is not associated with BCIS and the cement osteolysis is not associated with uncemented methods. A well-positioned uncemented implant fixation gets stronger at the interface with time as bone ingrowth occurs, however, loosening may also be associated with uncemented stems.
With a setting time of 10 mins, the cemented implants are fixed instantaneously and patients are able to bear weight right after the surgery. However, in the case of uncemented stems, only partial weight-bearing is allowed initially as the bone ingrowth takes at least 3 months. However, with recent changes in implant designs and techniques, some surgeons may allow weight-bearing right after surgery even in uncemented fixations.
Positioning of the femoral stem is easier in cemented fixation as the stem position may be individually adjusted during cementing and stem insertion. However, in the case of uncemented fixation, the position is largely determined by the reaming and broaching of the femoral marrow.
There are numerous studies that compare the complications such as stress shielding, peri-prosthetic fractures, long-term survivorship, ease of revision, etc. between uncemented and cemented techniques with variable results.
The type of fixation used in hip replacement is largely determined by the patient’s individual hip anatomy, age, and any history of medical conditions. While cemented fixation is mainly done at the extremes of age, even these patients may be candidates for uncemented fixation depending upon their bone stock.
Why It Happens – Causes (Etiology and Pathophysiology)
The most common causes of hip replacement are:
- Osteoarthritis: A degenerative joint disease where the cartilage that cushions the bones wears away, leading to pain and stiffness.
- Rheumatoid arthritis: An autoimmune condition causing inflammation in the joints.
- Avascular necrosis: A condition where the blood supply to the femoral head is reduced, causing bone death and subsequent arthritis.
- Post-traumatic arthritis: Arthritis that develops after a traumatic hip injury or fracture.
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint. The ball is the femoral head (the upper end of the femur), and the socket is the acetabulum, a part of the pelvic bone. The joint is lined with articular cartilage that allows smooth movement. Ligaments and muscles surround the joint, providing stability and enabling movement.
What You Might Feel – Symptoms (Clinical Presentation)
- Pain: In the groin, buttock, or deep within the hip joint, especially during activities such as walking, climbing stairs, or getting in/out of a chair.
- Stiffness: Difficulty moving the hip joint, making it hard to perform daily tasks.
- Loss of Function: Inability to engage in normal activities due to pain or stiffness.
How Doctors Find the Problem? (Diagnosis and Imaging)
- Physical Examination: Assesses hip mobility, strength, and alignment.
- X-rays: Show the extent of joint damage, including the wear and tear of the cartilage.
- MRI/CT scans: Sometimes used to assess the bone and soft tissue surrounding the joint.
Procedure Types or Techniques (Classification)
- Cemented Hip Replacement: Involves the use of bone cement to fix the prosthetic components to the bone. It is typically used for patients with weaker bone quality, such as older adults or those with osteoporosis.
- Uncemented Hip Replacement: Involves using specially designed prosthetic components that allow for bone ingrowth, where the bone grows into the porous surface of the implant. This is commonly used for younger patients with good bone stock.
Other Problems That Can Feel Similar (Differential Diagnosis)
- Trochanteric bursitis: Inflammation of the bursa on the outside of the hip.
- Sciatica: Pain radiating down the leg, often caused by a herniated disk in the spine.
- Hip labral tear: Damage to the cartilage around the hip socket.
Treatment Options
Conservative Treatment: Includes medications, physical therapy, lifestyle changes, or injections. These may provide relief, but when the hip arthritis becomes severe, hip replacement surgery is often required.
Recovery and What to Expect After Surgery
- Hospital Stay: Typically 1-3 days.
- Physical Therapy: Begins within 24 hours to help improve mobility and prevent complications.
- Pain Management: A combination of medications and exercises to manage postoperative pain.
- Full Recovery: Most patients recover within 3-6 months, though recovery can take longer in elderly patients.
Possible Risks or Side Effects (Complications)
- Infection: Minor infections may be treated with antibiotics, but severe infections may require surgery to remove the prosthetic.
- Blood Clots: Prevented with medications, support stockings, and early mobilization.
- Dislocation: The ball may come out of the socket, requiring repositioning.
- Implant Loosening: Over time, the implant may loosen due to wear or improper alignment.
Long-Term Outlook (Prognosis)
Hip replacement implants can last 15-20 years or more with appropriate care. The majority of patients experience significant pain relief and improved mobility after the surgery.
Out-of-Pocket Costs
Medicare
CPT Code 27130 – Uncemented or Cemented Total Hip Replacement (Total Hip Arthroplasty with Acetabulum and Femoral Head Replacement): $303.45
Medicare Part B typically covers 80% of the approved cost for this procedure once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans coordinate with Medicare to fill the coverage gap and reduce financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it serves as a secondary payer. These plans generally cover any remaining balance, including coinsurance or small deductibles, which usually range from $100 to $300, depending on your plan and provider network.
Workers’ Compensation
If your hip replacement surgery is required due to a work-related injury or degenerative hip disease caused by your job, Workers’ Compensation will cover all associated medical expenses, including surgery, rehabilitation, and follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your hip replacement surgery is needed due to an automobile accident, No-Fault Insurance will typically cover the full cost of treatment, including surgery and postoperative care. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
Richard Foster underwent cemented total hip replacement (CPT 27130) for arthritis in his hip. His estimated Medicare out-of-pocket cost was $303.45. Since Richard had supplemental insurance through Blue Cross Blue Shield, his remaining balance was fully covered, leaving him with no out-of-pocket expenses for the procedure.
Frequently Asked Questions (FAQ)
Q. Can I run after surgery?
High-impact activities like running are discouraged. However, low-impact activities like walking, swimming, and cycling are ideal.
Q. How long will my hip replacement last?
A. On average, the implant lasts 15-20 years, though some younger patients may require a revision surgery sooner due to higher activity levels.
Summary and Takeaway
Both cemented and uncemented hip replacement surgeries are highly effective for treating hip arthritis and improving mobility. Cemented hip replacements are often used for older patients or those with poor bone quality, while uncemented replacements are more common in younger, healthier patients with good bone stock. The choice between the two depends on factors such as age, bone quality, and activity level.
Who Performs This Surgery? (Specialists and Team Involved)
Orthopedic surgeons, specifically those specializing in joint replacement, perform the surgery, supported by anesthesiologists, surgical nurses, and physical therapists.
When to See a Specialist?
If you experience severe hip pain that interferes with daily activities and conservative treatments are no longer effective, consult an orthopedic surgeon to explore hip replacement surgery options.
When to Go to the Emergency Room?
Seek emergency care if you experience signs of infection (fever, redness, swelling) or extreme pain after surgery.
What Recovery Really Looks Like?
Full recovery typically takes 3-6 months, with most of the recovery occurring within the first few months. Most patients can return to light activities within a few weeks and resume normal activities after 3 months.
What Happens If You Delay Surgery?
Delaying surgery can result in further joint damage, increased pain, and complications that could make the surgery more difficult.
How to Prevent Recurrence or Failure?
Avoid high-impact activities, maintain a healthy weight, and follow your surgeon’s advice to ensure the longevity of your implant.
Nutrition and Bone or Joint Health
Ensure a balanced diet rich in calcium and vitamin D to support bone health during recovery.
Activity and Lifestyle Modifications
Engage in low-impact activities and avoid high-impact sports that stress the joint.
Do you have more questions?
What can patients do to maximize the lifespan of their knee replacement?
Following post-operative instructions, maintaining a healthy weight, staying active with low-impact exercises, and attending regular follow-up appointments with their orthopedic surgeon can all help prolong the life of a knee replacement.
Are there specific patient factors that make them better candidates for cemented or uncemented hip replacement?
Yes, certain patient factors such as age, bone quality, activity level, and underlying medical conditions may influence the suitability of cemented or uncemented hip replacement.
How does the longevity of cemented and uncemented hip replacements compare?
The longevity of cemented and uncemented hip replacements can vary, but studies have shown similar long-term outcomes for both types of procedures in appropriately selected patients.
Are there any differences in post-operative pain levels between cemented and uncemented hip replacements?
Post-operative pain levels may vary between cemented and uncemented hip replacements, with some studies suggesting less immediate post-operative pain with uncemented procedures due to reduced soft tissue trauma.
Can cemented and uncemented hip replacements be revised if necessary, and are there any differences in revision techniques?
Both cemented and uncemented hip replacements can be revised if necessary, with revision techniques tailored to the specific implant type and patient anatomy. Revision surgery may involve removing and replacing the implant components.
How do cemented and uncemented hip replacements differ in terms of surgical technique and recovery time?
Cemented hip replacements typically involve a shorter surgical time due to the immediate fixation provided by bone cement, while uncemented procedures may require longer surgical time for proper implant positioning and fixation. Recovery time may vary depending on individual patient factors.
Are there any differences in implant survivorship rates between cemented and uncemented hip replacements?
Implant survivorship rates, or the likelihood of the implant remaining in place without needing revision surgery, may be similar between cemented and uncemented hip replacements when appropriately selected and placed.
How does the risk of infection compare between cemented and uncemented hip replacements?
The risk of infection is generally low for both cemented and uncemented hip replacements when proper surgical techniques and infection prevention protocols are followed. However, some studies suggest a slightly higher risk of infection with uncemented procedures.
Can patients with osteoporosis undergo uncemented hip replacement surgery, or are there limitations?
Patients with osteoporosis can undergo uncemented hip replacement surgery, but careful consideration is needed to ensure adequate bone quality for implant fixation and stability.
Are there any limitations on physical activities or weight-bearing restrictions following cemented or uncemented hip replacement surgery?
While early post-operative weight-bearing restrictions may vary depending on surgical technique and implant fixation, most patients can gradually resume normal activities and weight-bearing as tolerated with guidance from their healthcare provider.
What are the risks of complications such as implant loosening or fracture with cemented and uncemented hip replacements?
The risks of complications such as implant loosening or fracture are generally low for both cemented and uncemented hip replacements when performed by experienced surgeons using appropriate techniques and implants. However, these risks can vary depending on individual patient factors.
How does the cost of cemented and uncemented hip replacement surgery compare, including initial expenses and long-term considerations?
The cost of cemented and uncemented hip replacement surgery can vary depending on factors such as implant type, surgical technique, hospital fees, and post-operative care. Initial expenses may differ, but long-term considerations such as revision surgery rates can impact overall costs.
Can patients with metal allergies undergo cemented or uncemented hip replacement surgery, and are there implant options available to accommodate allergies?
Patients with metal allergies can undergo cemented or uncemented hip replacement surgery with careful consideration of implant material composition. Alternative implant options such as ceramic or titanium may be available to accommodate metal allergies.
How do cemented and uncemented hip replacements differ in terms of implant stability and longevity in the younger population?
In younger patients, uncemented hip replacements may offer potential advantages in terms of bone preservation and longevity, as they rely on bone ingrowth for fixation and may facilitate future revision surgery if needed. However, long-term studies comparing outcomes between cemented and uncemented implants in younger patients are needed.
Are there any specific risks or complications associated with cemented or uncemented hip replacement surgery in obese patients?
Obese patients undergoing cemented or uncemented hip replacement surgery may face increased risks of complications such as wound healing problems, infection, implant loosening, and joint instability. Preoperative optimization and careful surgical planning are essential to minimize these risks.
Can patients with a history of previous hip surgeries undergo cemented or uncemented hip replacement surgery, and does the surgical history impact implant selection?
Patients with a history of previous hip surgeries can undergo cemented or uncemented hip replacement surgery, but the surgical history may influence implant selection and surgical approach. Careful assessment of previous surgical outcomes and bone quality is necessary to optimize implant fixation and stability.
How does the choice between cemented and uncemented hip replacement surgery impact rehabilitation protocols and post-operative care?
Rehabilitation protocols and post-operative care may vary slightly depending on the type of hip replacement surgery performed, with considerations for early weight-bearing restrictions, activity modifications, and physical therapy goals.
Can patients with compromised bone quality, such as those with osteoporosis, undergo cemented or uncemented hip replacement surgery, and are there any considerations for implant selection?
Patients with compromised bone quality, including osteoporosis, can undergo cemented or uncemented hip replacement surgery with careful consideration of implant selection and fixation techniques. Options such as cement augmentation or specialized implants may be considered to optimize stability and longevity.
How do patient age and activity level influence the decision between cemented and uncemented hip replacement surgery?
Patient age and activity level are important factors in the decision-making process for cemented versus uncemented hip replacement surgery. Younger, more active patients may benefit from uncemented implants, which offer potential advantages in bone preservation and long-term durability.
Are there any differences in the risk of complications such as dislocation or leg length discrepancy between cemented and uncemented hip replacement surgery?
The risk of complications such as dislocation or leg length discrepancy may vary between cemented and uncemented hip replacement surgery, depending on factors such as surgical technique, implant selection, and patient-specific variables. Surgeons take these factors into account to minimize the risk of complications during surgery.

