Knee cartilage injuries can significantly impair mobility, causing pain, swelling, and limited joint function. Cartilage plays a crucial role in smooth joint movement, and damage to it can lead to conditions like osteoarthritis or joint instability. This article outlines the causes, symptoms, diagnosis, treatment options, and recovery for knee cartilage injuries, offering insights into both non-surgical and surgical management approaches.
How Common It Is and Who Gets It? (Epidemiology)
Knee cartilage injuries are most common in young, active individuals, particularly athletes involved in high-impact sports like basketball, soccer, and football. Overuse or trauma to the knee joint is a common cause of cartilage damage. However, age-related degeneration of the cartilage (osteoarthritis) is more prevalent in older adults. Cartilage damage can lead to progressive knee problems, including pain, swelling, and a reduced range of motion.
Why It Happens – Causes (Etiology and Pathophysiology)
Knee cartilage injuries typically occur due to:
- Trauma or Injury: Direct impact on the knee, common in athletes, can cause tears or damage to the articular cartilage.
- Overuse: Repetitive stress on the knee joint can lead to microfractures and cartilage damage, especially in active adults.
- Congenital Abnormalities: Some individuals may be predisposed to cartilage injury due to abnormal joint biomechanics.
- Osteochondritis Dissecans: A condition where the bone under the cartilage loses its blood supply, leading to bone death and cartilage breakdown.
- Endocrine and Hormonal Disorders: Conditions like thalassemia or vascular diseases can also affect cartilage health.
- Osteoarthritis: Age-related wear and tear on the joint cartilage is the most common cause of cartilage damage in older adults.
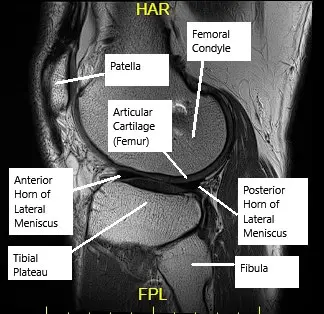
MRI of the knee showing articular cartilage.
How the Body Part Normally Works? (Relevant Anatomy)
Articular cartilage is a smooth, glistening tissue covering the ends of bones within a joint. In the knee, it cushions the femur, tibia, and patella, allowing for smooth, friction-free movement. Cartilage helps absorb shock, reduce friction, and distribute loads during activities like walking and running. However, due to its limited blood supply, damaged cartilage doesn’t heal effectively on its own, making it vulnerable to further injury and degeneration.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of knee cartilage injuries vary depending on the severity of the damage and the location of the injury. Common symptoms include:
- Knee Pain: Persistent or intermittent pain, especially with weight-bearing activities like walking, running, or sports.
- Swelling and Stiffness: The knee may become swollen and stiff, particularly after physical activity.
- Instability or Buckling: A sensation of the knee giving way, especially during sudden movements.
- Locking: The knee may lock or feel as though it cannot fully bend or straighten, often due to a “loose body” (a piece of cartilage that becomes detached and moves within the joint).
- Grinding or Popping Sensation: A feeling of grinding or catching during movement, which may indicate cartilage damage or irregular joint movement.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosing knee cartilage injuries begins with a detailed history and physical examination. The physician will assess knee function, joint stability, and any signs of swelling or tenderness. Imaging studies used to diagnose cartilage damage include:
- X-rays: Primarily used to assess bone integrity and rule out fractures or osteoarthritis.
- MRI: The most effective tool for visualizing cartilage damage, providing detailed images of the cartilage, subchondral bone, and other soft tissues.
- CT Scans: Sometimes used to evaluate joint alignment or bone defects.
- Arthroscopy: A minimally invasive procedure that allows direct visualization of the cartilage damage inside the knee joint and can be used for both diagnosis and treatment.
Classification
Knee cartilage injuries are classified based on the size, depth, and location of the defect:
- Grade 1: Superficial damage to the cartilage, typically without significant pain or functional limitations.
- Grade 2: Partial-thickness damage, affecting a larger portion of the cartilage but not reaching the subchondral bone.
- Grade 3: Full-thickness damage that extends to the underlying bone, often causing pain, swelling, and instability.
- Grade 4: Severe damage that results in exposed bone, often leading to significant knee instability and the need for surgical intervention.
Other Problems That Can Feel Similar (Differential Diagnosis)
Several conditions may mimic the symptoms of knee cartilage injuries, including:
- Meniscal Tears: Tears in the cartilage of the knee, often causing pain, swelling, and locking sensations.
- Ligament Injuries: Damage to the ACL, PCL, or MCL may cause instability, pain, and swelling similar to cartilage injuries.
- Osteoarthritis: Degeneration of the joint cartilage due to aging or overuse can lead to similar symptoms, including pain and stiffness.
Treatment Options
Non-Surgical Care
Initial treatment for knee cartilage injuries may include:
- Physical Therapy: Strengthening the muscles around the knee, improving range of motion, and reducing pain.
- Medications: NSAIDs (nonsteroidal anti-inflammatory drugs) may be used to reduce pain and inflammation.
- Bracing: Knee braces can help offload the joint and provide stability during daily activities.
- Injections: Steroid injections or viscosupplementation (hyaluronic acid injections) may help reduce inflammation and improve joint lubrication, although their use in young patients is controversial.
Surgical Care
Surgical options are typically considered for larger or more severe cartilage defects, including:
- Arthroscopic Debridement/Chondroplasty: The damaged cartilage is cleaned and smoothed using a small camera and specialized tools. This is most effective for small, superficial defects.
- Microfracture: Small holes are drilled into the bone beneath the cartilage defect to stimulate new cartilage growth. This procedure is effective for small to medium defects but requires a period of non-weight-bearing recovery.
- Mosaicplasty: Healthy cartilage from non-weight-bearing areas of the knee is transplanted into the damaged areas. This technique is effective for small, full-thickness defects.
- Allograft Osteochondral Transplantation: A donor cartilage and bone graft are used to replace damaged cartilage in large defects. This is typically used for younger patients with significant cartilage loss.
- Autologous Chondrocyte Implantation (ACI): A two-stage procedure where healthy cartilage cells are harvested from the knee, cultured in a lab, and then implanted into the damaged area. This is used for large cartilage defects.
- Total Knee Replacement (TKR): Reserved for older patients with widespread osteoarthritis and significant cartilage damage. In some cases, a partial knee replacement (unicondylar knee replacement) may be performed if only one part of the knee is affected.
For Knee replacement procedure and cost information, please click here.
Recovery and What to Expect After Treatment
Recovery after cartilage repair surgery varies depending on the procedure used:
- Physical Therapy: Rehabilitation plays a key role in recovery, with tailored exercises aimed at strengthening the knee and restoring full range of motion.
- Post-Surgical Care: Patients may need to limit weight-bearing activity during the initial recovery phase, especially after procedures like microfracture or ACI.
- Timeline: Recovery times vary, with minor procedures like debridement requiring less recovery time (several weeks) compared to more complex surgeries like ACI, which may take several months for full rehabilitation.
Possible Risks or Side Effects (Complications)
Complications associated with knee cartilage surgeries include:
- Infection: As with any surgical procedure, there is a risk of infection.
- Graft Failure: In procedures like mosaicplasty or ACI, there is a risk of the graft not integrating properly or failing over time.
- Scar Tissue Formation: Excessive scarring can limit the effectiveness of the surgery and cause stiffness.
- Implant Loosening: In cases of knee replacement, the prosthetic joint may loosen over time, requiring revision surgery.
Long-Term Outlook (Prognosis)
The long-term prognosis for knee cartilage injuries depends on the severity of the damage, the age of the patient, and the chosen treatment approach. Non-surgical treatments can help manage symptoms, but surgery may be necessary for larger defects. With appropriate treatment and rehabilitation, many patients experience significant improvement in knee function and quality of life.
Out-of-Pocket Costs
Medicare
CPT Code 29877 – Arthroscopic Debridement/Chondroplasty: $148.26
CPT Code 29879 – Microfracture: $158.02
CPT Code 29866 – Mosaicplasty (Autograft Osteochondral Transfer): $250.65
CPT Code 27415 – Allograft Osteochondral Transplantation: $325.45
CPT Code 27412 – Autologous Chondrocyte Implantation (ACI): $389.71
CPT Code 27447 – Total Knee Replacement (TKR): $303.02
CPT Code 27446 – Partial Knee Replacement (Unicondylar): $271.70
Under Medicare, 80% of the approved amount for these procedures is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—typically cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved knee surgeries. These supplemental plans work directly with Medicare to ensure full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, ranging from $100 to $300, depending on the specific policy and network status.
Workers’ Compensation
If your knee surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your knee injury requiring surgery is the result of a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses, including arthroscopic debridement, microfracture, mosaicplasty, osteochondral transplantation, ACI, total knee replacement, and partial knee replacement. The only possible out-of-pocket cost may be a small deductible depending on your individual policy terms.
Example
Sarah, a 62-year-old patient with knee arthritis, underwent partial knee replacement (CPT 27446) and also received autologous chondrocyte implantation (CPT 27412). Her estimated Medicare out-of-pocket costs were $271.70 for the partial knee replacement and $389.71 for the ACI. Since Sarah had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving her with no out-of-pocket expenses for the procedures.
Frequently Asked Questions (FAQ)
Q. What causes knee cartilage injuries?
A. Knee cartilage injuries can result from trauma, overuse, congenital abnormalities, or conditions like osteochondritis dissecans. They are common in athletes and active individuals.
Q. How is knee cartilage damage diagnosed?
A. Diagnosis involves a detailed history, physical examination, and imaging studies, including MRI or arthroscopy, to assess the extent of the cartilage damage.
Q. What treatments are available for knee cartilage injuries?
A. Treatment options range from non-surgical methods like physical therapy and medications to surgical procedures such as arthroscopic debridement, microfracture, mosaicplasty, and total knee replacement.
Q. How long does it take to recover from cartilage repair surgery?
A. Recovery times vary based on the type of surgery. Non-weight-bearing recovery may last several weeks to months, with full rehabilitation taking several months to a year, depending on the procedure.
Summary and Takeaway
Knee cartilage injuries can significantly impact mobility and quality of life, but with early diagnosis and appropriate treatment, many individuals can experience significant improvements. Surgical options, including arthroscopic and open procedures, provide effective solutions for managing cartilage defects and restoring knee function. Working closely with a healthcare provider and adhering to a rehabilitation plan can help achieve the best possible outcomes.
Clinical Insight & Recent Findings
A recent study systematically reviewed the outcomes of various surgical strategies for cartilage injuries in football players, focusing on return-to-sport and clinical results.
The study found that different techniques such as bone marrow stimulation (BMS), osteochondral autograft transplantation (OAT), matrix-assisted autologous chondrocyte transplantation (MACT), and microfractures (MFX) yielded varying results, with the fastest return-to-sport observed for debridement and BMS.
Despite the widespread use of microfractures, which allow for quicker recovery, long-term results showed a tendency for deterioration in clinical outcomes. Larger lesions typically required MACT or OAT, which provided more durable results but with a longer time to return-to-sport.
These findings highlight the importance of lesion size and treatment approach in optimizing recovery and return to sport. (“Study of cartilage injuries in football players – See PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons specializing in sports medicine or joint preservation perform most cartilage repair surgeries. Physical therapists are integral to post-surgical rehabilitation, helping restore strength and function to the knee.
When to See a Specialist?
If you experience persistent knee pain, swelling, or difficulty moving your knee, it’s important to consult an orthopedic specialist for proper evaluation and treatment.
When to Go to the Emergency Room?
Seek emergency care if you experience sudden, severe knee pain, significant swelling, or signs of infection (e.g., redness, warmth, fever) after surgery.
What Recovery Really Looks Like?
Recovery typically involves rehabilitation and physical therapy to restore knee function and strength. Full recovery time depends on the severity of the injury and the surgical technique used.
What Happens If You Ignore It?
Ignoring knee cartilage injuries can lead to long-term joint instability, further cartilage degradation, and the development of osteoarthritis, which may require more extensive surgery.
How to Prevent It?
Prevention includes maintaining a healthy weight, avoiding repetitive knee stress, and using proper technique during physical activities. Regular strengthening exercises can also help support the knee joint.
Nutrition and Bone or Joint Health
Maintaining a diet rich in calcium, vitamin D, and omega-3 fatty acids can help support joint and cartilage health, reducing the risk of injury and promoting healing.
Activity and Lifestyle Modifications
Engaging in low-impact activities like swimming, cycling, or walking can help maintain joint health without putting excessive strain on the knee.
Do you have more questions?
What are the long-term consequences of untreated kneecap maltracking?
Untreated kneecap maltracking can lead to chronic pain, cartilage damage, and increased risk of developing osteoarthritis in the knee joint over time. Seeking early treatment can help prevent these complications.
How common are cartilage injuries in the knee?
Cartilage injuries in the knee are relatively common, especially among athletes and individuals who engage in high-impact activities. They can also occur due to aging and degenerative changes in the joint.
Can cartilage injuries in the knee heal on their own without treatment?
In some cases, minor cartilage injuries may heal on their own with rest and conservative management. However, more significant injuries often require medical intervention to promote proper healing and prevent long-term complications.
Are there any specific risk factors that increase the likelihood of cartilage injuries in the knee?
Yes, several factors can increase the risk of cartilage injuries in the knee, including participating in sports with repetitive knee movements, previous knee injuries, obesity, and genetic predisposition.
How long does it typically take to recover from a cartilage injury in the knee?
The recovery time for a cartilage injury in the knee varies depending on the severity of the injury and the chosen treatment approach. In some cases, individuals may experience improvement within a few weeks, while others may require several months of rehabilitation.
Is surgery always necessary for treating cartilage injuries in the knee?
Surgery is not always necessary for treating cartilage injuries in the knee. Many cases can be effectively managed through conservative treatments such as physical therapy, pain management, and activity modification. However, surgery may be recommended for severe or complex cases.
What are the potential risks and complications associated with surgical interventions for cartilage injuries in the knee?
Surgical interventions for cartilage injuries in the knee carry certain risks and potential complications, including infection, bleeding, nerve damage, and failure of the procedure to provide the desired outcome.
Can cartilage injuries in the knee lead to long-term joint damage or arthritis?
Yes, untreated or improperly managed cartilage injuries in the knee can lead to long-term joint damage and increase the risk of developing osteoarthritis, a degenerative joint disease characterized by cartilage breakdown and inflammation.
Are there any specific exercises or activities that individuals with cartilage injuries in the knee should avoid?
Individuals with cartilage injuries in the knee should avoid high-impact activities and exercises that place excessive stress on the joint, such as running, jumping, and heavy lifting. Instead, they should focus on low-impact exercises and activities that promote joint stability and flexibility.
How can I prevent cartilage injuries in the knee from recurring?
Preventing cartilage injuries in the knee from recurring involves maintaining a healthy weight, participating in regular exercise to strengthen the muscles around the knee joint, using proper techniques during physical activities, and wearing supportive footwear.
Are there any dietary or nutritional recommendations that can help support cartilage health in the knee?
While there is no specific diet that can guarantee cartilage health, consuming a balanced diet rich in nutrients such as vitamin C, vitamin D, calcium, and omega-3 fatty acids can help support overall joint health and reduce inflammation.
Is there a specific age group more prone to cartilage injuries in the knee?
Cartilage injuries in the knee can occur in individuals of all age groups, but they are more common in older adults due to age-related changes in the joint and increased risk of degenerative conditions like osteoarthritis.
Can cartilage injuries in the knee affect other areas of the body besides the knee joint?
While cartilage injuries in the knee primarily affect the knee joint, they can also lead to compensatory changes in gait and movement patterns, potentially causing secondary issues in other areas of the body such as the hips and lower back.
Is there a difference in treatment approaches for acute versus chronic cartilage injuries in the knee?
Yes, the treatment approach for acute (recently occurred) versus chronic (long-standing) cartilage injuries in the knee may vary. Acute injuries may require immediate rest, ice, compression, and elevation (RICE) followed by conservative management, while chronic injuries may necessitate more aggressive interventions such as surgery.
Are there any non-surgical alternatives for managing cartilage injuries in the knee?
Yes, several non-surgical alternatives exist for managing cartilage injuries in the knee, including physical therapy, pain management techniques, regenerative medicine therapies, and lifestyle modifications.
Can cartilage injuries in the knee worsen over time if left untreated?
Yes, cartilage injuries in the knee can worsen over time if left untreated, leading to progressive pain, stiffness, and functional impairment. In severe cases, untreated injuries can result in irreversible joint damage and disability.
How soon after sustaining a knee injury should I seek medical attention?
It is advisable to seek medical attention promptly after sustaining a knee injury, especially if you experience persistent pain, swelling, or difficulty bearing weight on the affected knee. Early intervention can help prevent further damage and improve treatment outcomes.
Is it possible to prevent cartilage injuries in the knee altogether?
While it may not be possible to completely prevent cartilage injuries in the knee, certain preventive measures such as maintaining a healthy weight, staying physically active, using proper techniques during physical activities, and wearing supportive footwear can help reduce the risk.
Are there any specific diagnostic tests that can accurately assess the extent of cartilage damage in the knee?
Yes, diagnostic tests such as MRI (Magnetic Resonance Imaging) and arthroscopy can provide detailed images of the knee joint and accurately assess the extent of cartilage damage. These tests help guide treatment decisions and prognosis.
How does age impact the effectiveness of treatment for cartilage injuries in the knee?
Age can impact the effectiveness of treatment for cartilage injuries in the knee, with younger individuals generally having a better capacity for cartilage repair and regeneration compared to older adults. However, treatment outcomes also depend on factors such as the severity of the injury and overall health status.
Are there any specific precautions I should take during the recovery period after treatment for a cartilage injury in the knee?
During the recovery period after treatment for a cartilage injury in the knee, it is important to follow your healthcare provider’s instructions carefully, including participating in prescribed rehabilitation exercises, avoiding high-impact activities, and attending follow-up appointments for monitoring progress.
Can cartilage injuries in the knee be hereditary or genetic?
While cartilage injuries in the knee are often associated with factors such as trauma, overuse, and aging, there may also be a genetic component that predisposes some individuals to cartilage abnormalities and injuries.
Are there any specific occupational or recreational activities that increase the risk of cartilage injuries in the knee?
Yes, certain occupational or recreational activities that involve repetitive knee movements, heavy lifting, or prolonged standing can increase the risk of cartilage injuries in the knee. Examples include construction work, landscaping, and high-impact sports.
Are there any emerging treatments or technologies for cartilage injuries in the knee that show promise?
Yes, there are several emerging treatments and technologies for cartilage injuries in the knee that show promise, including tissue engineering techniques, 3D printing of cartilage implants, and advanced imaging modalities for early detection and monitoring of cartilage damage.

