At Complete Orthopedics, we specialize in diagnosing and treating back and spine conditions through personalized care and advanced surgical options. Our clinics across New York City and Long Island are connected with leading hospitals and equipped with the latest technology to deliver exceptional orthopedic and spinal care.
Cauda equina syndrome (CES) is a rare but serious condition caused by pressure on the group of nerves at the lower end of the spinal cord, called the cauda equina or “horse’s tail.” These nerves control movement and sensation in the legs as well as bladder and bowel function. Compression of these nerves is a true emergency and requires immediate surgical treatment to prevent permanent damage.
How Common It Is and Who Gets It? (Epidemiology)
Cauda equina syndrome is uncommon, affecting only a small fraction of people who experience lower back pain or disc herniation. It can occur in adults of any age but is most often seen in middle-aged individuals who develop large disc herniations or spinal injuries. Men and women are equally affected. The condition can also occur after severe trauma, spinal surgery, or rarely due to tumors or infections.
Why It Happens – Causes (Etiology and Pathophysiology)
The most common cause of cauda equina syndrome is a herniated disc in the lower back that presses on the nerve bundle. Other possible causes include:
- Spinal stenosis, or narrowing of the spinal canal
- Trauma, such as fractures or dislocations from car accidents or falls
- Tumors that grow inside the spinal canal
- Bleeding or infections that compress the nerves
- Spondylolisthesis, when one vertebra slips forward over another
When these conditions put pressure on the cauda equina nerves, blood flow to the area decreases and nerve signals stop traveling normally. If not relieved quickly, this pressure can cause lasting nerve damage.
How the Body Part Normally Works? (Relevant Anatomy)
The spinal cord carries messages between the brain and the body. It runs through the spine and ends around the level of the first lumbar vertebra. Below this point, a bundle of nerves continues downward within the spinal canal—these are called the cauda equina because they resemble a horse’s tail.
These nerves control sensation and movement in the legs, bladder, bowel, and sexual organs. Because they are exposed within the canal and not protected by bone or tissue as strongly as the spinal cord, they are more sensitive to pressure or injury.
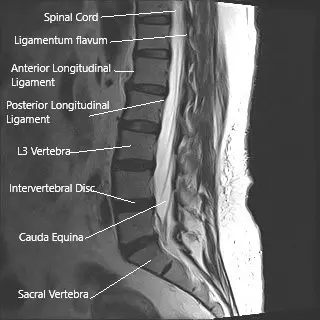
MRI of the lumbar spine in sagittal section showing cauda equina (horse’s tail)
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of cauda equina syndrome can appear suddenly or develop over time. Common signs include:
- Severe lower back pain
- Pain, numbness, or tingling in one or both legs
- Weakness in the legs or difficulty walking
- Numbness around the inner thighs, buttocks, or the area that touches a saddle (“saddle anesthesia”)
- Loss of bladder or bowel control
- Trouble starting or stopping urination, or the feeling of incomplete emptying
- Sexual dysfunction
Patients often describe not feeling toilet paper or losing the urge to urinate. These symptoms require emergency evaluation.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis starts with a careful review of symptoms and a physical and neurological exam to check strength, reflexes, and sensation in the legs and groin area.
Imaging tests help confirm the diagnosis and locate the cause of nerve pressure:
- MRI is the best imaging test, showing nerves, discs, and soft tissues in detail.
- CT scan or CT myelogram may be used if MRI is not possible.
- X-rays may identify fractures or bone problems after trauma.
- Bladder studies can assess urinary function if bladder symptoms are present.
Early diagnosis is critical—any delay in treatment can lead to permanent nerve injury.
Classification
Cauda equina syndrome is often categorized based on how complete the nerve compression is:
- Incomplete CES: Patients still have some bladder or bowel control but experience weakness, numbness, or urinary difficulties.
- Complete CES: There is total loss of bladder or bowel function and widespread numbness.
This distinction helps guide urgency and treatment approach.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions may mimic cauda equina syndrome, including:
- Lumbar disc herniation without nerve compression
- Peripheral neuropathy from diabetes
- Spinal cord compression higher up in the spine
- Multiple sclerosis
- Infections or inflammation of the spinal cord
Doctors rule these out using MRI and neurological testing.
Treatment Options
Non-Surgical Care
Because cauda equina syndrome is almost always a surgical emergency, non-surgical treatment is limited. Pain control, rest, and anti-inflammatory medication may be used briefly while preparing for surgery, but delaying decompression can lead to permanent loss of function.
Surgical Care
The main treatment is decompression surgery, performed as soon as possible—ideally within 48 hours of symptom onset. The procedure removes whatever is pressing on the nerves, restoring blood flow and nerve function.
Depending on the cause, surgery may include:
- Discectomy: Removal of the herniated disc portion that is pressing on the nerves.
- Laminectomy: Removal of part of the bone covering the spinal canal to relieve pressure.
- Fusion: Placement of screws and rods to stabilize the spine when instability or fracture is present.
Early surgery provides the best chance for recovery of leg strength and bladder and bowel control.
Recovery and What to Expect After Treatment
After surgery, patients often stay in the hospital for monitoring. Improvement in symptoms can begin quickly but may continue over months or even years.
Recovery includes:
- Physical therapy to strengthen leg muscles and restore movement.
- Bladder retraining if urinary control is affected.
- Pain management using medications and gentle stretching.
- Regular follow-up visits and imaging to ensure continued stability.
Even after successful surgery, some symptoms—especially bladder or sexual dysfunction—may take longer to improve.
Possible Risks or Side Effects (Complications)
Possible complications include:
- Persistent numbness or weakness
- Ongoing bladder or bowel problems
- Chronic pain or stiffness
- Infection or bleeding after surgery
- Nerve root injury or spinal fluid leakage
Delayed surgery increases the risk of permanent nerve damage and long-term disability.
Long-Term Outlook (Prognosis)
Outcomes depend on how quickly surgery is performed. Patients treated within 48 hours of symptom onset have the best chance of regaining bladder and leg function. Delays may result in partial recovery or permanent deficits. Lifelong follow-up and rehabilitation help maintain function and quality of life.
Out-of-Pocket Costs for Cauda Equina Syndrome (CES)
Medicare
CPT Code 63047 – Lumbar laminectomy for decompression: $271.76
CPT Code 63030 – Lumbar discectomy (if herniated disc is the cause): $225.06
CPT Code 22612 – Posterior spinal fusion (if stabilization required): $382.85
Under Medicare, patients are typically responsible for 20% of the approved amount for physician and facility services after meeting their deductible. Supplemental insurance plans, such as Medigap, AARP, or Blue Cross Blue Shield, often cover this remaining 20%, meaning patients usually have no further costs when the procedure is Medicare-approved. These plans are designed to fill the payment gap left by Medicare but do not replace it.
If you also have secondary insurance, such as an Employer-Based Plan, TRICARE, or Veterans Health Administration (VHA), it generally acts as a secondary payer after Medicare. Once your Medicare deductible is met, the secondary insurance can pay the remaining balance, including co-insurance. Deductibles for these secondary plans often range from $100 to $300, depending on the policy and network status of the provider or hospital.
Workers’ Compensation
If your Cauda Equina Syndrome is the result of a work-related injury, Workers’ Compensation will cover the entire cost of the surgical and hospital care associated with treatment. This includes decompression, discectomy, and fusion if required. You will have no out-of-pocket expenses under Workers’ Compensation coverage.
No-Fault Insurance
If your Cauda Equina Syndrome resulted from an automobile accident, No-Fault Insurance will pay for all necessary medical and surgical care, including decompression, discectomy, and spinal fusion if indicated. The only possible cost to you may be a minor deductible depending on your specific policy terms.
Example
John, age 58, developed Cauda Equina Syndrome after a large lumbar disc herniation caused severe leg weakness and urinary retention. His Medicare out-of-pocket cost for lumbar laminectomy was $271.76. Because John had supplemental insurance, the 20% portion not covered by Medicare was paid by his Medigap plan, leaving him with no out-of-pocket expense for the surgery.
Frequently Asked Questions (FAQ)
Q. Is cauda equina syndrome curable?
A. Yes, if treated quickly. Early surgery can relieve pressure and restore nerve function, though recovery may take time.
Q. Can it happen again?
A. Recurrence is rare but can occur if another disc herniation or spinal problem develops.
Q. Will I regain bladder and bowel control?
A. Many patients do, especially if treated early. The longer the delay before surgery, the lower the chance of full recovery.
Q. Is this a type of paralysis?
A. It can cause partial or complete paralysis in the legs if not treated, but early surgery can prevent permanent loss of movement.
Summary and Takeaway
Cauda equina syndrome is a medical emergency that occurs when the nerves at the bottom of the spinal cord are compressed. It causes back pain, leg weakness, numbness, and bladder or bowel problems. Immediate surgical decompression is essential to prevent permanent damage. With early diagnosis and treatment, many patients regain strength, sensation, and bladder control over time.
Clinical Insight & Recent Findings
A recent study on cauda equina syndrome (CES) emphasized the importance of urgent surgical decompression to prevent irreversible neurological damage. The research highlighted that early intervention—preferably within 48 hours of symptom onset—significantly improves recovery of motor, sensory, and bladder functions.
MRI remains the diagnostic gold standard for identifying the compression of the cauda equina nerve roots, often caused by intervertebral disc herniation, spinal stenosis, trauma, or tumors. Delayed surgery was found to increase the risk of long-term complications such as chronic pain, bladder dysfunction, and lower-limb weakness.
The findings underscore that prompt recognition of red flag symptoms—such as saddle anesthesia, bowel or bladder incontinence, and severe leg weakness—is critical for optimizing outcomes. (Study of early decompression in cauda equina syndrome – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is performed by a spine or orthopedic surgeon trained in complex spinal procedures. The care team often includes neurologists, radiologists, anesthesiologists, physical therapists, and rehabilitation specialists to support recovery.
When to See a Specialist?
You should see a spine specialist immediately if you have severe back pain with leg weakness, numbness, or trouble controlling your bladder or bowel. Early evaluation can prevent irreversible nerve damage.
When to Go to the Emergency Room?
Go to the nearest emergency room if you experience:
- Sudden loss of bladder or bowel control
- Numbness in the saddle or groin area
- Severe or worsening leg weakness
- Inability to stand or walk normally
These symptoms require urgent medical attention.
What Recovery Really Looks Like?
Recovery from cauda equina syndrome can be gradual. Some patients regain full strength and sensation within weeks, while others require months of therapy. Persistent symptoms, such as mild numbness or urinary urgency, may remain but often improve over time with rehabilitation and follow-up care.
What Happens If You Ignore It?
Delaying treatment can lead to permanent paralysis, loss of bladder and bowel control, and chronic pain. Once nerve damage occurs, it may not be reversible. Prompt recognition and surgery are essential for the best possible recovery.
How to Prevent It?
While not all cases can be prevented, maintaining good spinal health helps reduce risk:
- Maintain a healthy weight
- Exercise regularly to strengthen back muscles
- Use proper posture and lifting techniques
- Avoid smoking, which weakens spinal discs
- Address chronic back pain early with a specialist
Nutrition and Bone or Joint Health
A balanced diet rich in calcium, vitamin D, and lean protein supports bone strength and recovery after spinal surgery. Staying hydrated and maintaining a healthy weight also reduce stress on the spine.
Activity and Lifestyle Modifications
After surgery, patients should avoid bending, twisting, or heavy lifting until cleared by their surgeon. Walking and light stretching are encouraged as healing progresses. Over time, physical therapy helps rebuild strength and flexibility, allowing a safe return to work, sports, and daily activities.
Do you have more questions?
What is Cauda Equina Syndrome?
Cauda equina (Latin) means horse tail. It is a name given to the nerve roots in the lumbosacral spinal canal as they look similar to horse tail on visualization. Cauda equina syndrome is the compression of the spinal nerve roots in the lumbar and sacral area of the spine Lesions above this level leads to compression of spinal cord and is not cauda equina syndrome, but the presentation is more dramatic and carries same or more urgency as of cauda equina syndrome. Compression of the spine causes weakness of upper or lower extremities with increased reflexes and with or without involvement of the bowel or bladder. Cauda equina syndrome is essentially a clinical presentation of new onset or worsening weakness in one or both lower extremities, gait abnormality, involvement of the bladder and numbness in either lower extremity and peri genital area (sacral anesthesia). These patient may also have sexual dysfunction. The patients usually have severe back pain. Cauda equina syndrome is usually associated with pain in the back and occasionally with radiculopathy. Rarely, patients with cauda equina syndrome may present without any complaints of pain. This happens due to compression of the nerve roots in the lumbar spine and leading to dysfunction of the muscles as well as altered sensation that are taken care by the specific nerve roots. This is a severe form of presentation of nerve root compression in the lumbar spine. It can present acutely or over many months or days. It may be caused due to degeneration of disk fragment, mass in the spinal canal, bleeding in the spinal canal, intraspinal mass like tumor, fracture, gunshot or rarely with a birth defect (usually an arteriovenous malformation). The presentation can be acute or chronic depending on the pathology.
What injuries can cause cauda equina syndrome?
Fractures or dislocations of the lumbosacral spine may lead to cauda equina syndrome. These are traumatic injuries and are associated with high velocity accidents like motor vehicle accident or fall from height. Traumatic disc herniation may also lead to cauda equina syndrome.
What type of physicians take care of cauda equina syndrome?
Acute cauda equina syndrome is usually treated under the care of a spine surgeon who can be of orthopedic or a neurosurgical background. A chronic cauda equina syndrome in which a surgery has been ruled out is usually under the care of neurologist and may also need care of oncologist or radiation oncologist in cases which are associated with malignancy or metastasis.
Why is rectal exam needed in cauda equina syndrome?
The rectal exam can be of diagnostic value in cauda equina syndrome lacks rectal sphincter is associated with cauda equina syndrome and should be checked in all patients. It may be the only sign of Cauda Equina Syndrome.
How to diagnose a cauda equina syndrome?
Cauda equina syndrome is diagnosed clinically due to its characteristic presentation of new onset or worsening of weakness, gait abnormality, bowel or bladder dysfunction, sexual dysfunction and sacral anesthesia. Confirmation of diagnosis is done with advanced imaging specifically. MRI which helps to find out the level of compression as well as helps in diagnosing the pathology. In patients who have contraindications for MRI (Pacemaker, aneurysmal clip), CT scan and myelogram may be done. Confirmatory diagnosis of the pathology can only be done at the time of surgery and with the need of histopathologic examination of the tissue compressing on the nerve roots.
What are the causes of cauda equina syndrome?
Causes of acute cauda equina syndrome can be a disk fragment (most common), fracture or dislocation of the spine, a hematoma caused by bleeding in the spinal canal, vascular insult to the nerve root due to underlying systemic or local pathology, infection, inflammation, gunshot or stabbing to spine, motor vehicle accident or fall, birth defect (arteriovenous malformation). Cause of chronic cauda equina syndrome can be a slow growing mass or a degenerative spine with disk fragment or hypertrophied ligaments causing lumbar stenosis, birth defects etc. A mass can be in the form of tumor or metastasis or rarely a primary tumor of the nerve roots or the nerve elements.
Can I be disabled due to cauda equina syndrome?
Cauda equina syndrome is a disabling disease. It leads to weakness and usually with dysfunction of the bladder and sometimes bowels too. It leads to impaired gait due to the weakness of the muscles of the leg. Due to involvement of bladder, it may lead to retention or incontinence of urine leading to use of alternate methods for evacuation of the bladder. Patients may have gait problems too.
How do I know I have a cauda equina syndrome?
Patients with cauda equina syndrome usually have new onset or worsening weakness in one or both lower extremities, gait abnormality, involvement of the bladder and numbness in either lower extremity and peri genital area (sacral anesthesia). These patient may also have sexual dysfunction. The patients usually have severe back pain. These patients may have preexisting back pain and radiculopathy. Patients may have a history of cancer with or without metastasis to the spine and may have already undergone treatment for that in the past.
What do I do if I have cauda equina syndrome?
An acute onset cauda equina syndrome is a surgical emergency and the patient should go to the ER immediately. Advanced imaging should be performed as soon as possible to confirm the diagnosis after the physical examination of the patient. If a cauda equina syndrome is confirmed, a surgery may be needed to decompress the spine and allow the recovery of the nerve roots. Patients with chronic cauda equina syndrome who have insidious onset over many days or weeks, should seek medical attention to confirm the diagnosis as well as plan a possible treatment for their disease.
How common or rare is cauda equina syndrome?
Cauda equina syndrome is a rare presentation of various pathologies of the spine. Most pathologies present with back pain or/and radiculopathy. They may also develop subtle weakness, but developing profound weakness with involvement of bladder and gait is rare. It is even rarer in degenerative disk disease and lumbar canal stenosis.
What is the treatment of cauda equina syndrome?
Patients with acute presentation of cauda equina syndrome with confirmatory diagnosis on an MRI showing mass effect on the nerve roots usually will need an urgent or emergent surgery to decompress the nerve roots. They will need to be admitted to the hospital and will need to undergo physical rehabilitation for optimization of the function as well as enhance their recovery. Patients with chronic cauda equina syndrome may also need surgery depending on the pathology, but may also need adjuvant treatment especially in the cases of malignancy or metastasis in the form of chemo or radiotherapy. Occasionally these patients with chronic cauda equina syndrome can manage with adjuvant treatments only without the need for surgery. Patients with poor general condition and multiple comorbidities may have to be treated non-surgically so as to curtail the risk to their life due to the anesthesia as well as the surgery.
How is the recovery from cauda equina syndrome?
Recovery from cauda equina syndrome depends on the type of pathology, amount of compression, number of levels involved as well as the surgery performed. In most cases, the recovery will happen if their condition has been treated promptly but may not lead to full recovery of the functions. Patients will need to undergo physical rehabilitation to optimize their function as well as enhance their recovery.
Can cauda equina syndrome cause bladder problems?
Cauda equina syndrome usually causes bladder problems in the form of retention or incontinence. These patients need to be treated for their bladder problems separately so as to allow recovery and at the same time avoid complications due to the condition.
Can cauda equina syndrome cause constipation?
Cauda equina syndrome can occasionally cause involvement of bowels also which may lead to constipation in most cases.
Can cauda equina syndrome cause death?
Cauda equina syndrome causes disability in the form of weakness of the lower extremities and involvement of bowel or bladder, and problems with ambulation, but it cannot be a direct cause of death, though in patients with chronic sequelae of cauda equina complications like deep vein thrombosis causing pulmonary embolism, urinary tract infection causing sepsis pulmonary infection or respiratory failure may be secondary cause of death in such patients.
Can you get cauda equina syndrome twice?
Cauda equina syndrome in itself is a rare entity and to get it twice is rarer, though not impossible. Patients who are predisposed to cauda equina syndrome like those with malignancy or metastasis or those with blood disorder and are on anticoagulants may rarely have cauda equina syndrome twice too.
Is cauda equina syndrome permanent?
An acute presentation of cauda equina syndrome if treated appropriately can lead to good recovery, but if not treated appropriately or in patients with chronic cauda equina, the sequelae of cauda equina syndrome may be long lasting or permanent too.
Can you get cauda equina syndrome with fusion surgery?
Any surgery on lumbar spine carries a risk of cauda equina syndrome. This can happen due to any bleeding at the surgical site, which leads to hematoma formation and compression of the nerve roots causing the presentation of cauda equina syndrome. These patients need to be treated urgently with decompression and need to be carefully followed up.
How to avoid or prevent cauda equina syndrome?
As the cauda equina syndrome and itself is a rare entity, there is no possible way to prevent a cauda equina syndrome. Patients who are on anticoagulants carry a higher risk of cauda equina syndrome, but the benefits of anticoagulant therapy far outweighs the risk of cauda equina syndrome or any other such bleeding complication. Similarly patient with metastases are at increased risk of cauda equina syndrome and their tumor is appropriately treated with chemo or radiotherapy, but prophylactic treatment with the surgery or radio or chemotherapy just to prevent cauda equina syndrome is not advisable.

