If you have been experiencing neck pain or other issues related to your cervical spine, your doctor might suggest surgery as a potential solution. There are two primary surgical approaches to address problems in the cervical spine: anterior cervical surgery and posterior cervical surgery. Understanding the differences between these procedures, their benefits, and potential risks can help you make an informed decision about your treatment.
Sometimes, it is a difficult question for the patient and even for the surgeon to decide if the patient needs surgery from the front or the back of the neck. There are multiple factors that help in the decision making of the approach to the neck.
The location of the pathology has a considerable effect on the decision making of the approach. If the pathology is located in the front of the neck then going from the front may be a better option and vise versa.
Also, the number of levels involved as well as the time of disease process on its natural history timeline helps in understanding and deciding the approach. Patients who have wear and tear over multiple segments can be better treated from the back of the neck.
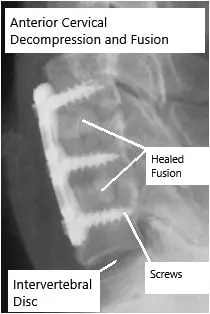
Healed and fused Anterior Cervical Decompression and Fusion.
The contour or the posture of the neck also is important. The patients who have lost their normal contour are not a good candidate from the surgery from the back of the neck. These patients are at a high risk of further worsening of the contour if surgery is done from the back. Surgery from the front of the neck can help regain the posture back to normal or near normal.
Patients who have significant neck pain are a candidate for fusion surgery, which can be done either from the front or the back of the neck. Patients who do not have significant neck pain can be a good candidate for non-fusion surgery, which includes laminoplasty for cervical spondylotic myelopathy or foraminotomy for nerve root pain or radiculopathy. Both of these surgeries are done from the back of the neck.
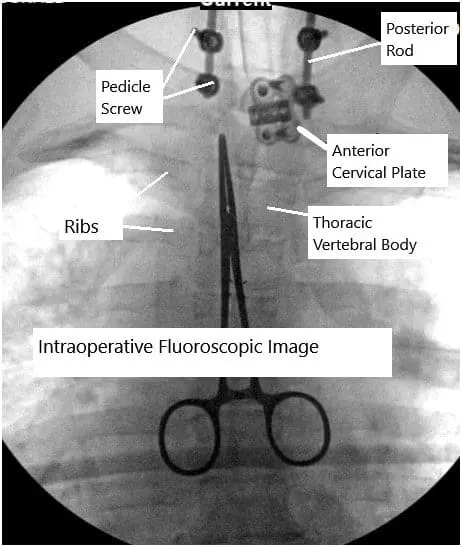
Combined anterior and posterior cervical spine surgery.
Anterior Cervical Surgery
What Is It?
Anterior cervical surgery involves accessing the cervical spine from the front (anterior) of the neck. This approach is often used for procedures like anterior cervical discectomy and fusion (ACDF) and cervical disc replacement.
Procedure Overview
Incision: A small incision is made in the front of the neck.
Accessing the Spine: The surgeon gently moves aside the muscles and tissues to reach the cervical spine.
Removing the Problem: If you have a herniated disc or bone spurs, these are removed to relieve pressure on the spinal cord or nerves.
Stabilization: The surgeon might insert a bone graft and a metal plate with screws to stabilize the spine. In the case of disc replacement, an artificial disc is used instead of a bone graft.
Benefits
- Less Postoperative Pain: Accessing the spine from the front often causes less disruption to muscles, resulting in less pain after surgery.
- Better Alignment: This approach allows the surgeon to better restore the alignment of the cervical spine.
- Quicker Recovery: Many patients experience a quicker recovery and return to normal activities.
Risks
- Throat Discomfort: Temporary discomfort in the throat and difficulty swallowing can occur.
- Voice Changes: Rarely, there can be changes in the voice due to the proximity of the vocal cords.
- Infection and Bleeding: As with any surgery, there are risks of infection and bleeding.
Click on Cervical Corpectomy and Cervical Discectomy and Fusion for procedure and cost information.
Posterior Cervical Surgery
What Is It?
Posterior cervical surgery involves accessing the cervical spine from the back (posterior) of the neck. This approach is commonly used for procedures like laminectomy, foraminotomy, and posterior cervical fusion.
Procedure Overview
Incision: A small incision is made in the back of the neck.
Accessing the Spine: The surgeon moves the muscles and tissues to reach the vertebrae and spinal cord.
Removing the Problem: If there is pressure on the spinal cord or nerves, bone and ligament tissue may be removed to relieve this pressure.
Stabilization: Similar to anterior surgery, a bone graft and metal hardware might be used to stabilize the spine if necessary.
Benefits
- Addressing Spinal Stenosis: This approach is particularly effective for treating spinal stenosis by directly relieving pressure on the spinal cord.
- Wider Access: It provides a wider access area for the surgeon to address multiple levels of the spine if needed.
- Flexibility: Posterior surgery can be tailored to address specific issues such as removing tumors or cysts.
Risks
- Muscle Pain: Since the muscles in the back of the neck are moved, there can be more postoperative muscle pain.
- Longer Recovery: Recovery might take longer compared to anterior surgery due to the greater disruption of muscles.
- Infection and Bleeding: Similar to anterior surgery, there are risks of infection and bleeding.
Click on Cervical Laminoplasty for procedure and cost information.
Other Differences between Anterior and Posterior Cervical Surgery
The results from a surgery done either from the front or the back of the neck not only depends on the approach but also depends on the type of pathology and its expected results. The approaches do differ in recovery as well as complications.
Patients who undergo surgery from front recover faster as compared to one who gets surgery from the back of the neck. The wound healing may be delayed with the higher incidence of infection in surgeries, which are performed from the back of the neck. Patients may have neck pain or loss of neck contour after surgery from the back of the neck.
Occasionally, the patient may need support on the neck from both sides and may have to undergo surgeries from the back as well as the front of the neck. A thorough discussion between the patient and the physician about the disease process, the anatomy of the neck, symptoms, and expectations is helpful in making a decision regarding the type of surgery as well the approach being from the front or the back of the neck.
Decision Making: Anterior Cervical Vs Posterior Cervical Surgery
As in most other situations the decision making between an approach from the front or the back is not straightforward and there are multiple variables in play.
It is not just the surgical approach being from the front of the neck or from the back of the neck that decides the result of the surgery. Surgical results also depend on the disease process as well as its presentation, severity, associated symptoms, natural history of the disease and expected results.
In a usual most common presentation of cervical radiculopathy that is pain with tingling or numbness going down into one arm, the approach depends on the condition of the disc.
If the disc is in good condition then a minimal invasive posterior non-fusion approach can give good results with minimal long term effects. This approach includes relieving the pressure from the nerve root, which is being compressed by the disk material and the process is called microdiscectomy and foraminotomy.
If the disc is degenerated and the patient has no neck pain then they can be a good candidate for Total Disc replacement arthroplasty. In this surgery, the natural diseased disc is replaced by an artificial disc. This allows us to restore normal functionality of the disc and at the same time taking care of the disease process.
If the patient has neck pain also and has a diseased disc, then a procedure from the front involving removal of the disk followed by fusion surgery may be more beneficial. The surgery involves replacing the disk with the cage and graft material, supplemented with a plate. This allows us to take care of the pathology and the disk to fuse. The surgery is called Anterior Discectomy and Fusion (ACDF).
Patients with radiculopathy can usually be treated with either of the above mentioned surgery.
Some patients may present with myelopathy, which means weakness of the arms and/or legs with issues with balance, dexterity and/or bowel and bladder function. These patients can be treated either from the front or the back depending on the number of levels involved, contour of the neck, presentation etc.
Overall patients with bad neck contour are preferably operated from the front while those with good contour can be treated from either side. Patients with one or two level involvement can be treated with Disc replacement arthroplasty from the front. All attempts are made to do a surgery from the front, so as to restore the anatomy as well as allow decompression of the nerve roots and the spinal cord.
Patients with weakness associated neck pain are preferably treated with fusion surgery rather than non fusion surgery like disc replacement or laminoplasty.
Patients with weakness, multilevel involvements and good neck contour are better treated from the back. If they do not have neck pain, avoiding fusion by doing a motion sparing surgery called Laminoplasty can give good results.
If the patient has weakness, neck pain along with multilevel involvement then fusion with an approach from the back of the neck will give better results. This surgery involves removing the back of the vertebra and fusing them with screws and rods at multiple levels. The surgery is called Laminectomy and Posterior Cervical Fusion.
Patients who present early in the course and have not responded to conservative means respond very well to surgical treatment.
Patients who are late in the course of disease and already have weakness with or without involvement of bowel, bladder or gait, balance may have incomplete recovery from the surgery.
Surgery in such patients is directed towards stopping further progression of the disease and further neurological deficit by optimizing the condition of the spinal cord and nerve root. Recovery is expected, though not complete and is not guaranteed.
Comparing Anterior and Posterior Approaches
Choosing the Right Approach
The choice between anterior and posterior cervical surgery depends on several factors, including the specific condition being treated, the location of the issue within the cervical spine, and the patient’s overall health and anatomy. Your surgeon will evaluate these factors and recommend the best approach for your situation.
Effectiveness
Both anterior and posterior surgeries are effective in relieving symptoms and improving the quality of life for patients with cervical spine issues. Studies have shown that both approaches can provide significant pain relief and improve function. The effectiveness of the surgery largely depends on the precise nature of the spinal problem and the skill of the surgeon.
Recovery Time
- Anterior Surgery: Generally, recovery is quicker due to less muscle disruption. Patients often experience less postoperative pain and can return to normal activities sooner.
- Posterior Surgery: Recovery might be longer because the surgery involves moving more muscle tissue. However, this approach can be more effective for certain conditions, such as extensive spinal stenosis.
Complications
- Anterior Surgery: Complications can include throat discomfort, difficulty swallowing, and voice changes. These are usually temporary and resolve as the patient heals.
- Posterior Surgery: Complications can include more significant muscle pain and a longer recovery period. As with any surgery, there are risks of infection and bleeding.
Do you have more questions?
What are the main differences between anterior and posterior cervical surgery?
Anterior cervical surgery involves accessing the spine from the front of the neck, typically for conditions like herniated discs or degenerative disc disease. Posterior cervical surgery accesses the spine from the back of the neck, often used for treating spinal stenosis or more complex multi-level issues.
Which approach, anterior or posterior, has a quicker recovery time?
Generally, anterior cervical surgery has a quicker recovery time due to less muscle disruption compared to posterior surgery.
Are there different risks associated with anterior versus posterior cervical surgery?
Yes, anterior surgery risks include throat discomfort, difficulty swallowing, and voice changes, while posterior surgery risks include greater muscle pain and a potentially longer recovery period.
How does the incision location differ between anterior and posterior cervical surgery?
Anterior cervical surgery involves an incision in the front of the neck, while posterior cervical surgery involves an incision in the back of the neck.
Which surgery approach is more effective for treating spinal stenosis?
Posterior cervical surgery is generally more effective for treating spinal stenosis as it provides a broader access area to relieve pressure on the spinal cord.
What type of pain relief can be expected from anterior cervical surgery compared to posterior cervical surgery?
Both surgeries provide significant pain relief, but anterior surgery typically results in less postoperative pain due to less muscle disruption.
Which approach allows for better spinal alignment restoration?
Anterior cervical surgery allows for better restoration of spinal alignment because it provides direct access to the vertebral bodies and discs.
Can both anterior and posterior cervical surgeries be performed using minimally invasive techniques?
Yes, both approaches can utilize minimally invasive techniques, which can reduce recovery time and postoperative pain.
How does the surgeon decide between anterior and posterior cervical surgery?
The decision is based on the specific condition being treated, its location, the patient’s overall health, and the potential benefits and risks of each approach.
Are there differences in the type of hardware used in anterior versus posterior cervical surgery?
Yes, anterior surgery often uses a bone graft and metal plate with screws, while posterior surgery may use rods, screws, and bone grafts to stabilize the spine.
Which approach is more suitable for multi-level spinal issues?
Posterior cervical surgery is often more suitable for multi-level spinal issues as it provides broader access to multiple levels of the spine.
What are the potential complications unique to posterior cervical surgery?
Potential complications include increased muscle pain, a longer recovery period, and a higher risk of infection due to the larger incision and muscle disruption.
How does the surgical approach impact the length of the hospital stay?
Anterior cervical surgery typically results in a shorter hospital stay compared to posterior surgery, due to less postoperative pain and quicker recovery.
Can both approaches address issues like herniated discs and degenerative disc disease?
Yes, both approaches can address these issues, but anterior surgery is more commonly used for herniated discs and degenerative disc disease, while posterior surgery is used for more complex cases.
How does each approach affect postoperative mobility?
Anterior surgery generally allows for quicker return to normal activities due to less muscle disruption, while posterior surgery might require a longer period of restricted movement.
What is the difference in scar visibility between anterior and posterior cervical surgery?
Anterior cervical surgery typically leaves a small, less visible scar on the front of the neck, whereas posterior surgery leaves a scar on the back of the neck, which may be more noticeable depending on the incision size and healing.
Are there differences in how pain is managed postoperatively between the two approaches?
Pain management is similar but might be more intensive for posterior surgery due to greater muscle disruption. Both approaches use medications, physical therapy, and non-pharmacological methods for pain relief.
How does each approach impact the risk of needing additional surgeries in the future?
Both approaches have similar long-term success rates, but the choice of surgery should be tailored to the specific condition and patient needs to minimize the risk of future surgeries.
What role does patient anatomy play in choosing between anterior and posterior cervical surgery?
Patient anatomy, such as the location and severity of the spinal issue, overall health, and specific anatomical considerations, significantly influences the choice of surgical approach.
How do anterior and posterior approaches differ in terms of addressing nerve compression?
Anterior surgery is typically more effective for directly decompressing nerves affected by herniated discs or bone spurs, while posterior surgery is often used to decompress the spinal cord and nerve roots in cases of spinal stenosis.
Are there specific conditions that are exclusively treated with one approach over the other?
Conditions like severe spinal stenosis or multi-level spondylosis are more often treated with posterior surgery, while isolated herniated discs or single-level degenerative disc disease are frequently addressed with anterior surgery.
How does each surgical approach impact postoperative physical therapy requirements?
Both approaches require physical therapy, but patients who undergo posterior surgery might need a more extended physical therapy regimen due to greater muscle involvement.
Can both anterior and posterior surgeries be performed as outpatient procedures?
Some minimally invasive anterior surgeries can be performed as outpatient procedures, while posterior surgeries typically require a short hospital stay due to the more extensive nature of the procedure.
How do the rates of surgical success compare between anterior and posterior approaches?
Both approaches have high success rates when performed for the appropriate indications, with success largely dependent on the specific condition being treated and the surgeon’s expertise.
What advancements are being made to improve outcomes for anterior and posterior cervical surgeries?
Advancements include the development of minimally invasive techniques, better imaging for surgical planning, customized implants, and enhanced postoperative care protocols to improve outcomes and reduce complications for both anterior and posterior cervical surgeries.

