Cervical laminoplasty is one of the newer and novel surgical procedures done on the neck for Cervical Spondylotic Myelopathy. This surgery is performed from the back of the neck.
This surgery is done in patients who have weakness due to compression of the spinal cord in the neck. Laminoplasty is a non-fusion surgery, which means that it does not lead to restriction of movement of the neck as opposed to fusion surgeries that cause restriction of the movement of the neck. It gives excellent results in appropriately chosen patients.
Indications Cervical Laminoplasty is performed in patients who have spinal cord compression at multiple levels in the neck. These patients may have compression of the spinal cord due to wear and tear and aging changes. Some patients may also have underlying cervical spine stenosis These patients with stenosis have a smaller diameter of the spinal canal.
Patients with congenital spinal canal stenosis are at higher risk of developing spinal cord compression and its subsequent complications. An ideal patient for laminoplasty is one who does not have any neck pain or any pain going down into the arm (cervical radiculopathy). These patients have a good contour of their neck (Cervical Lordosis) and are not found to have any gross instability of the neck.
Prior imaging of the neck and sometimes the whole spine is done before the surgical treatment is planned. X-rays, MRI, and CT scans are performed to find the right candidate as well as do good surgical planning. Occasionally, the patient may have to undergo EMG and nerve conduction study before surgery to confirm the diagnosis. These patients usually have weakness in their legs, which manifests in the form of gait problems and imbalance. These patients may also have weakness in their hand and upper extremity.
Occasionally, thereby the patients who have more weakness in their upper extremity than their lower extremity as is the presentation of central cord syndrome. Patients who have pain in one or both upper extremities only are not a good candidate for the surgery. Also, patients who have an inflammatory disease of their neck including ankylosing spondylitis or rheumatoid arthritis are not good candidates for this type of surgery.
Patients who have weakness along with pain in one or both arm can be a candidate for the surgery along with decompression of their nerve root, which can be done at the same time.
Cervical Laminoplasty Operative Technique
Laminoplasty is done under general anesthesia and an endotracheal tube is passed into the patient’s windpipe to maintain the ventilation during the surgery. We also use spinal cord monitoring by the use of electrodes and monitoring the sensory and motor functions of the nerves during the surgery. This helps in knowing if something is going bad with the nerve or the spinal cord during the surgery and helps us do the procedure safely.
Patient is positioned prone on their belly on the operating table and their head is fixed. The hairs from the back of the head are shaved. The shoulders are taped to the bed. We use intraoperative imaging to confirm our levels and treatment.
The surgical incision is given in the midline on the back of the neck and the back of the spine is exposed with meticulous dissection and control of bleeding. This surgery involves opening up the spinal canal from the back thereby giving space for the spinal cord and relieving the compression from the spinal cord.
The compression is usually from the front of the spinal cord. In patients who have a good neck contour, the surgery allows the spinal cord to move back. This drifting of the spinal cord towards the back relieves it off the pressure.To open the spinal canal, the lamina of the back of the spine is cut sequentially over multiple levels on one side.
This cut is through-and-through into the spinal canal. A similar cut is made on the lamina on the other side but is not through-and-through. This allows hinging the spinous process onto another side of lamina. Once the hinging is done, the spinal canal opens on the one side.
This opening is kept in place by the use of plate and screws. Many plates and screws can be used in the fixation. This opening of the canal allows the spinal cord to drift back and relieve its pressure.
Once it is done, the spinal cord is meticulously examined and all the bleeding is controlled. If the patient has radicular pain also then foraminotomy to relieve the pressure from the nerve root can also be performed at the same time. The incision is closed.
We regularly use vancomycin antibiotic powder to prevent infection and allow good healing. Patients are put in a cervical collar for a couple of weeks for comfort.
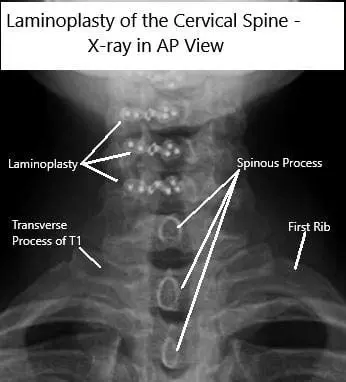
AP and Lateral view X rays of Laminoplasty C3-6
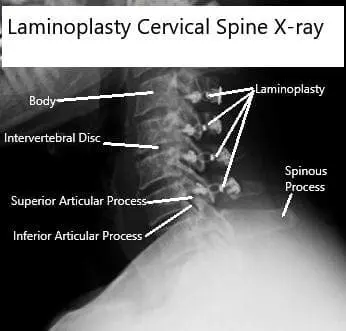
AP and Lateral view X rays of Laminoplasty C3-6
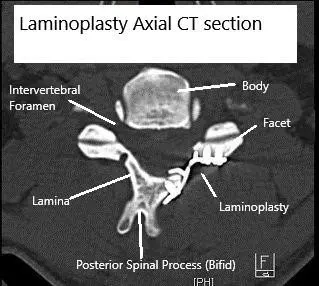
Axial CT scan Post-op Laminoplasty
Benefits and Risks
One of the primary benefits of cervical laminoplasty is the relief from symptoms like pain, numbness, and weakness, thereby improving quality of life. Unlike procedures that fuse the vertebrae together, laminoplasty preserves the natural movement of the spine, which is significant for maintaining mobility.
However, like any surgery, laminoplasty comes with risks. These include bleeding, infection, nerve damage, and in rare cases, spinal cord injury. Long-term complications might include loss of spinal alignment, kyphosis (forward curvature of the spine), recurrent stenosis, and lordosis (inward curvature of the spine).
Cervical Laminoplasty Recovery
Carefully selected patients who undergo laminoplasty do well after the surgery. They recover gradually over a period of time. Occasionally, they may have to go to rehab especially if their activities are grossly limited due to their disease process. Laminoplasty allows the patient to retain and recover there range of motion.
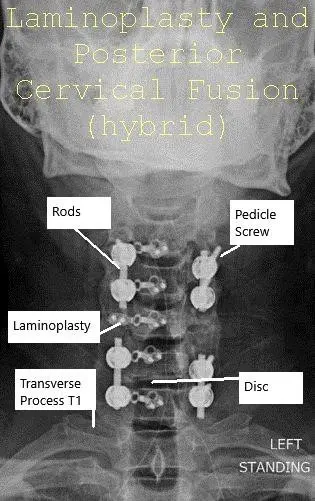
AP and Lateral view X-ray Post-op Laminoplasty and Posterior Spinal Fusion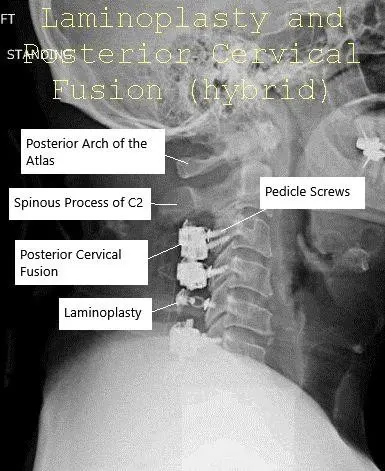
AP and Lateral view X-ray Post-op Laminoplasty and Posterior Spinal Fusion
Alternative Surgical Options
If cervical laminoplasty is not suitable, other surgical options are available. A laminectomy involves removing the lamina to decompress the spinal cord but often requires spinal fusion, limiting mobility. A laminotomy, on the other hand, involves making a small hole in the lamina to relieve pressure without removing the entire structure.
Another option is an anterior cervical discectomy and fusion (ACDF), which is performed through the front of the neck and involves fusing the vertebrae. Total disc replacement (TDR) is also an option, aiming to preserve spinal motion by replacing the damaged disc with an artificial one.
Long-Term Outlook
The success rate of cervical laminoplasty is promising, with studies showing that up to 70% of patients experience long-term relief from their symptoms. The outcome of the surgery depends on factors such as the patient’s overall health, age, the extent of spinal cord compression, and how long symptoms were present before surgery.
Out-of-Pocket Costs
Medicare
CPT Code 63051 – Cervical Laminoplasty: $411.04
Under Medicare, 80% of the approved amount for this procedure is covered after meeting the annual deductible. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans, such as Medigap, AARP, or Blue Cross Blue Shield, generally cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved cervical spine surgeries like laminoplasty. These supplemental plans coordinate directly with Medicare to provide full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it functions as a secondary payer after Medicare processes the claim. Once your deductible is satisfied, the secondary plan may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, ranging from $100 to $300, depending on the specific policy and network status.
Workers’ Compensation
If your cervical spine condition requiring laminoplasty resulted from a work-related injury, Workers’ Compensation will cover all related medical and surgical costs, including the laminoplasty procedure. You will have no out-of-pocket expenses under an approved Workers’ Compensation claim.
No-Fault Insurance
If your cervical spine injury requiring laminoplasty resulted from a motor vehicle accident, No-Fault Insurance will pay for all related surgical and hospital expenses. The only potential out-of-pocket cost may be a small deductible, depending on the terms of your insurance policy.
Example
Susan, a 64-year-old patient with cervical myelopathy due to spinal stenosis, underwent cervical laminoplasty (CPT 63051). Her estimated Medicare out-of-pocket cost was $411.04. Since she had supplemental insurance through AARP Medigap, the 20% that Medicare did not cover was fully paid, leaving her with no out-of-pocket expense for the procedure.
Frequently Asked Questions (FAQ)
Q. What are the advantages of cervical laminoplasty over other procedures?
A. Cervical laminoplasty is a non-fusion surgery that preserves neck mobility, unlike fusion surgeries that restrict movement. It provides significant relief from symptoms without permanently altering the anatomy of the spine.
Q. How long does it take to recover from cervical laminoplasty?
A. Recovery typically takes several months, with most patients returning to normal activities within 6 to 12 weeks. Physical therapy may be required for optimal recovery.
Summary and Takeaway
Cervical laminoplasty is an effective, non-fusion procedure for treating cervical spondylotic myelopathy, offering significant symptom relief while preserving neck movement. It is ideal for patients with multi-level spinal cord compression without significant neck pain. As with any surgery, the procedure carries risks, but the prognosis is generally favorable, especially in carefully selected patients.
Clinical Insight & Recent Findings
A recent study explored the connection between muscle degeneration in the neck (known as sarcopenia) and the development of kyphosis (a curvature in the spine) after cervical laminoplasty surgery. The study found that patients with more fatty infiltration in their cervical paraspinal muscles before surgery were at a higher risk of developing kyphosis after the procedure.
Using both qualitative and quantitative methods to measure fat in the muscles, the research revealed that a fat percentage greater than 23% in the muscles was linked to a higher chance of kyphosis. This suggests that muscle health plays an important role in surgical outcomes and can help predict post-surgery complications.
However, other factors like age and spinal condition may also influence the results. The study emphasizes the need for further research to confirm these findings and improve preoperative assessments. (“Study on cervical paraspinal muscle fatty degeneration and kyphosis – See PubMed”)
Who Performs This Treatment? (Specialists and Team Involved)
Cervical laminoplasty is typically performed by spine surgeons, which may include orthopedic surgeons or neurosurgeons specializing in cervical spine surgery. The surgical team may also include anesthesiologists, nurses, and physical therapists who assist in the recovery process.
When to See a Specialist?
If you experience symptoms such as weakness, numbness, or difficulty with balance and coordination that do not improve with conservative treatment, it is time to consult a spine specialist.
When to Go to the Emergency Room?
If you experience sudden loss of strength, difficulty breathing, or loss of bowel or bladder control, these may be signs of a spinal emergency and you should seek immediate medical attention.
What Recovery Really Looks Like?
Recovery after cervical laminoplasty is gradual, with patients typically experiencing significant relief from their symptoms within a few months. Physical therapy is often recommended to help restore strength and flexibility in the neck and upper limbs.
What Happens If You Ignore It?
Ignoring symptoms of cervical spondylotic myelopathy can lead to permanent nerve damage, difficulty walking, and worsening balance issues. Early surgical intervention can prevent further progression and improve quality of life.
How to Prevent It?
Maintaining good posture, engaging in neck-strengthening exercises, and avoiding activities that strain the cervical spine can help prevent degenerative changes. Regular check-ups with a healthcare provider can also help identify issues early before they require surgery.
Nutrition and Bone or Joint Health
Adequate intake of calcium and vitamin D is crucial for bone health, which is essential for maintaining a strong and healthy cervical spine. A well-balanced diet rich in these nutrients can help prevent spinal degeneration.
Activity and Lifestyle Modifications
Post-surgery, patients should focus on gentle, low-impact activities that promote neck mobility and overall strength. Avoid heavy lifting and high-impact activities until cleared by a healthcare provider.
Do you have more questions?
What is the typical recovery time after cervical laminoplasty?
Recovery time varies, but most patients can expect to return to light activities within a few weeks. Full recovery, including return to work and more strenuous activities, generally takes between 2 to 8 weeks, depending on the individual and the nature of their work
Will I need physical therapy after cervical laminoplasty?
Yes, physical therapy is often recommended after cervical laminoplasty to help strengthen the neck muscles, improve mobility, and ensure proper healing
How long will I need to wear a cervical collar after surgery?
The duration of wearing a cervical collar varies. It could be a few days to several weeks, depending on your specific case and your surgeon’s recommendations
What kind of pain management can I expect post-surgery?
Pain management typically involves oral medications, including painkillers and muscle relaxants. NSAIDs are usually avoided for the first six weeks to not impede the healing process
Are there any dietary restrictions post-surgery?
There are no specific dietary restrictions, but staying hydrated and consuming a balanced diet rich in vitamins and minerals can aid in recovery. Avoid alcohol and tobacco as they can hinder healing
Can cervical laminoplasty be performed on patients with advanced arthritis?
Cervical laminoplasty may not be suitable for patients with advanced arthritis where there is minimal motion left in the spine. Other surgical options might be more appropriate in such cases
How is cervical laminoplasty different from other spinal surgeries like laminectomy or discectomy?
Cervical laminoplasty reshapes the lamina to relieve pressure while preserving spinal motion. Laminectomy involves removing the lamina, often leading to spinal fusion, while discectomy involves removing a herniated disc
What are the signs of infection I should look out for after surgery?
Signs of infection include redness, swelling, warmth, and drainage from the incision site, as well as fever. Contact your healthcare provider immediately if you notice these symptoms
Is cervical laminoplasty a permanent solution for spinal stenosis?
While cervical laminoplasty can provide long-term relief, it may not be a permanent solution for everyone. Some patients may experience recurring symptoms or complications over time
Can cervical laminoplasty improve my range of motion?
Cervical laminoplasty aims to preserve your current range of motion rather than improve it. It prevents further loss of motion by avoiding spinal fusion
How soon after surgery can I resume driving?
You should avoid driving until your follow-up visit and you are no longer taking narcotic pain medications. Your ability to turn your head sufficiently to drive safely is also a factor
What types of activities should I avoid during recovery?
Avoid lifting anything heavier than 10 pounds, pushing, pulling, and strenuous activities. Gradually increase walking as it is beneficial for recovery
How long will I stay in the hospital after the procedure?
Hospital stays typically range from 1 to 2 nights, depending on your recovery progress and any complications that may arise
Are there long-term complications associated with cervical laminoplasty?
Long-term complications are rare but can include loss of spinal alignment, kyphosis, recurrent stenosis, and lordosis
Will cervical laminoplasty cure my neck pain completely?
While many patients experience significant relief from symptoms, there is no guarantee that pain will be completely eliminated. Success rates vary, and some patients may have residual pain
What is the success rate of cervical laminoplasty?
Success rates are quite good, with up to 70% of patients experiencing relief from symptoms for up to 10 years post-surgery. Individual results vary based on several factors
Can I engage in sports after recovering from cervical laminoplasty?
Once fully recovered and cleared by your surgeon, you may be able to return to some sports. However, activities that put significant strain on the neck should be avoided or approached with caution
Will I have a visible scar after cervical laminoplasty?
The incision is typically made in the back of the neck, and while there will be a scar, it usually fades over time. Proper incision care can help minimize its appearance
How does the surgeon decide between the open door and French door techniques?
The choice of technique depends on the specific anatomy and condition of your spine. Your surgeon will choose the method that offers the best outcome for your situation
Are there any non-surgical alternatives to cervical laminoplasty?
Non-surgical options include physical therapy, medications, and epidural steroid injections. These can be effective for managing symptoms but may not address the underlying cause as effectively as surgery
What happens if the laminoplasty doesn't relieve my symptoms?
If symptoms persist after surgery, further evaluation is necessary. Additional treatments, including other surgical options or revision surgeries, might be considered
How should I care for my incision after surgery?
Keep the incision clean and dry, inspect it daily for signs of infection, and follow your surgeon’s instructions on changing dressings and using any prescribed ointments or medications
Can cervical laminoplasty be done as an outpatient procedure?
Cervical laminoplasty is typically performed as an inpatient procedure, requiring a hospital stay of 1 to 2 nights for monitoring and initial recovery
How does my general health affect the outcome of cervical laminoplasty?
Your general health, including factors like age, overall fitness, and the presence of other medical conditions, can significantly affect your recovery and the overall success of the surgery

