Cervical Degenerative Disc Disease (DDD) refers to gradual wear and tear of the discs and joints in the neck. As we age, the spinal discs lose water and elasticity, becoming thinner and less able to cushion the vertebrae. These changes can lead to pain, stiffness, and, in some cases, nerve compression that affects the arms or hands.
How Common It Is and Who Gets It? (Epidemiology)
Degenerative disc disease is one of the most common causes of neck pain in adults over 40. The most frequently affected areas are the middle and lower parts of the cervical spine—especially the C5–C6 and C6–C7 levels. Age, genetics, occupation, smoking, and prior neck injury all influence how quickly degeneration progresses. Men and women are affected equally.
Why It Happens – Causes (Etiology and Pathophysiology)
As discs lose water with age, they shrink and crack, placing more stress on nearby joints and ligaments. Repetitive motion, poor posture, or trauma such as whiplash can speed up this process. Chronic conditions like rheumatoid arthritis may also accelerate degeneration.
The body sometimes responds by forming bone spurs (osteophytes) to stabilize the area, but these spurs can narrow the spinal canal or pinch nerves.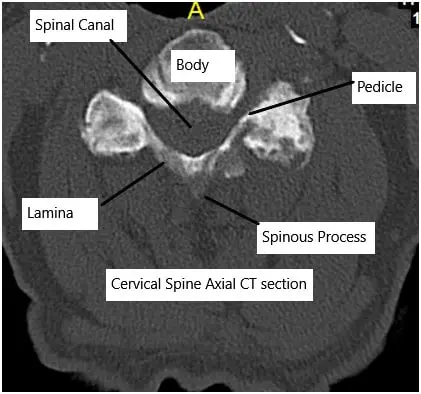
Cervical CT scan showing axial section.
How the Body Part Normally Works? (Relevant Anatomy)
The cervical spine has seven vertebrae separated by discs that act as cushions. Each disc has a tough outer ring (annulus fibrosus) and a gel-like center (nucleus pulposus). These structures allow flexibility and absorb shock. Nerves travel through openings in the vertebrae to the arms and upper body.
When a disc weakens or collapses, space for the nerves decreases, leading to irritation or compression.
What You Might Feel – Symptoms (Clinical Presentation)
Many people with cervical disc degeneration never develop symptoms. When symptoms occur, they may include:
- Neck pain or stiffness that worsens with movement
- Radiating pain to the shoulder, arm, or upper back
- Tingling, numbness, or weakness in the arms or hands
- Headaches at the base of the skull
- In severe cases, unsteady gait, clumsiness, or bladder changes due to spinal cord compression
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a physical exam to check range of motion, reflexes, and strength.
Imaging tests include:
- X-rays to evaluate disc space narrowing or bone spurs
- MRI to visualize discs, nerves, and spinal cord compression
- CT scans to detail bone changes or calcified ligaments
- Electrodiagnostic tests (EMG/NCS) if nerve involvement is unclear
Classification
Cervical DDD can be described by location and severity:
- Mild: Disc height loss with occasional neck pain
- Moderate: Disc herniation or bone spurs causing nerve irritation
- Severe: Multi-level degeneration with spinal cord compression (cervical stenosis)
Other Problems That Can Feel Similar (Differential Diagnosis)
Neck pain may also result from:
- Muscle strain or whiplash injury
- Cervical facet joint arthritis
- Herniated disc without degeneration
- Spinal tumors or infections
- Shoulder or upper-back disorders
Treatment Options
Non-Surgical Care
Most patients improve without surgery. Common treatments include:
- Medications: Anti-inflammatory drugs, pain relievers, or muscle relaxants.
- Physical therapy: Stretching and strengthening exercises to stabilize neck muscles.
- Activity modification: Ergonomic adjustments, posture correction, and regular breaks from prolonged sitting.
- Cervical collar: Short-term use for acute pain relief.
- Injections: Corticosteroid injections to reduce inflammation.
Surgical Care
Surgery is recommended for persistent pain, nerve compression, or spinal cord involvement that does not improve with conservative care. Options include:
- Anterior Cervical Discectomy and Fusion (ACDF): Removal of the diseased disc through the front of the neck followed by fusion of the adjacent bones.
- Cervical Disc Replacement (Arthroplasty): Replacement of the damaged disc with an artificial one to preserve motion.
- Posterior Foraminotomy: Minimally invasive decompression through the back of the neck without fusion.
- Posterior Laminectomy and Fusion / Laminoplasty: Used for multi-level disease or spinal cord compression.
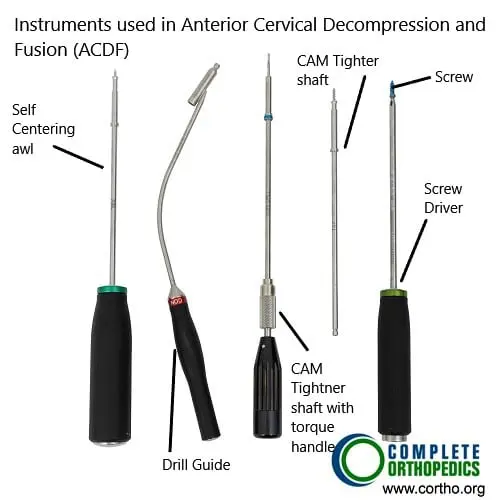
Instruments used in ACDF
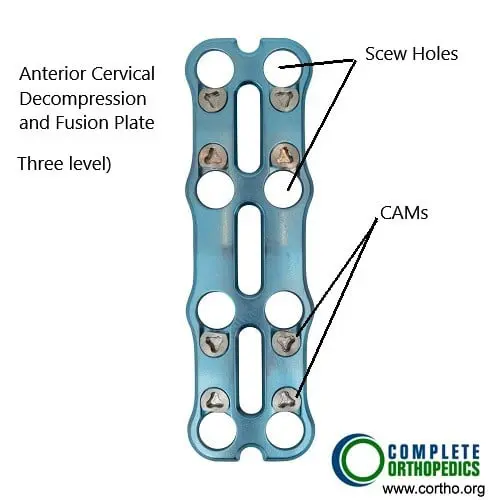
ACDF Plate (3 level fusion)
The images above show ACDF (anterior cervical decompression and fusion) plate and instruments used to fuse the cervical vertebrae from the front of the neck. The surgery helps to decompress the spinal nerves/spinal cord and prevent movement between the segments to alleviate the symptoms and achieve stability.
Recovery and What to Expect After Treatment
- Conservative therapy: Most patients recover in 4–6 weeks with rest, exercise, and medication.
- After surgery: Hospital stay is usually 1–2 days. Return to light activity occurs within a few weeks; full recovery may take 2–3 months.
Patients with spinal cord compression may take longer to recover and may need ongoing rehabilitation.
Possible Risks or Side Effects (Complications)
Potential surgical risks include:
- Infection, bleeding, or nerve injury
- Failure of fusion or implant loosening
- Difficulty swallowing or hoarseness (temporary)
- Blood clots or anesthesia complications
- Persistent pain or stiffness
Patients with diabetes, obesity, or smoking history have higher complication risks.
Long-Term Outlook (Prognosis)
Most patients achieve lasting pain relief and improved mobility after treatment. Surgery generally prevents further nerve damage, though mild stiffness may remain. Early diagnosis and good postoperative care yield the best outcomes.
Out-of-Pocket Costs
Medicare
CPT Code 22551 – Anterior Cervical Discectomy and Fusion (ACDF): $417.50
CPT Code 22856 – Cervical Disc Replacement (Arthroplasty): $396.11
CPT Code 63020 – Posterior Foraminotomy: $271.49
CPT Code 63045 + 22600 – Posterior Laminectomy and Fusion: $319.26 + $322.92
CPT Code 63050 – Laminoplasty: $362.34
Under Medicare, the program typically covers 80% of the approved cost for these procedures once the deductible is met. Patients are responsible for the remaining 20%, which can be completely covered by supplemental insurance such as Medigap, AARP, or Blue Cross Blue Shield. These supplemental plans coordinate directly with Medicare, ensuring that for approved cervical spine surgeries, patients often pay little to no out-of-pocket cost.
If you carry secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA) benefits—it acts as a secondary payer after Medicare has processed the claim. Once your deductible has been satisfied, the secondary plan can cover remaining balances, including co-insurance or uncovered costs. These plans may include a small deductible, generally ranging between $100 and $300 depending on the specific policy and network coverage.
Workers’ Compensation
If your cervical disc degeneration or related spinal injury occurred as a result of work activity, Workers’ Compensation will cover the full cost of treatment, including ACDF, disc replacement, foraminotomy, or fusion procedures. All associated hospital and rehabilitation costs are included, and you will have no out-of-pocket expenses under an accepted claim.
No-Fault Insurance
If your cervical disc disease or injury was caused or worsened by an automobile accident, No-Fault Insurance will pay for all medically necessary treatments, including decompression, disc replacement, or fusion procedures. The only potential charge is a small deductible, depending on the details of your insurance policy.
Example
Linda, a 57-year-old office professional, was diagnosed with cervical disc degeneration that caused neck pain and arm numbness. She underwent a single-level anterior cervical discectomy and fusion (ACDF) with an estimated Medicare out-of-pocket cost of $417.50. Her supplemental Medigap plan covered the 20% that Medicare did not pay, leaving her with no out-of-pocket expense for the surgery.
Frequently Asked Questions (FAQ)
Q. Is cervical degenerative disc disease part of aging?
A. Yes. Disc wear is a normal part of aging, though not everyone develops symptoms.
Q. Can it be reversed?
A. No, but symptoms can be controlled through exercise, therapy, and lifestyle changes.
Q. When is surgery needed?
A. When pain, weakness, or numbness persist after several weeks of non-surgical treatment or if spinal cord compression is found.
Q. Will the surgery affect neck movement?
A. Fusion limits motion slightly at the treated level, but most people retain near-normal flexibility. Disc replacement preserves more motion.
Summary and Takeaway
Cervical Degenerative Disc Disease is a natural part of aging that can cause neck pain and nerve irritation. Most cases respond well to non-surgical treatment. When surgery is required, modern techniques such as fusion or disc replacement offer excellent pain relief and restore stability. Maintaining good posture, staying active, and avoiding smoking help slow further degeneration.
Clinical Insight & Recent Findings
A recent network meta-analysis compared different anterior surgical techniques for treating noncontiguous cervical degenerative disc disease (CDDD), including anterior cervical discectomy and fusion (ACDF) with plate fixation or zero-profile spacers, cervical disc arthroplasty (CDA), and hybrid cervical surgery (HCS).
The study analyzed 312 patients across six trials and found that all techniques achieved high fusion success rates, with no cases of pseudoarthrosis and only one reoperation. While functional recovery—measured by the Japanese Orthopedic Association (JOA) and Neck Disability Index (NDI) scores—was similar across all groups, techniques using zero-profile spacers or CDA had significantly fewer postoperative complications, particularly lower rates of dysphagia and adjacent segment degeneration compared to traditional plated ACDF.
These findings suggest that motion-preserving and low-profile implants may reduce soft-tissue irritation and stress on neighboring spinal levels, improving patient comfort and reducing long-term risks. (Study of anterior cervical surgical techniques for noncontiguous cervical degenerative disc disease – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Care is provided by orthopedic spine surgeons or neurosurgeons with experience in cervical reconstruction, along with physical therapists, pain specialists, and rehabilitation teams.
When to See a Specialist?
Seek specialist care if you have:
- Persistent neck or arm pain
- Tingling, numbness, or weakness in the arms or hands
- Difficulty with balance or fine hand movements
When to Go to the Emergency Room?
Go to the ER immediately if you experience:
- Sudden paralysis or severe weakness
- Loss of bladder or bowel control
- High fever or unexplained weight loss with neck pain
What Recovery Really Looks Like?
Mild stiffness and soreness may last several weeks. Gradual stretching, therapy, and good posture restore mobility. Long-term outcomes are excellent when patients remain active and follow rehabilitation plans.
What Happens If You Ignore It?
Untreated spinal cord or nerve compression can cause permanent nerve damage, chronic pain, or muscle weakness. Early treatment prevents these complications.
How to Prevent It?
- Maintain good posture
- Avoid smoking and excessive strain
- Exercise regularly to strengthen neck and shoulder muscles
- Manage chronic illnesses such as diabetes and arthritis
Nutrition and Bone or Joint Health
A balanced diet rich in calcium, vitamin D, and protein supports bone strength. Staying hydrated and avoiding excess caffeine and alcohol protect spinal discs.
Activity and Lifestyle Modifications
Low-impact exercises such as swimming, yoga, and walking maintain flexibility and reduce stiffness. Use ergonomic furniture and proper lifting techniques to protect your neck.
Do you have more questions?
What are the earliest signs of Cervical Degenerative Disc Disease?
The earliest signs often include mild neck pain and stiffness, which may be more noticeable after activities that strain the neck. Some people may experience a slight decrease in neck flexibility.
How does cervical disc degeneration differ from other types of arthritis in the spine?
Cervical disc degeneration primarily involves the breakdown of the intervertebral discs, while other types of arthritis, like osteoarthritis, affect the joints and bone surfaces. Both conditions can coexist, contributing to neck pain and stiffness.
Are there specific activities I should avoid to prevent worsening of CDDD?
Avoid activities that involve heavy lifting, repetitive neck movements, and prolonged periods of poor posture, such as looking down at your phone or computer screen for extended times.
How effective are non-surgical treatments for managing CDDD?
Non-surgical treatments like physical therapy, medications, and lifestyle changes are effective for many people in managing pain and improving function. They can significantly reduce symptoms and delay the need for surgery.
Can physical therapy completely cure CDDD?
Physical therapy cannot cure CDDD but can effectively manage symptoms, improve neck strength and flexibility, and enhance overall function, thus improving quality of life.
Are there any alternative therapies that might help with CDDD?
Alternative therapies such as acupuncture, chiropractic care, and massage therapy can provide symptom relief for some individuals. Always consult with a healthcare provider before starting any alternative treatments.
How do I know if my CDDD is severe enough to consider surgery?
Surgery is considered if conservative treatments fail, symptoms significantly impact your daily life, or if there is evidence of nerve compression causing severe pain, weakness, or loss of function.
What are the risks associated with cervical spine surgery?
Risks include infection, bleeding, nerve damage, spinal cord injury, persistent pain, and complications from anesthesia. Discuss these risks thoroughly with your surgeon.
How long is the recovery period after cervical spine surgery?
Recovery time varies but typically ranges from several weeks to a few months, depending on the type of surgery and individual factors like overall health and adherence to rehabilitation protocols.
Can cervical disc degeneration lead to permanent disability?
While rare, severe cases of CDDD can lead to significant nerve damage and permanent disability if left untreated. Early intervention and appropriate management are crucial.
Is cervical disc replacement surgery better than spinal fusion?
Cervical disc replacement preserves more natural neck motion and may reduce the risk of adjacent segment disease. However, suitability depends on individual factors, and both procedures have their own benefits and risks.
Can wearing a neck brace help with CDDD?
A neck brace can provide short-term relief by limiting motion and allowing the neck muscles to rest. However, long-term use is not recommended as it can weaken neck muscles.
How can I differentiate between neck pain from CDDD and other conditions like a muscle strain?
CDDD-related pain often includes stiffness and radiating pain to the shoulders, arms, or hands. Muscle strain pain is usually localized and may improve with rest and simple treatments.
Is it safe to exercise with CDDD?
Yes, exercise is generally safe and beneficial. Low-impact activities like walking, swimming, and specific stretching and strengthening exercises recommended by a physical therapist can help manage symptoms.
How does smoking affect cervical disc health?
Smoking reduces blood flow to the discs, accelerating degeneration and impairing healing. Quitting smoking can improve overall spine health and reduce pain.
Can cervical degenerative disc disease cause headaches?
Yes, CDDD can cause cervicogenic headaches, which originate from neck issues and can radiate to the back of the head and temples.
Are there specific sleeping positions recommended for those with CDDD?
Sleeping on your back or side with a supportive pillow that keeps your neck in a neutral position is recommended. Avoid sleeping on your stomach as it can strain the neck.
What is the prognosis for someone diagnosed with CDDD?
The prognosis varies. Many individuals manage symptoms well with conservative treatments, while some may require surgical intervention. Early diagnosis and proper management can lead to a good quality of life.
Can stress worsen the symptoms of CDDD?
Yes, stress can increase muscle tension and pain perception, exacerbating symptoms. Stress management techniques like mindfulness and relaxation exercises can be beneficial.
How often should I have follow-up appointments if diagnosed with CDDD?
Follow-up frequency depends on symptom severity and treatment response. Initially, more frequent visits may be necessary, tapering off as symptoms are managed effectively.
Can I use a heating pad or ice pack for pain relief?
Both can be effective. Use a heating pad to relax muscles and improve blood flow or an ice pack to reduce inflammation and numb the area. Use for 15-20 minutes several times a day.
Are there any specific ergonomic adjustments for workstations to help with CDDD?
Ensure your monitor is at eye level, use an ergonomic chair that supports your lower back, keep your feet flat on the floor, and take regular breaks to avoid prolonged neck strain.
Is it normal to feel tired or fatigued with CDDD?
Chronic pain can lead to fatigue. Managing pain effectively, getting adequate rest, and maintaining a healthy lifestyle can help reduce fatigue.
Can CDDD affect my ability to drive?
Severe CDDD can impair neck movement and reaction times, affecting driving ability. If you experience significant symptoms, it’s advisable to consult your doctor about driving safety.

