Lumbar disc replacement surgery is a modern procedure designed to alleviate chronic lower back pain caused by degenerative disc disease by replacing a damaged intervertebral disc with an artificial one. This surgery aims to restore the natural movement of the spine and provide pain relief, offering a potential alternative to traditional lumbar spinal fusion, which can reduce flexibility and cause degeneration of adjacent spinal segments.
How Common It Is and Who Gets It? (Epidemiology)
Low back pain affects a significant portion of the population, with about 70-85% of individuals experiencing this condition at some point in their lives. Degenerative disc disease, which often leads to the need for lumbar disc replacement, is particularly common in adults over 40, especially those with a history of spine problems or injuries.
Why It Happens – Causes (Etiology and Pathophysiology)
The spine is made up of vertebrae, with intervertebral discs acting as shock absorbers between them. Over time, these discs can deteriorate due to age, injury, or wear and tear. The central part of the disc (nucleus pulposus) loses water content and the disc height decreases, leading to conditions like herniation, where the disc material presses against the spinal nerves, causing pain, weakness, and numbness.
An intervertebral disc has two main parts:
- Annulus Fibrosus: The tough, outer layer.
- Nucleus Pulposus: The soft, gel-like center.
With age or injury, these discs can degenerate, leading to conditions such as lumbar degenerative disc disease. As the central nucleus loses water content, the disc height decreases, which can cause the disc to herniate. Herniation occurs when the inner nucleus pushes through the outer layer, potentially compressing nearby nerves and causing pain and other symptoms.
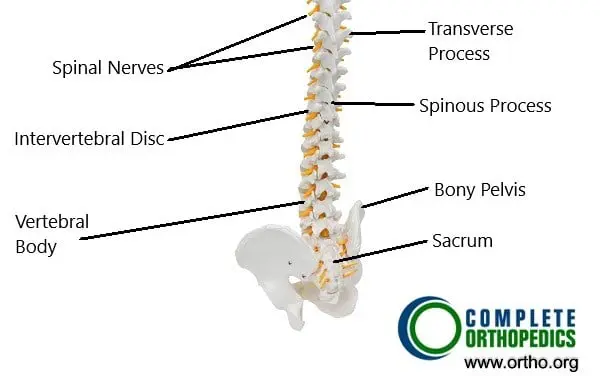
With advancing age, the water content of the central nucleus of the disk decreases. As a result of dehydration, the disc height decreases and the intervertebral disk may herniate through the vertebral canal. The herniated disks may compress the dural sac and the transversing or descending spinal nerves. The compression/irritation of the spinal nerves and the dural sac may lead to symptoms of back pain and radiculopathy.
In the majority of patients, these symptoms are relieved in a period of few weeks with conservative management. Conservative management consists of physical therapy, activity modification, pain medications, heat and cold therapy, epidural/nerve block injections, etc.
How the Body Part Normally Works? (Relevant Anatomy)
The lumbar spine consists of five vertebrae (L1-L5), with discs in between each vertebra. These discs cushion the vertebrae and allow for spinal movement and flexibility. The discs are composed of two parts: the annulus fibrosus (the outer layer) and the nucleus pulposus (the soft, gel-like center). When these discs degenerate or herniate, they can compress spinal nerves, leading to pain and dysfunction.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of degenerative disc disease include:
- Persistent lower back pain, especially when sitting or bending.
- Radiating pain in the legs (sciatica).
- Numbness, tingling, or weakness in the legs.
- Difficulty with bending, twisting, or moving.
How Doctors Find the Problem? (Diagnosis and Imaging)
Doctors diagnose lumbar disc problems through physical exams, reviewing medical history, and imaging tests. MRI or CT scans are typically used to visualize the discs and assess the degree of degeneration or herniation. X-rays may also be used to evaluate the alignment of the spine.
Classification
Lumbar disc problems are typically classified based on the degree of degeneration or herniation:
- Mild: Minor disc degeneration without nerve compression.
- Moderate: Disc bulging or herniation causing some nerve compression.
- Severe: Advanced disc degeneration or herniation with significant nerve damage or compression.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions that might mimic lumbar disc issues include:
- Muscle strain or ligament injury.
- Sciatica from piriformis syndrome.
- Kidney stones or infections.
- Spinal stenosis or spondylolisthesis.
Treatment Options
- Non-Surgical Care: Most people with lumbar disc issues start with conservative treatments like physical therapy, medications (NSAIDs, muscle relaxants), and epidural steroid injections.
- Surgical Care: Surgery is considered for patients who don’t respond to conservative treatments after 6 months. Options include spinal fusion or lumbar disc replacement (LDR).
Recovery and What to Expect After Treatment
- Post-Surgery Recovery: After lumbar disc replacement surgery, most patients stay in the hospital for 2-3 days. Early mobilization is encouraged, and physical therapy begins soon after surgery to restore strength and flexibility. Full recovery may take 6-12 weeks.
- Long-Term Recovery: Most patients experience significant pain relief and can return to normal activities within a few months.
Possible Risks or Side Effects (Complications)
As with any surgery, there are risks, including:
- Infection at the surgical site.
- Nerve damage, leading to weakness or numbness.
- Vascular injury due to proximity to major blood vessels.
- Implant failure or displacement.
- Persistent back pain despite surgery.
Long-Term Outlook (Prognosis)
The prognosis for lumbar disc replacement surgery is generally positive, with most patients experiencing improved mobility and pain relief. However, long-term success depends on factors like patient health, adherence to postoperative care, and the presence of adjacent segment degeneration.
Out-of-Pocket Cost
Medicare
CPT Code 22857 – Lumbar Disc Replacement: $412.08
Under Medicare, 80% of the approved amount for this procedure is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, leaving most patients with little to no out-of-pocket expenses for Medicare-approved lumbar disc replacement procedures. These supplemental plans work directly with Medicare to provide full coverage for the surgery.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare has processed the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or any uncovered charges. Most secondary insurance plans have a modest deductible, typically between $100 and $300, depending on the specific policy and network status.
Workers’ Compensation
If your lumbar disc replacement is required due to a work-related injury, Workers’ Compensation will cover all related medical and surgical costs, including the procedure and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your lumbar disc replacement is related to a motor vehicle accident, No-Fault Insurance will cover the full cost of the surgery. The only possible out-of-pocket expense would be a small deductible depending on your specific policy terms.
Example
Rebecca, a 60-year-old patient with lumbar degenerative disc disease, underwent lumbar disc replacement (CPT 22857) to relieve her chronic back pain. Her estimated Medicare out-of-pocket cost was $412.08. Since Rebecca had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving her with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. How long does recovery from lumbar disc replacement surgery take?
A. Recovery typically takes 3-6 months, with most patients experiencing significant pain relief within a few weeks.
Q. Are there any risks associated with lumbar disc replacement surgery?
A. Risks include infection, nerve damage, vascular injury, and implant failure. However, these complications are rare.
Q. Will I need additional surgery after lumbar disc replacement?
A. Most patients do not need additional surgery, but some may require fusion if the disc replacement fails or if the degeneration progresses.
Summary and Takeaway
Lumbar disc replacement surgery is a promising alternative to spinal fusion for treating degenerative disc disease. It helps preserve spinal motion, reduces pain, and improves function. The procedure offers several benefits over fusion, such as maintaining flexibility and potentially preventing adjacent segment degeneration. However, not all patients are candidates for this surgery, and careful evaluation by a spine specialist is necessary to determine the best course of action.
Clinical Insight & Recent Findings
A recent study conducted a systematic review on the readability of patient education materials (PEMs) for lumbar disc replacement surgery, highlighting that these materials are written well above the recommended 6th-grade reading level.
The analysis found that the average readability score for these PEMs was at a 12th-grade level, far exceeding the American Medical Association’s (AMA) recommended reading level. This suggests that many patients may struggle to comprehend the nature of their condition and treatment.
The study emphasizes the need for revisions to make PEMs more accessible, including simplifying language, reducing sentence length, and incorporating more visual aids to improve patient understanding and outcomes. (“Study on readability of lumbar disc replacement PEMs – see PubMed.”)
Who Performs This Treatment? (Specialists and Team Involved)
Lumbar disc replacement is typically performed by orthopedic spine surgeons or neurosurgeons with specialized training in complex spine surgeries.
When to See a Specialist?
If you experience persistent lower back pain, leg weakness, or numbness, consult a spine specialist to determine if lumbar disc replacement or another treatment is appropriate.
When to Go to the Emergency Room?
Seek emergency care if you experience sudden and severe pain, loss of bladder or bowel control, or new weakness or paralysis in the legs.
What Recovery Really Looks Like?
Recovery from lumbar disc replacement surgery is generally faster than fusion surgery, with patients returning to normal activities within a few weeks and full recovery within 3-6 months.
What Happens If You Ignore It?
Untreated degenerative disc disease can lead to worsening pain, decreased mobility, and permanent nerve damage. Early intervention can prevent further complications and improve long-term outcomes.
How to Prevent It?
Maintaining a healthy weight, staying active, and practicing good posture can help prevent lumbar spine issues. Regular exercise, especially core strengthening, is essential for spinal health.
Nutrition and Bone or Joint Health
A diet rich in calcium and vitamin D supports bone health. Weight-bearing exercises help maintain strong bones and prevent degeneration.
Activity and Lifestyle Modifications
After surgery, patients should avoid heavy lifting, twisting, and bending movements. Continuing physical therapy is essential for a full recovery and to prevent future issues.
Do you have more questions?
Who is a good candidate for lumbar disc replacement surgery?
Good candidates are those with clear disc pathology, not significantly obese, and without inflammatory bone diseases like osteoporosis or rheumatoid arthritis. They should also not have facet joint disease, infections, tumors, or fractures causing their back pain.
How does lumbar disc replacement differ from spinal fusion?
Unlike spinal fusion, which fuses two vertebrae together to eliminate movement, lumbar disc replacement retains the mobility of the spine segment by replacing the damaged disc with an artificial one. This helps maintain natural motion and reduces the risk of degeneration in adjacent segments.
What materials are used in artificial discs?
Artificial discs are typically made from surgical-grade plastic (polyethylene) and metal alloys. The metal parts often cover the surfaces of the adjoining vertebrae, providing stability and durability.
What are the main benefits of lumbar disc replacement surgery?
The main benefits include preserving spinal movement, reducing back pain, and potentially lowering the risk of adjacent segment degeneration compared to spinal fusion.
How long does the surgery take?
The surgery typically takes 2-3 hours, depending on the complexity of the case and the surgeon’s experience.
What are the risks associated with lumbar disc replacement surgery?
Risks include excessive bleeding, damage to blood vessels or nerves, infection, implant failure, and persistent back pain.
What is the recovery time for lumbar disc replacement surgery?
Patients generally stay in the hospital for 2-3 days post-surgery. Full recovery, including a return to normal activities, usually takes several weeks to a few months, with physical therapy playing a crucial role in the rehabilitation process.
How long does the artificial disc last?
Current studies indicate that artificial discs can last 10-15 years or more, but long-term data is still being collected as the procedure is relatively new compared to spinal fusion.
Can a lumbar disc replacement fail?
Yes, like any medical implant, an artificial disc can fail due to factors such as improper placement, wear and tear, or rejection by the body.
What symptoms should prompt me to consider lumbar disc replacement surgery?
Chronic lower back pain not responding to conservative treatments like physical therapy, medications, and injections might prompt consideration for this surgery. Symptoms often include pain radiating down the legs, numbness, and weakness.
How do surgeons determine if a patient is a candidate for this surgery?
Surgeons evaluate medical history, physical examination, imaging studies (like MRI and X-rays), and the response to conservative treatments to determine if a patient is a candidate for lumbar disc replacement.
What is the success rate of lumbar disc replacement surgery?
Success rates are generally high, with many studies showing significant pain relief and improved function. Long-term studies, like the five-year follow-up mentioned, indicate durable benefits with low complication rates.
What should I expect during the recovery period?
Expect a hospital stay of 2-3 days, followed by gradual resumption of activities. Physical therapy will be essential to strengthen your back and improve flexibility. Pain and discomfort are common initially but should decrease over time.
Are there any activities I should avoid post-surgery?
Initially, avoid heavy lifting, bending, and twisting movements. Your surgeon and physical therapist will provide specific guidelines tailored to your recovery progress.
Can I return to work after the surgery?
Many patients return to work within a few weeks, depending on the nature of their job and their recovery progress. Desk jobs may allow an earlier return, while physically demanding jobs may require a longer recovery period.
Will I need physical therapy after the surgery?
Yes, physical therapy is a crucial part of the recovery process, helping to strengthen your back, restore flexibility, and ensure a successful outcome.
Can lumbar disc replacement be performed on more than one disc?
In some cases, multiple discs can be replaced. However, the suitability of multi-level disc replacement depends on individual patient factors and should be discussed with your surgeon.
What are the alternatives to lumbar disc replacement if I am not a candidate?
Alternatives include continued conservative management, spinal fusion surgery, and other less invasive procedures like nerve decompression or spinal injections.
Is lumbar disc replacement covered by insurance?
Coverage varies by insurance provider and policy. It’s essential to check with your insurance company to understand the specifics of your coverage for this procedure.
How do artificial discs compare to natural discs in terms of function?
Artificial discs are designed to mimic the natural disc’s function by allowing motion and providing cushioning between vertebrae. While not identical to natural discs, they offer a similar range of movement and flexibility.
Can I undergo MRI scans after having an artificial disc implanted?
Most modern artificial discs are MRI-compatible. However, it’s essential to inform the radiologist about your implant before undergoing an MRI.
Will I feel the artificial disc in my spine?
Generally, patients do not feel the artificial disc once they have healed. Any initial discomfort typically subsides as the body adjusts to the implant.
What is the long-term outlook for patients with lumbar disc replacement?
The long-term outlook is promising, with many patients experiencing sustained pain relief and improved function. Ongoing research continues to monitor the durability and effectiveness of artificial discs.

