Ossification of posterior longitudinal ligament (OPLL) is a condition affecting the cervical spine. OPLL may lead to compression of the spinal cord and may cause symptoms of cervical myelopathy. Patients with cervical myelopathy present with symptoms of weakness and clumsiness in the hands and difficulty walking.
How Common It Is and Who Gets It? (Epidemiology)
OPLL is most often seen in middle-aged and older adults, particularly in individuals of Asian descent, though it occurs worldwide. The condition tends to develop gradually and may not cause symptoms until the ossified (hardened) ligament begins pressing on the spinal cord. Men are affected slightly more often than women.
Why It Happens – Causes (Etiology and Pathophysiology)
OPLL occurs when a ligament that runs along the back of the spine’s vertebral bodies—called the posterior longitudinal ligament—gradually turns into bone. This thickened, hardened tissue can narrow the spinal canal and compress the spinal cord or nerves.
The exact cause is unknown, but aging, genetics, diabetes, and minor repetitive injuries to the spine may contribute. In some people, the spinal canal is naturally narrow (a condition known as congenital stenosis), making them more likely to develop symptoms if ossification occurs.
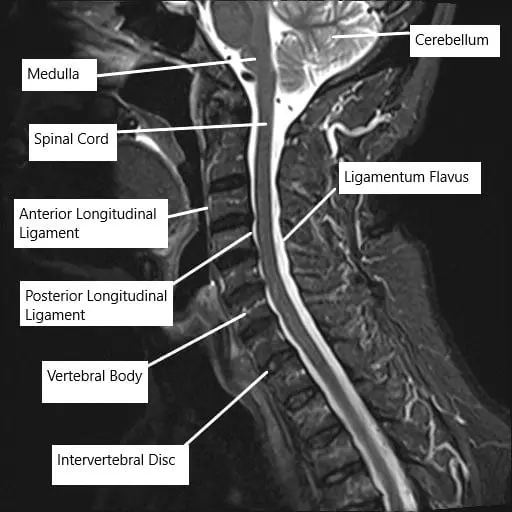
MRI of the cervical spine showing the various ligaments surrounding the spinal cord.
How the Body Part Normally Works? (Relevant Anatomy)
The posterior longitudinal ligament runs along the back surface of the vertebral bodies inside the spinal canal. Its job is to stabilize the spine and limit excessive movement. When the ligament thickens and hardens, it takes up space in the canal, squeezing the spinal cord. This pressure can interrupt signals between the brain and body, leading to numbness, weakness, or coordination problems.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms depend on how much the spinal cord is compressed. Common signs include:
- Neck stiffness or aching
- Numbness or tingling in the hands, arms, or legs
- Weakness or clumsiness of the hands
- Unsteady gait or loss of balance
- Electrical shock-like sensations when bending the neck
- In more severe cases, difficulty controlling bladder or bowel function
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a physical exam to assess strength, sensation, and coordination.
Imaging is crucial to confirm the diagnosis and plan treatment:
- MRI scans show pressure on the spinal cord and detect inflammation or swelling.
- CT scans clearly show the hardened ligament and help classify the type of OPLL.
OPLL is typically divided into four types: segmental, continuous, mixed, and localized (other). Understanding which type a patient has helps surgeons choose the safest approach.
Classification
OPLL is classified based on the shape and distribution of the ossification:
- Segmental: Small, separate areas of bone formation behind individual vertebrae.
- Continuous: A long stretch of bone extending across multiple vertebrae.
- Mixed: Features of both continuous and segmental patterns.
- Localized/Other: Limited to a small area or atypical pattern.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that can mimic OPLL include:
- Cervical spondylotic myelopathy (spinal cord compression from arthritis)
- Herniated cervical discs
- Spinal tumors or infections
- Inflammatory disorders such as ankylosing spondylitis
MRI and CT imaging help rule out these other causes.
Treatment Options
Non-Surgical Care
If symptoms are mild, OPLL may be managed conservatively with:
- Physical therapy and posture correction
- Medications to relieve pain and stiffness
- Regular monitoring with MRI to detect progression
However, once neurological symptoms such as weakness, numbness, or walking imbalance appear, surgery is usually required to prevent worsening.
Surgical Care
Surgery aims to relieve pressure on the spinal cord and stabilize the spine. The approach depends on spinal alignment, location of the ossified ligament, and number of levels involved.
Posterior (Back) Surgery
If the spine retains a normal forward curve (lordosis), decompression through the back—such as laminoplasty or laminectomy and fusion—is preferred. These methods relieve pressure without the risks associated with operating from the front of the neck.
Anterior (Front) Surgery
If the spine has lost its normal curve or is bent forward (kyphosis), surgery from the front may be needed. Procedures such as corpectomy (removal of part of the vertebral body) allow direct removal of the ossified ligament.
Each approach has unique advantages and risks, and the final decision is made based on detailed imaging and patient factors.
Recovery and What to Expect After Treatment
After OPLL surgery, patients typically stay in the hospital for several days. Early movement and physical therapy are encouraged to maintain flexibility and prevent stiffness.
Rehabilitation focuses on:
- Restoring strength and coordination
- Practicing proper neck alignment and movement
- Preventing recurrence through gentle exercise and posture training
Patients are advised to avoid heavy lifting or activities that strain the neck during recovery.
Possible Risks or Side Effects (Complications)
As with any spine surgery, complications can occur but are minimized through careful planning. Potential risks include:
- Infection or bleeding
- Nerve injury or spinal fluid leak
- Difficulty swallowing (after anterior surgery)
- Wound healing issues (especially after prior radiation)
- Hardware failure or need for revision surgery
Elderly patients and those with extensive ossification may have slightly higher complication risks.
Long-Term Outlook (Prognosis)
Surgery for OPLL generally leads to significant improvement in pain, strength, and balance. The degree of recovery depends on how much spinal cord damage occurred before surgery. Most patients report improved quality of life and reduced risk of sudden paralysis after successful decompression and stabilization.
Out-of-Pocket Cost
Medicare
CPT Code 63081 – Anterior Corpectomy: $433.45
CPT Code 63045 – Posterior Decompression (Laminectomy): $319.26
CPT Code 22551 – Anterior Cervical Discectomy and Fusion (ACDF): $417.50
CPT Code 22600 – Posterior Cervical Fusion: $322.92
CPT Code 22842 – Instrumentation (Rods, Screws, Plates – 3–6 Segments): $185.26
Under Medicare, 80% of the approved cost for these spine procedures is covered once your annual deductible is met. Patients are responsible for the remaining 20%. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover this coinsurance, ensuring that most patients have minimal or no out-of-pocket costs for Medicare-approved surgeries. These supplemental policies work directly with Medicare to provide full coverage for multi-level cervical spine decompression and stabilization procedures.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer after Medicare has processed the claim. Once your deductible is satisfied, the secondary plan may cover any remaining coinsurance or balance due. Secondary insurance policies generally include a small deductible ranging from $100 to $300, depending on the specific policy and whether the procedure is performed at an in-network facility.
Workers’ Compensation
If your cervical spine condition or injury requiring decompression or fusion surgery is related to a work-related accident, Workers’ Compensation will cover all medical, surgical, and hospital expenses. This includes anterior and posterior approaches, fusion, and instrumentation, leaving you with no out-of-pocket costs under an approved claim.
No-Fault Insurance
If your cervical spine injury or condition was caused or worsened by a motor vehicle accident, No-Fault Insurance will cover the entire cost of necessary surgical care, including decompression, fusion, and instrumentation. The only potential charge may be a small deductible based on your policy terms.
Example
Laura, a 64-year-old patient with multi-level cervical stenosis, underwent anterior corpectomy (CPT 63081) and posterior fusion with instrumentation (CPT 22600 + 22842) for spinal cord compression. Her Medicare out-of-pocket costs were $433.45, $322.92, and $185.26. Because she had supplemental insurance through Blue Cross Blue Shield, the remaining 20% not covered by Medicare was fully paid, leaving her with no out-of-pocket expenses for her surgery.
Frequently Asked Questions (FAQ)
Q. Is surgery always necessary for OPLL?
A. No. If symptoms are mild and stable, your doctor may recommend monitoring and physical therapy. Surgery is advised if nerve compression worsens.
Q. Which surgery is safer—anterior or posterior?
A. Each approach has its place. Posterior surgery avoids major front-of-neck structures, while anterior surgery allows direct removal of the ossified ligament in certain cases. Your surgeon will determine which is best for your spine alignment and anatomy.
Q. How long does recovery take?
A. Most patients return to light activities within a few weeks and continue improving for several months with therapy.
Q. Can OPLL return after surgery?
A. It’s uncommon, but ossification may slowly progress over time. Regular follow-up imaging helps monitor any changes.
Summary and Takeaway
Ossification of the posterior longitudinal ligament (OPLL) is a condition where a spinal ligament hardens and presses on the spinal cord. When symptoms progress, surgery is the most effective way to relieve pressure and protect nerve function. With careful surgical planning and rehabilitation, most patients experience meaningful pain relief, improved mobility, and long-term stability.
Clinical Insight & Recent Findings
A recent study developed a machine learning model to improve early detection of ossification of the posterior longitudinal ligament (OPLL) during routine health screenings. Researchers analyzed data from 1,442 adults, including 432 confirmed OPLL cases, and used Random Forest–based feature selection to identify 20 key predictors out of 235 variables.
The study found that age, body fat percentage, abdominal circumference, and elevated blood glucose and CA19-9 levels were the strongest risk factors for OPLL. The logistic regression model achieved an accuracy of 65% and an AUROC of 0.69, performing comparably to more complex models while offering greater clinical interpretability. Decision-curve analysis showed that the model could identify one additional true OPLL case per 48 individuals screened while avoiding 38 unnecessary CT scans.
These findings suggest that metabolic and inflammatory factors play central roles in OPLL development and that interpretable machine learning tools can facilitate early diagnosis, reduce false positives, and guide targeted screening strategies. (Study of machine learning–based early detection of OPLL – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is performed by orthopedic spine surgeons or neurosurgeons experienced in complex cervical procedures. The team also includes anesthesiologists, neurophysiologists, and rehabilitation specialists to ensure safe surgery and full recovery.
When to See a Specialist?
You should see a spine specialist if you experience:
- Progressive neck stiffness or pain
- Numbness or weakness in the arms or legs
- Trouble with coordination or balance
- Difficulty controlling bladder or bowel function
When to Go to the Emergency Room?
Go to the ER if you experience:
- Sudden paralysis or severe weakness
- Loss of bladder or bowel control
- New or worsening numbness in the hands or feet
These are signs of spinal cord compression that require urgent care.
What Recovery Really Looks Like?
After surgery, most patients notice gradual improvement in strength and coordination. Neck soreness is normal at first but lessens with time. Physical therapy helps restore mobility and ensures proper spinal alignment during healing.
What Happens If You Ignore It?
Untreated OPLL can lead to progressive spinal cord damage, increasing the risk of paralysis even from minor injury. Early diagnosis and timely treatment are essential for preventing irreversible nerve damage.
How to Prevent It?
While OPLL cannot always be prevented, maintaining a healthy lifestyle and protecting spinal health can help:
- Maintain good posture and neck alignment
- Avoid repetitive strain or high-impact sports
- Keep a healthy weight and manage chronic conditions like diabetes
- Schedule regular checkups if you have a family history of OPLL
Nutrition and Bone or Joint Health
A balanced diet with calcium, vitamin D, and protein supports bone health and recovery after surgery. Avoid smoking and excessive alcohol, as they can weaken bone and delay healing.
Activity and Lifestyle Modifications
After recovery, continue gentle exercises such as walking or swimming. Avoid sudden neck movements and heavy lifting. Good ergonomics at work and home—such as proper desk height and supportive seating—help protect your spine long-term.
Do you have more questions?
What causes OPLL?
The exact cause is unknown, but it is believed to be due to a combination of genetic, hormonal, and environmental factors. There are associations with conditions like diabetes and obesity, and it is more common in East Asian populations
How is OPLL diagnosed?
Diagnosis typically involves a combination of patient history, physical examination, and imaging studies like X-rays, MRI, and CT scans to identify the ossification and assess the extent of spinal cord compression
What are the symptoms of OPLL?
Symptoms include neck pain and stiffness, radiating pain to the shoulders and arms, numbness or tingling in the hands, weakness in the arms and legs, difficulty with coordination and balance, and in severe cases, paralysis or bladder and bowel dysfunction
What non-surgical treatments are available for OPLL?
Non-surgical treatments include pain relievers, anti-inflammatory drugs, muscle relaxants, physical therapy, and lifestyle modifications such as weight management and avoiding activities that exacerbate symptoms
What surgical options are available for treating OPLL?
Surgical options include anterior approaches like ACDF and corpectomy, posterior approaches like laminoplasty and laminectomy, and sometimes combined approaches for more extensive cases
When is surgery recommended for OPLL?
Surgery is recommended when conservative treatments fail to relieve symptoms or if there is significant spinal cord compression that poses a risk of severe neurological damage
What is the recovery process like after OPLL surgery?
Recovery involves rest, medication, and physical therapy. Patients are typically advised to follow a tailored physical therapy program, avoid strain on the neck and spine, and monitor for complications
How successful is OPLL surgery?
Surgical outcomes are generally favorable, with many patients experiencing significant relief from symptoms and improved quality of life. However, some may continue to have residual symptoms or complications
What are the risks associated with OPLL surgery?
Risks include infection, bleeding, spinal fluid leakage, nerve damage, and worsening of neurological symptoms due to spinal cord manipulation
Can OPLL recur after surgery?
While surgery can relieve symptoms and stabilize the spine, there is a risk of recurrence. Ongoing follow-up and possibly further treatment may be necessary
What role does genetics play in OPLL?
Genetics is believed to play a significant role in OPLL, with certain genetic markers associated with an increased risk. This is particularly evident in populations with a higher prevalence of the condition
Are there any lifestyle changes that can help manage OPLL?
Yes, weight management, proper posture, regular exercise, and avoiding activities that strain the neck and spine can help manage OPLL symptoms
How does OPLL progress over time?
OPLL can progress slowly, with gradual worsening of symptoms as the ossification increases and further compresses the spinal cord and nerves. Early intervention can help manage the progression
Can physical therapy help with OPLL?
Yes, physical therapy can help strengthen the neck muscles, improve flexibility, and reduce pain. A tailored physical therapy program is an important part of both conservative treatment and postoperative recovery
Is there a cure for OPLL?
There is no cure for OPLL, but treatments can effectively manage symptoms and prevent further progression. Research into the genetic and molecular mechanisms of OPLL may lead to new therapeutic approaches in the future
What is the difference between laminoplasty and laminectomy?
Laminoplasty involves reshaping or repositioning the lamina to relieve pressure on the spinal cord while maintaining stability. Laminectomy involves removing the lamina to create more space for the spinal cord, often combined with spinal fusion for stability
How long does it take to recover from OPLL surgery?
Recovery time varies depending on the type of surgery and the patient’s overall health, but it typically takes several weeks to months. Full recovery and return to normal activities can take up to a year
What are the potential complications of not treating OPLL?
Untreated OPLL can lead to severe spinal cord compression, resulting in chronic pain, significant neurological deficits, and in extreme cases, paralysis and loss of bladder and bowel control
Can children develop OPLL?
OPLL is rare in children and is more commonly seen in middle-aged and older adults. However, it can occur in younger individuals, particularly those with a genetic predisposition
How does OPLL differ from other spinal conditions like spondylosis or disc herniation?
OPLL involves the ossification of a specific spinal ligament, whereas spondylosis refers to general degenerative changes in the spine, and disc herniation involves the displacement of the intervertebral disc material. Each condition has distinct causes, symptoms, and treatment approaches
Are there any new treatments or research developments for OPLL?
Research is ongoing to better understand the genetic and molecular mechanisms of OPLL, which may lead to new treatments. Advances in imaging and surgical techniques are also improving the diagnosis and management of the condition
What should I do if I suspect I have OPLL?
If you have symptoms suggestive of OPLL, such as neck pain, numbness, or weakness, you should seek medical evaluation. An orthopedic surgeon or spine specialist can perform the necessary diagnostic tests and recommend appropriate treatment
Can OPLL affect other parts of the spine besides the cervical region?
Yes, while OPLL is most commonly found in the cervical spine, it can also occur in the thoracic and lumbar regions, though less frequently
How does the surgical approach for OPLL get decided?
The choice of surgical approach depends on the extent and location of ossification, the patient’s overall health, and the surgeon’s experience. Detailed imaging studies and thorough patient evaluation guide the decision-making process

